The patient was referred to the hospital for bilateral cataracts 6 months after being diagnosed with diabetes mellitus (DM). The patient was fed a raw food diet (VOM, 2018) three times daily (TID) at home, a diet that consisted of equal or more fat than protein content. This patient was fairly controlled with insulin (Caninsulin® Vet 40IU/ml) 5 IU twice daily (BID) at home where the owners monitored his blood glucose several times a day. His blood glucose normally stayed within 7–15 mmol/litre (ideal blood glucose 4.4–6.6). It was decided to do a phacoemulsification on the left eye to recover partial vision and increase patient welfare.
Signalment
Species: Canine
Breed: Miniature Schnauzer
Age: 8 years 8 months
Sex: Male entire
Weight: 7.3 kg
American Society of Anesthesiologists (ASA) Physical Status Scale: Class III (Severe systemic disease present).
Pre-operative assessment
It is recommended to perform an electroretinogram (ERG) prior to phacoemulsification surgery to rule out general retinal disease (Kelawala and Patil, 2016) as a patient with retinal disease would not regain eyesight through phacoemulsification. The patient had a successful ERG, which meant that this type of surgery would benefit him.
It is not advisable to put unstable diabetic patients under general anaesthesia due to the increased mortality and complication risk (Monticelli et al, 2018). However as the patient was fairly managed, class III ASA status was assigned to this patient (AVTAA, 2018), which means that there was a severe systemic disease present and consequently a higher risk of anaesthetic complications. Specifically risks to this case included: hypo- or hyperglycaemia which in turn would affect acid–base, heart rhythm, ventilation and intraocular pressure (IOP). Therefore, haematology and biochemistry were performed to tailor the patient's anaesthetic protocol and evaluate potential risks. Most parameters were within normal limits aside from: a mildly elevated fructosamine 407 μMol/litre (200–400), increased cholesterol 10.84 mmol/litre (3.5–9) and a decreased creatinine 40 μmol/litre (44–132), which is a result of the patient's DM. Marked increase in alanine aminotransferase (ALAT) 2.19 μKAT/litre (0–1.2), and mildly increased bile acids 22.3 μMol/litre (0–20) could possibly be a result of the patient's diet, however liver damage could not be excluded as a differential.
A routine physical examination was performed and the patient was deemed stable and healthy, and able to proceed with general anaesthesia and surgery.
Pre-anaesthetic management
The patient received topical diclofenac (Voltaren Ophtha 1 mg/ml) BID in the left eye (OS), starting 3 days before planned surgery. On the day of surgery, one drop of diclofenac and one drop of chloramphenicol (Kloramfenikol Santen 5 mg/ml) OS, were given at 10 minute intervals at 6, 7, 8, and 9 am. This was to ensure maximum mydriasis prior to general anaesthesia, which is desirable as it is difficult to achieve this after induction (Gross et al, 2015).
The patient had half a portion of breakfast and half the dose of insulin at 6 am at home on the day of surgery. A 22 G intravenous catheter was placed in his left saphenous vein and blood glucose (19 mmol/litre) was measured on admittance. Anaesthesia and surgery results in a so-called stress response, which is impossible to avoid in diabetic patients; this stress response results in an increase in blood glucose due to several catabolic hormones (De Vries, 2011). The stress response could explain the patient's hyperglycaemia on admission, however as he received a half dose of insulin 2 hours prior, it could be argued that the insulin had only then begun its effect. Caninsulin® (MSD Animal Health) reaches maximum effect 7 to 12 hours post injection (Caninsulin®, 2015), which would have been in recovery, therefore no intervention was carried out, especially as mild hyperglycaemia is preferable to hypoglycaemia under general anaesthesia (AAHA, 2018). The increase in blood glucose could also be justified by the breakfast eaten 2 hours prior to admittance. As recommended by De Vries (2011) and Levensaler (2014) DM patients should be the first to be anaesthetised in the day. This recommendation was followed so that the patient's normal feeding and insulin routines would not be disrupted, aiding in a quicker recovery. Therefore the patient was admitted at 8 am in the morning and induced by 9 am. It is also encouraged to anaesthetise DM patients first in the morning as if there are complications associated with the disease there are more staff and resources available to help in an emergency.
Preparation and premedication
As part of the daily routine and preparation for this surgery an anaesthetic machine check was carried out in the induction suite and in the operating theatre (Table 1). All drugs and constant rate infusions (CRIs) were drawn up, prepared and labelled to minimise confusion. A selection of endotracheal tubes were prepared together with a cuff syringe, ties and an appropriate sized laryngoscope. Emergency drugs were stored nearby for if needed.
Table 1. Anaesthesia machine check
| Chose |
|---|
|
| Check |
|
| Leak test |
|
If using a ventilator, check the function of this one too. Turn on patient monitor, adjust alarm settings and you're ready to go!
It is advisable to avoid alpha-2 agonists such as dexmedetomidine as premedication for phacoemulsification due to the increased risk of nausea and the resultant increase in IOP (Thompson et al, 2007). Ideally a low-normal IOP (dog <10–26 mmHg) is desirable for ocular surgery as high IOP increases the risk of globe rupture (Gross et al, 2015). Alpha-2 agonists are also avoided in diabetic patients as they can cause an increased blood glucose concentration (Levensaler, 2014; Monticelli et al, 2018). The patient was therefore premedicated with 0.4 mg/kg methadone (Synthadon Vet 10 mg/ml, Virbac) intravenously (IV); as the procedure is anticipated to be painful, 0.1 mg/kg metacam (Metacam® 5 mg/ml, Boehringer Ingelheim) was administered subcutaneously as pre-emptive analgesia, and 15 mg/kg amoxicillin (Curamox Vet 150 mg/ml, Boehringer Ingelheim) subcutaneously due to the increased risk of infection in diabetic patients, especially if hyperglycaemia is detected before induction (Robertshaw and Hall, 2006). The sedative agent used for this anaesthetic was a benzodiazepine used as co-induction.
Induction
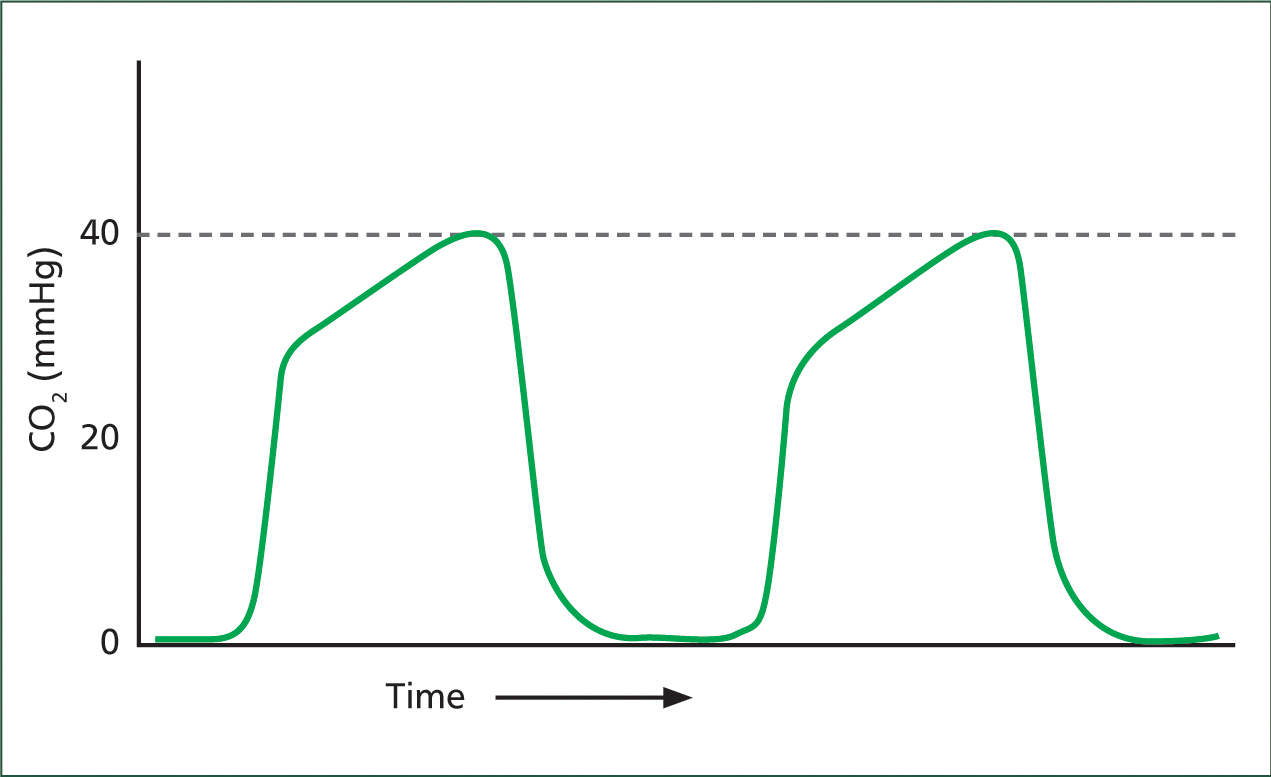
As coughing or sneezing increases IOP it is favourable to induce these patients deeper than usual so that intubation is less irritant. The patient was anaesthetised with 6 mg/kg propofol (Propolid 10 mg/ml, Frensius Kabi) IV and 0.35 mg/kg midazolam IV (Midazolam 5 mg/ml, Hameln Pharmaceutics) as co-induction and intubated with a size six endotracheal tube (ETT) that was secured and tied around the patient's mandible so that it would not interfere with the procedure. Ideally guarded ETT are preferred when performing phacoemulsification surgery due to the unusual head positioning that could otherwise kink the ETT and cause an airway block (Gross et al, 2015). This type of ETT was not available at the time of surgery and therefore it was important to closely monitor capnograph curves for any potential ‘shark fin’ curves indicating an obstructed airway (Figure 1). Once induced, another 22 G intravenous catheter was placed in the patient's right metatarsal vein, the sole purpose of which was to monitor blood glucose during the anaesthetic. Patches over the tibial nerve and over the deep peroneal nerve on the right leg were clipped for the train-of-four monitor (TOF-Watch®, Bluestar Enterprises, Inc) and two electrode pads were placed on the clipped areas.
According to Oliver et al (2010) the biggest complication in anaesthetised dogs undergoing phacoemulsification is hypotension, it was therefor vital to maintain intravascular volume and normotension under anaesthesia, a crystalloid fluid (Ringer-Acetat, Baxter Viaflo) was started at 5 ml/kg/hour intravenously. The fluid rate was decreased by 25% each hour if the patient stayed normotensive and until a maintenance rate was achieved. Hypotension is defined as mean arterial pressure <60 mmHg, fortunately the patient stayed normotensive throughout the anaesthetic period.
Peri-anaesthetic management
A small circle system was used to deliver oxygen, medical air and volatile gases; in this case the patient was maintained on 2.6% sevoflurane (Sevoflo, Orion Pharma) in 0.3 litres/minute fresh gas. A small circle system benefits smaller patients by enabling low gas flow anaesthesia that prevents heat and moisture loss (Hughes, 2007). Capnography, electrocardiogram (ECG), rectal temperature, oscillometric blood pressure and pulse oximeter was used to constantly monitor the patient during the procedure, these parameters were recorded every 15 minutes. Ideally, all monitoring should be kept to the caudal end of the patient, as there is limited access to the cranial end due to the nature of this surgery. Blood glucose was obtained and monitored with a G-Pet Plus+ handheld monitor every 30 minutes if stable and every 15 minutes if a fast shifting trend was seen. The patient stayed between 16.7–19.0 mmol/litre during the procedure and no glucose supplementation was needed.
Preferably, an arterial catheter for invasive blood pressure would have been ideal (Durham, 2005), but due to the limited area in the hind limbs it was accepted to attach an oscillometric blood pressure machine to the base of the tail and measurements were taken manually every 5 minutes. Some (Lavensaler, 2014) may argue that oscillometric blood pressure easurement is best used in patients >10 kg, however newer articles (Sierra and Savino, 2015) argue that oscillometric blood pressure is less accurate in patients <5 kg. It has been found that oscillometric monitoring correlates with Doppler ultrasonic monitoring (Haberman et al, 2006) and is an accurate way of detecting hypotension in anaesthetised dogs (Oliver et al, 2010).
The TOF-Watch® nerve simulator (Figure 2) was attached to the electrode pads on the right leg and the acceleration-sensitive crystal was taped to the dorsal aspect of the right metatarsal (Figure 3). It is vital to mechanically ventilate patients for phacoemulsification as they receive neuromuscular blocking agents (NMBA), these relax the patient's muscles, including its respiratory muscles. Pressure control ventilation was maintained around 6–8 cm water with a positive end-expiration pressure of 3 cm water. Once the patient was positioned and all monitoring was attached half dose of a NMBA starting bolus of 0.1 mg/kg vecuronium (Vecuronuim 10 mg powder for injection, Inresa) was injected slowly IV, 2–3 minutes later a TOF measurment showed a ratio of 43%. It was decided to continue injecting the rest of the starting bolus of the NMBA as the patient was not fully relaxed and then start the 0.1 mg/kg/hour vecuronium CRI. After another couple of minutes, the TOF-watch® displayed a count rather than ratio, which means the neuromuscular block was intense (TOF-Watch®, 2007, Martin-Flores et al, 2012). The surgeon was happy with the relaxed, centred eyeball and it was decided to begin with the surgery.
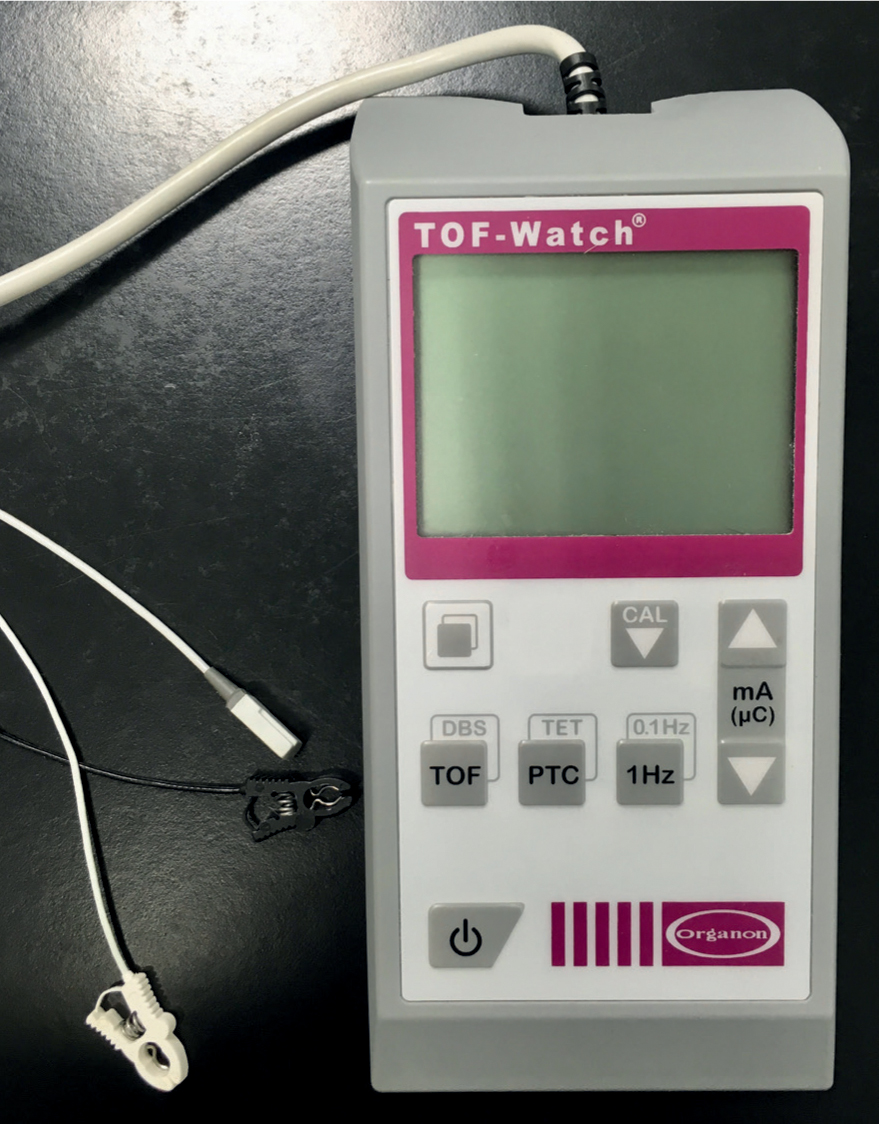

As the duration of action of vecuronium is 20–30 minutes (Ramsey, 2011) the CRI was stopped when the phacoemulsification was accomplished and the surgeon only had approximately 10 minutes left to complete the surgery. When the surgery was complete, the sevoflurane was lowered to 1% and the TOF-watch® evoked a ratio of 64%, at this point the vecuronium was reversed with 0.1 mg/kg neostigmine (Robinul-Neostigmine 0.5 mg/ml+2.5 mg/ml, Meda). The sevoflurane was turned off and the fresh gas flow increased to flush out the volatile agent in the system. Once the patient showed signs of a lighter anaesthetic plane, the ventilator was turned off, allowing the patient to breathe on its own. As the patient was starting to hyperventilate while still intubated and not fully awake, excitation on recovery was anticipated and 0.1 mg/kg midazolam IV was administered to enable a smooth recovery, especially as vocalisation etc. is associated with an increase in IOP (Gross et al, 2015). A buster collar was put on the patient at this point to protect the eye, this is very important as self-inflicted injuries are common and happen quickly. The patient was shortly after extubated once the laryngeal reflex was present.
Vecuronium is metabolised in the liver (Ramsey, 2011) and if liver disease is present, atracurium is recommended instead because it is suitable for use in patients with hepatic and kidney disease (Gross et al, 2015). It could be argued that the patient described above would have benefited from atracurium instead of vecuronium, however vecuronium was the only NMBA available at the hospital at that time.
Ocular reflex (OCR) is a trigeminovagal reflex that is stimulated by the pressure of the eye globe. It is a possibility with any ocular surgery to stimulate this and it is important for the anaesthetic nurse to recognise this stimuli. OCR manifests as: cardiac arrhythmias; bradycardia; nodal rhythms; ectopic beats; ventricular fibrillation; and asystole (Thompson, 2007). No signs of OCR were seen during the procedure, however if noticed it is important to communicate this promptly to the surgeon.
Post-anaesthetic management
The recovery period is where most incidences of deaths have been reported (Crompton and Hill, 2011), so it was important to monitor this high-risk patient frequently during the recovery period. The patient was recovered in the hospital's intensive care unit (ICU) for two main reasons: one was that the patient had DM and needed regular monitoring of blood glucose; and the other was because of the administration of NMBA intra-operatively and midazolam on recovery, which increases the risk of post anaesthetic complication.
Even though the patient was on an electrical heat pad (HotDog®, Augustine Temperature Management) throughout the whole anaesthetic time and covered in a blanket, his rectal temperature decreased to 36.3°C on recovery. Shivering in recovery is linked to an increase in oxygen demand by up to 300% (Crompton and Hill, 2011), hence why the patient was actively warmed and received an infrared heat lamp. A HotDog® was considered but as the patient was moving frequently on recovery, the activation sensor was deactivated and the heat turned off. The disadvantage of using a heat lamp on recovery post phacoemulsification is the patient's increased light sensitivity; human studies have reported similar consequences and human patients are therefore asked to wear sunglasses post surgery (Culross, 2019). Similar recovery equipment is not to the author's knowledge described in veterinary medicine. In hindsight, an electrical forced air warmer such as a Bair Hugger™ (3M) could have been beneficial to reach normothermia instead of the heat lamp, but this equipment was not available at the given time. The patient's temperature was monitored every 30 minutes until normothermia was achieved. Heart- and respiratory rate, and mucous membranes were also monitored frequently to detect any early anaesthetic complications specifically regarding ventilation and the patient's disease. The patient's blood glucose was obtained once more in recovery and once before his evening insulin dose. Both measurements were within the patient's normal blood glucose readings.
It is of great importance to return a diabetic patient to normal routine after surgery (Robertshaw and Hall, 2006) therefore AAHA (2018) recommends to offer small food portions as soon as possible. The patient was offered a small meal of his own diet brought from home 30 minutes into recovery, while sitting up in sternal. Diabetic patients benefit significantly if offered familiar foods (Lumbis, 2012), this patient gladly ate his prepared meal from home if hand-fed by the nurses. Fluid therapy was discontinued since the patient was eating and drinking on his own, however if this had not been the case, fluid therapy would have been continued on a maintenance rate of 2 ml/kg/hour.
As mentioned earlier vocalisation and stress are major factors of an increase in IOP which is undesirable, therefore 0.01 mg/kg acepromazine (dilute Plegecil 2 mg/ml, Pharmaxim) was instructed to be given IV if the patient was agitated. The patient received two doses of 0.2 mg/kg methadone (Synthadon Vet 10 mg/ml) IV every 6 hours post-operatively, this was discontinued the following day as phacoemulsification surgeries are associated with mild pain (Assam et al, 2018). Topical eye drops diclofenac (Voltaren Ophtha 1 mg/ml, Laboratoires Théa) and chloramphenicol (Kloramfenikol 5 mg/ml, Santen) OS was continued post-operatively as analgesic and antibiotic treatment.
Conclusion
Even though phacoemulsification is a specialist procedure that requires specialist equipment and complex anaesthesia protocols, more and more veterinary professionals face diabetic patients and encounter the consequences of the disease, such as impaired vision. It is, therefore, impossible to avoid diabetic patients and thus important to be comfortable anaesthetising these patients. Preparing, anticipating and planning these anaesthetics are crucial for patient outcome. The author believes the important aspects of anaesthetising a diabetic dog for phacoemulsification has been discussed, including pre, peri and post anaesthesia.
KEY POINTS
- Mechanical ventilation is vital during phacoemulsification due to neuromuscular blocking agents (NMBAs). Correct ventilator settings to minimise risk of complications.
- Blood glucose monitoring is required pre-, peri-, and post-anaesthesia to recognise hypo-, or marked hyperglycaemia resulting in a dangerous ketoacidosis that is difficult to recognise under general anaesthesia.
- Anaesthetic monitoring is required, such as temperature probe and blood pressure monitoring, and intravenous access should be kept to the caudal end of the patient.
- Train-of-four (TOF) monitoring ensures satisfactory levels of neuromuscular blockage and successful surgery.
- Smooth and quick recovery is vital to ensure a short stay in-hospital.


