This patient care report highlights the initial veterinary nursing interventions provided to a canine patient presenting in respiratory distress secondary to cardiac failure. Nursing considerations including respiratory function, oxygen supplementation and patient monitoring will be discussed below.
Signalment
- Species: Canine
- Name: Roxy
- Breed: Jack Russell Terrier
- Age: 12 years
- Gender: Female neutered
- Weight: 5.45 kg
History and physical examination
Roxy had a chronic history of mitral valve disease, which had progressed to heart failure 18 months prior to presentation at the author's clinic. There had been an initial response to medical management; however, Roxy then developed dyspnoea, 2 days prior to referral. The patient was severely dyspnoeic on presentation and as such physical examination and diagnostic investigations were limited to non-invasive low-stress techniques (Tseng and Waddell, 2000). Roxy had marked inspiratory effort with a rate of 84 breaths per minute. Thoracic auscultation revealed bilateral crackles — worse over the right hemi-thorax. She was also tachycardic with a regular rhythm and a heart rate of 140 beats per minute. All other physical examination parameters were within normal limits.
Diagnosis and treatment
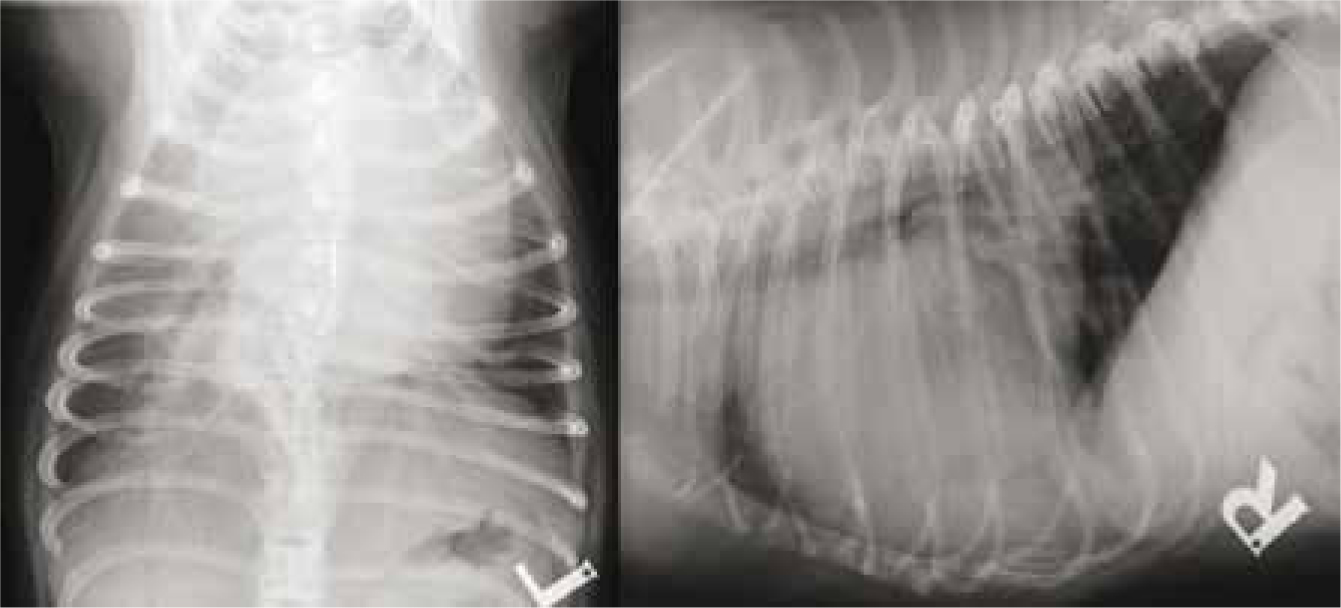
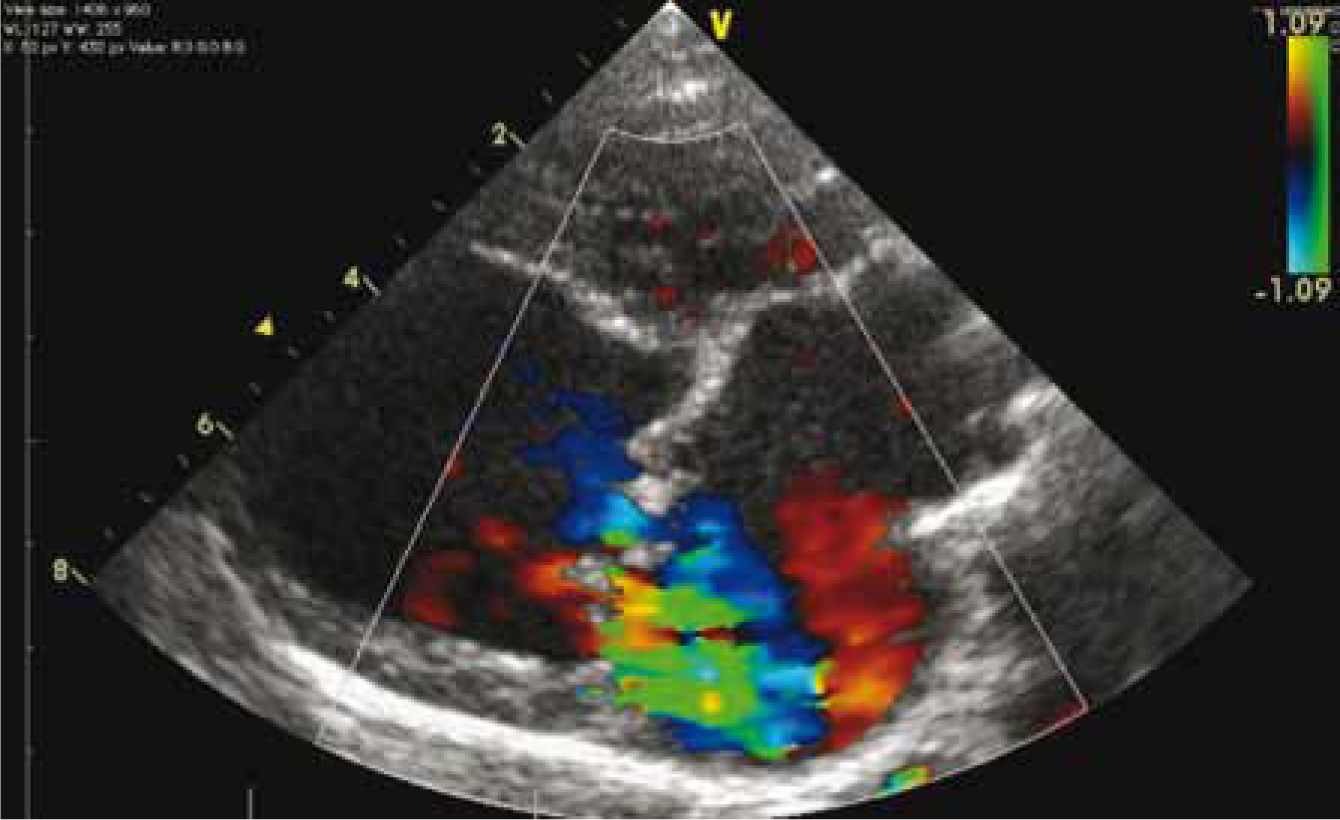
Thoracic radiographs revealed cardiomegaly and an alveolar pattern consistent with pulmonary oedema (Figure 1). Echocardiography highlighted severe mitral valve regurgitation (Figure 2), moderate tricuspid valve regurgitation, severe left atrial and ventricular enlargement (Figure 3) and moderate pulmonary hypertension. A diagnosis of severe mitral valve disease and congestive heart failure (CHF) resulting in severe pulmonary oedema was made and treatment initiated.

On admission, oxygen supplementation was provided via flow-by and an intravenous catheter placed. Roxy was then transferred to an oxygen cage and boluses of furosemide (1–4 mg/kg) administered according to the patient's response to therapy, as noted by monitoring of respiratory parameters. Furosemide is a potent diuretic that is frequently used to treat cardiogenic pulmonary oedema, with the resultant effect being a reduction in intravascular volume and cardiac preload pressures (Erling and Mazzaferro, 2008). It has been suggested that its effectiveness may be improved by administration as a constant rate infusion (CRI), as opposed to boluses (Erling and Mazzaferro, 2008), leading to greater diuresis. Dobutamine, a positive inotrope, was administered as a CRI to increase cardiac contractility leading to a net increase in cardiac output (Erling and Mazzaferro, 2008); its use is normally reserved for patients with severe decompensated CHF due to its ability to ‘increase myocardial contractility without increasing cardiac rate and myocardial oxygen demand’ (Erling and Mazzaferro, 2008). Pimobendan was utilised to improve cardiac efficiency through alteration of the hearts sensitivity to calcium (Erling and Mazzaferro, 2008). Spironolactone was continued, from previous treatment, to assist in diuresis while sparing potassium (Erling and Mazzaferro, 2008). An angiotensinconverting enzyme inhibitor, benazepril, was also continued. Benazepril inhibits the formation of angiotensin II, as part of the renin-angiotensin-aldoster-one system, resulting in venous and arterial dilation as well as a reduction in sodium and water retention, while inhibiting myocardial fibrosis (Pace, 2011). Despite aggressive therapy with the above agents, Roxy's respiratory function did not improve, so a CRI of sodium nitroprusside was added to her treatment plan. Sodium nitroprusside is a venous and arterial vasodilator that can be utilised short term in cases with refractory pulmonary oedema to decrease systemic and pulmonary vascular resistance (Erling and Mazzaferro, 2008); however, care must be taken with its use as it may result in significant hypotension (Sumner and Rozanski, 2013).
Nursing considerations
Patients presenting with CHF and cardiogenic pulmonary oedema require intensive monitoring, in which nursing staff will be significantly involved. Knowledge of the common medications utilised in these cases, and their effects on patient physiology, is imperative to ensure any rapid changes that may be detrimental to the patient, such as hypotension, are observed and appropriate therapy instigated. Monitoring and nursing interventions should be tailored to the requirements of the individual patient based on their abilities and designated treatment plan. The most significant nursing interventions, based on Roxy's individual requirements, were oxygen therapy and monitoring of respiratory and cardiovascular function. Other considerations include monitoring of fluid input and urine output. These will be discussed below.
Respiratory function and oxygen supplementation
Cardiogenic pulmonary oedema may result in a ventilation/perfusion mismatch leading to arterial hypoxaemia (Erling and Mazzaferro, 2008). Therefore, it is essential to provide oxygen supplementation to these patients to reduce arterial hypoxaemia and decrease myocardial workload (Erling and Mazzaferro, 2008). There are several methods of oxygen supplementation that may be employed, each with advantages and disadvantages of use; these include flow by oxygen, facemask, nasal prongs, nasal catheters, oxygen hoods or tents and oxygen cages (Tseng and Waddell, 2000; Erling and Mazzaferro, 2008; Sumner and Rozanski, 2013). Flow-by oxygen therapy was provided to Roxy on initial presentation to support her during the placement of an intravenous catheter. Although flowby does not yield as high a fractional inspired oxygen (FiO2) concentration as alternative methods (Sumner and Rozanski, 2013), it can be an effective means of providing short-term oxygen supplementation during procedures such as intravenous cannulation, in a manner that reduces patient stress and the risk of mortality (Pace, 2011). The patient was then transferred to an oxygen cage; this allowed non-invasive supplementation with a higher FiO2 concentration, and is considered as an ideal method of oxygen therapy in stressed animals (Tseng and Waddell, 2000). However, the use of an oxygen cage has the disadvantage of a rapid reduction in FiO2 concentration each time the kennel is opened for patient examination and nursing interventions, which may be detrimental (Tseng and Waddell, 2000; Rozanski and Chan, 2005). Nasal prongs and nasal catheters may have also been considered for longer-term therapy in this patient; however, nasal prongs may be more ideally suited to recumbent patients and nasal catheters for larger breed dogs (Tseng and Waddell, 2000). Conversely, both methods have the advantage of constant access to the patient for nursing interventions and physical examination without compromising oxygen supplementation (Tseng and Waddell, 2000). Despite the various options available for oxygen therapy, the use of an oxygen cage may be considered the most appropriate in this case, as it allowed patient movement and observation without causing undue stress, which may be fatal in respiratory-distressed patients (Erling and Mazzaferro, 2008). Its use does, however, result in limitations in monitoring and nursing interventions and as such a monitoring plan incorporating this factor should be constructed.
Arterial blood gas versus pulse oximetry
Cellular oxygen delivery is dependent on several factors, these include: haemoglobin concentration, haemoglobin oxygen saturation, gas exchange within the lung and cardiac output (Tseng and Waddell, 2000; Sumner and Rozanski, 2013). Supplementation with oxygen should improve both the dissolved oxygen content of the blood as well as the haemoglobinoxygen saturation (Guyton, 1991). The effectiveness of oxygen therapy can be measured through arterial blood gas analysis or pulse oximetry (Tseng and Waddell, 2000; Sumner and Rozanski, 2013). Arterial blood gas analysis is considered the gold standard method of assessing respiratory function as it allows assessment of both oxygenation and ventilation (Sumner and Rozanski, 2013). However, samples may be difficult to obtain due to technicality and patient status, especially those in respiratory distress (Sumner and Rozanski, 2013). Arterial catheters are available for placement in patients requiring consecutive samples for analysis, or direct blood pressure monitoring, removing the stress that may be involved in repeated sampling (Tseng and Waddell, 2000); however, their placement may be contraindicated in patients with respiratory compromise as stress should be minimised to reduce the risk of sudden respiratory arrest (Pace, 2011). It must also be noted that the use of arterial catheters should be limited to clinics in which 24 hour monitoring is available, due to the risk of significant haemorrhage from patient interference or dislodgement (Tseng and Waddell, 2000). Pulse oximetry may be used as a non-invasive method to assess oxygenation through haemoglobin saturation (Sumner and Rozanski, 2013); however, it can be prone to inaccuracies (Hopper and Powell, 2013) and as such, measurements should be checked through measurement of heart rate and comparison with that displayed by the monitor as well as judgement of trace quality (Hackett, 2002; Erling and Mazzaferro, 2008). Neither method was utilised in Roxy's care owing to the oxygen supplementation method employed. Both techniques would require either removal from the cage for arterial sampling or consecutive opening of the kennel door for probe placement, resulting in a reduction in FiO2 concentration, as discussed above, and as such may have detrimental effects on the patient. Sumner and Rozanski (2013) advise that monitoring of basic parameters should be performed and any further tests only performed when necessary, to ensure patients in respiratory distress are not removed from oxygen therapy for non-essential diagnostic test and procedures (Tseng and Wadddell, 2000).
Patient monitoring
Monitoring of patients with CHF and cardiogenic pulmonary oedema is essential and may be labour intensive (Pace, 2011). While monitoring is of paramount importance, it must never compromise the patient (Pace, 2011; Erling and Mazzaferro, 2008) and as such any monitoring techniques employed must be performed in a manner that reduces stress to the patient, which could ultimately lead to decompensation and arrest (Tseng and Waddell, 2000). Monitoring through serial physical examinations, pulse oximetry, blood gas analysis and blood pressure measurement is ideal (Tseng and Waddell, 2000; Erling and Mazzaferro, 2008); however, it is acknowledged by Pace (2011) that anxious patients may only tolerate monitoring of respiratory rate and effort from a distance. The patient's monitoring plan should be constructed after consideration of the pathophysiological effects that any pharmaceuticals may have, with some patients requiring constant observation of electrocardiogram (ECG) and direct arterial blood pressure (Erling and Mazzaferro, 2008; Pace, 2011; DeFrancesco, 2013; Sumner and Rozanski, 2013). When producing Roxy's monitoring plan, consideration was given to the medications administered, the oxygen supplementation method employed and her tolerance of interventions. The resultant plan involved constant ECG monitoring, due to the risks of cardiac arrhythmias associated with dobutamine administration (Erling and Mazzaferro, 2008; Pace, 2011), constant indirect oscillometric blood pressure measurement, due to the significant risk of hypotension with sodium nitroprusside administration (DeFrancesco, 2013), and hourly measurements of heart rate, respiratory rate and effort, to assess response to drug therapy. Pulse oximetry and arterial blood gas analysis were omitted due to the critical nature of the patient and the risk of stress-induced arrest, as well as low patient tolerance of the pulse oximeter probe, necessitating frequent opening of the patient's kennel, reducing oxygen delivery to the patient.
Frequent monitoring of electrolyte levels and renal parameters were also necessary, as excessive use of diuretics may induce electrolyte disturbances, such as hypokalaemia, or azotaemia (Sumner and Rozanski, 2013). Administration of dobutamine, as in Roxy's treatment plan, can exacerbate this through increased uptake of potassium into cells (Pace, 2011). As advised by Erling and Mazzaferro (2008), daily biochemical analysis was performed to ensure any disturbances were identified and treatment instigated immediately.
Urine output should be monitored to ensure efficacy of diuretic therapy, which aims to reduce intravascular volume through diuresis (Sumner and Rozanski, 2013). This may be performed through collecting urine voided, placement of an indwelling urinary catheter with a closed collection system, or weighing of bedding before and after voidance in the kennel (Erling and Mazzaferro, 2008). Due to the critical state of the patient and the requirement for strict cage rest (DeFrancesco, 2013), the patient was not permitted to walk outside and as such voided in her kennel. Her bedding involved an under layer of incontinence pads and a commercial veterinary bed, which were weighed prior to placement in her kennel. After voiding, these items were re-weighed and the difference in value taken as the volume passed, following the assumption that 1 ml of water was equivalent to 1 g and as such 1 ml of urine (Erling and Mazzaferro, 2013). This method was utilised to reduce patient stress as advised by DeFrancesco (2013).
Direct versus indirect blood pressure measurement
Roxy's blood pressure was monitored using an indirect oscillometric monitor, as this enabled measurement without patient handling and thus reduced stress. Direct blood pressure measurement is considered as the gold standard method in veterinary medicine (Clapham, 2011) and should ideally be used in patients receiving sodium nitroprusside (DeFrancesco, 2013). Conversely, its use necessitates the placement of an arterial catheter, which may not be possible in patients with CHF and respiratory compromise (Rozanski and Chan, 2005). Indirect Doppler and oscillometric methods have been found to underestimate blood pressure readings in comparison to direct methods (Love and Harvey, 2006). Further, oscillometric methods may be unreliable at hypotensive states, with the Doppler method being more successful (Love and Harvey, 2006). As hypotension was the main concern with Roxy's care, direct arterial blood pressure measurement may have been more ideal, however, the oscillometric method may be considered more beneficial than alternative methods due to reduced patient handling and stress, and any measurements of concern checked with an alternative method.
Patient outcome
Roxy's condition improved significantly following intensive nursing care and management with a resultant normalisation of her respiratory function. She was discharged several days after presentation with an alteration to her long-term cardiac treatment plan, which included a change from frusemide to torasemide and the addition of amlodipine to reduce vascular resistance and mitral valve regurgitation.
Conclusion and recommendations for future practice
Patients with CHF presenting in respiratory distress may prove a challenge to nurse and construct a monitoring plan for. Although some methods of oxygen supplementation and patient monitoring may be perceived as more ideal, the individual patient and circumstances must be considered prior to instigation, as the ‘gold standard’ techniques may not be as beneficial as initially thought. Patient health should not be compromised in order to obtain non-essential information. Instead, basic parameter monitoring should be considered as essential, followed by any other techniques that the patient will tolerate.
It is imperative that nurses have an underlying knowledge of the patient's disease process and the pathophysiological effects of any drug therapy, as well as the individual requirements and tolerance of the patient under their care before instigating any nursing interventions, so the most appropriate plan for the individual patient can be devised.
Key Points
- Specific nursing interventions for this condition include oxygen therapy, monitoring of respiratory and cardiovascular function, and monitoring fluid input and output.
- Stress should be minimised for patients in congestive heart failure and respiratory distress to reduce the risk of decompensation and possible arrest.
- The pathophysiological effects of any pharmaceuticals administered should be considered when devising a patient care plan.


