Species: canine
Breed: outcome.
Age: 9 years
Sex: male (neutered)
Weight: 5.4 kg
History
The patient was presented to the surgery with a 3-day history of a corneal ulcer in his left eye. His owners reported him to be inappetant, depressed and lethargic.
Assessment and initial management
On examination the patient was very depressed and lethargic and there was marked blepharospasm of the left eye (Figure 1). The patient's temperature, pulse and respiration were all within normal limits.

Topical local anaesthetic proxymetacaine (Minims proxymetacaine) was applied and ophthalmic examination revealed a desmetocoele on his left cornea with severe uveitis and corneal oedema (Figure 2). Visible exudates of red blood cells (hyphaema) and white blood cells (hypopyon) within the anterior chamber were present. His intraocular pressure (IOP) was normal.

A descemetocoele is a true ophthalmic emergency. It is a deep corneal lesion in which the corneal epithelium and stroma are completely destroyed, leaving a lesion lined only by Descemet's membrane and corneal endothelium (Featherstone and Stanley, 2002).
A conjunctival graft was necessary to prevent the eye from rupturing.
Pain is not always apparent in descemetocoele as there are fewer sensory nerves in the deeper layers of the cornea than in the superficial layers. Brachycephalic breeds have less sensitive corneas than other dogs and may display minimal signs of ocular pain (Thomson, 2007).
Intraocular pain occurs with glaucoma or uveitis. This patient was depressed and lethargic which are signs consistent with intraocular pain. Systemic non-steroidal anti-inflammatory drugs (NSAIDs) and opioids were administered immediately to provide analgesia.
Restraint
Restraining patients can be challenging. The best method of restraint for any situation varies with the species involved, the patient's temperament, and the effect desired.
Generally, for ophthalmic examinations, it is best to use as little restraint as possible. As the patient was a brachycephalic breed, great care was taken to prevent struggling and potential protopsis of the globe which can occur because of the breed's shallow orbits and large eyelid openings.
‘The ideal restraint of the ophthalmic patient involves placing one hand gently under the chin and the other hand on the back of the head to prevent sudden head movement and pulling backwards.’
Veterinary investigations
A preanaesthetic blood sample was taken because of the patient's age. This revealed a mild elevation in blood urea nitrogen (15 mmol/l, reference 2–9 mmol/l) and creatinine (185 μmol/l, reference 27 to 124 μmol/l).
An intravenous catheter was placed in the cephalic vein for an infusion of Hartmann's solution (compound sodium lactate, Aqupharm No 11, Animalcare Ltd) to commence at 4 ml/kg/hour before placing the patient under anaesthetic.
Intravenous analgesia of buprenorphine at 0.02 mg/kg and meloxicam 0.2 mg/kg (Metacam, made by Boehringer Ingelheim) was given. A loading dose of a topical antibiotic was administered to his affected eye every 15 minutes for the first four doses and then continued at one drop six times daily. Topical antibiotics were started as soon as the patient came into hospital and were continued post surgery (Exocin was used). Oral synulox was started after surgery and metacam continued orally. The patient was fitted with an Elizabethan collar to prevent potential self trauma to his eye.
Presurgical preparation
Preparation of the eye should only be performed once the patient is fully anaesthetized.
The patient was preoxygenated using the flow-by method of oxygenating. A face mask was not used to avoid causing external pressure on his face and potentially causing a rise in IOP. Midazolam (Hypnovel) 0.2 mg/kg was given slowly to effect just before induction to sedate the patient before anaesthesia was started.
The veterinary surgeon in charge of his care had requested that he was not given acepromazine because this can cause serious side effects in brachycephalic breeds. The patient was then anaesthetized with an non-premedicated dose of propofol at 6 mg/kg.
Periocular hair clipping was not necessary because the surgery was on the ocular surface. Clipping can also irritate the skin surface and risk the patient scratching the eye after surgery.
The ocular surface was rinsed with saline solution (sodium chloride 0.9%, Aqupharm No 1, Animalcare Ltd). This was chosen because its composition is similar to that of the tear film and the aqueous humour (Bowcott, 2009).
The patient was then taken to theatre and placed on a Bair Hugger warming system. He was placed in sternal recumbency and his head was positioned with slight elevation. Elevation of the head helps to reduce venous pressure and therefore IOP (Thomson, 2007). Povidone-iodine solution was used at a concentration of 1:10 to aseptically prepare the skin surrounding the eye.
Owing to the limited access to his head to monitor his depth of anaesthesia, the patient was connected to a capnograph and a blood pressure monitor which was activated to read his systolic, diastolic and mean arterial pressure every 3 minutes.
Instruments prepared
Veterinary surgical procedure
Once the patient had been anaesthetized, the intravenous infusion of Hartmann's solution was increased to 10 ml/kg/hour for the duration of the surgery.
The role of the theatre nurse (the author) was to clean and prepare the area aseptically and position the patient for surgery. The patient was monitored for the duration of his anaesthetic. A conjunctival graft was performed and sutured into place with 8–0 vicryl (made by Ethicon) (Figure 3).
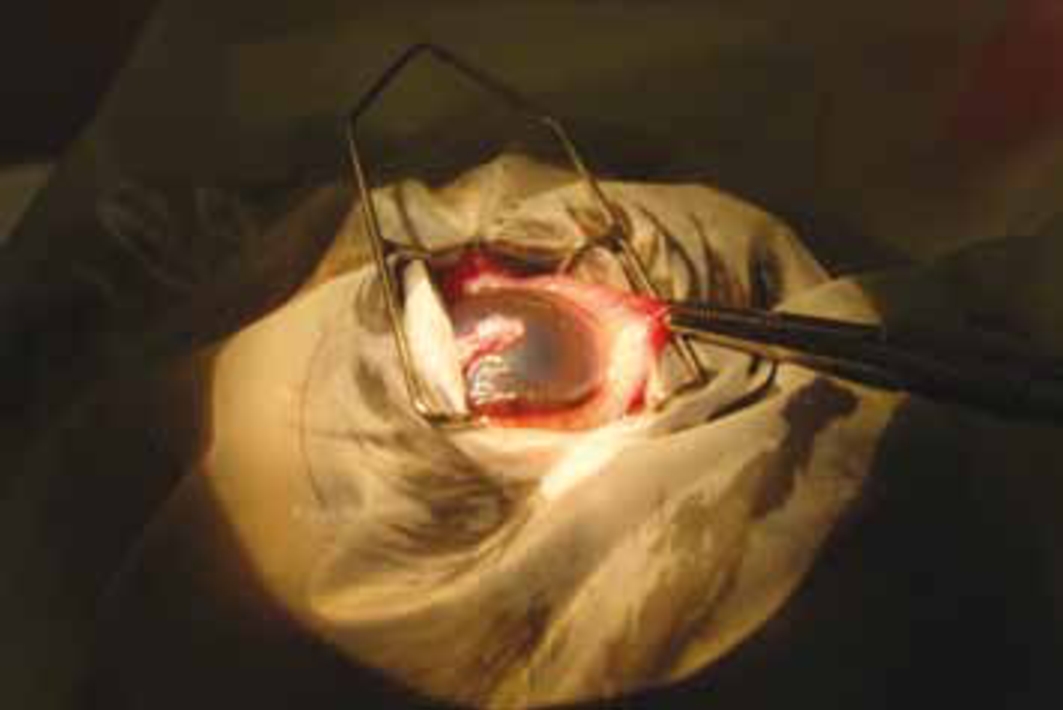
The conjunctiva is the pale pink tissue that covers the sclera (white of the eye). It is a thin, relatively strong tissue containing many blood vessels and this makes it a useful graft material to treat deep corneal ulcers. Under a general anaesthesia, a pedicle of conjunctival tissue is taken from the white of the eye and rotated so that it covers the ulcer. This is stitched in place with very fine dissolvable sutures.
Nursing considerations
The induction of general anaesthesia should be smooth and quiet to keep stress at a minimum. With intravenous access already obtained, the patient could be anaesthetized with minimal restraint.
Intubation was performed when he was sufficiently anaesthetized to avoid coughing or gagging. Topical anaesthesia to the larynx and trachea with 4% lignocaine was used to reduce the likelihood of coughing.
The nurse to this patient (the author) secured his endotracheal tube around his lower jaw, rather than around the back of his head. This helped to prevent distortion of the eye area and kept the tube tie well away from the surgical site.
Preparing the eye for surgery and positioning of the patient are important considerations for corneal surgery. Once the patient had been transferred into theatre, he was positioned in sternal recumbency and used a vacuum surgical pillow to place his head in a way that was comfortable for him, that would not lead to discomfort on recovery, and in the best position for the veterinary surgeon to operate, while ensuring a patent airway. The air was drawn out of the pillow bag to ensure there would be no further movement of the patient's head.
As mentioned above, presurgical preparation included flushing the surface of the eye with sterile saline solution. The eye was finally prepared for surgery using povidone-iodine solution. Povidone-iodone is an excellent ocular disinfectant with both antibacterial and antifungal activity (Hartley, 2010). It is im portant to use the surgical solution and not the scrub, as tincture formulations are irritant and damaging to the ocular surface (Bowcott, 2009).
Povidone-iodine is not well tolerated by the corneal endothelium and should not be used in the preparation of a ruptured globe; sterile saline only should be used to prepare such an eye for surgery. (Hartley, 2010).
A 1:10 concentration of povidone-iodine solution was used to clean the eyelids and surrounding skin. The globe can be cleaned using the same solution at a 1:50 concentration but, because there was risk of a corneal perforation, this was not used to clean the globe. A saline solution (sodium chloride 0.9%, Aqupharm No 1, Animalcare Ltd) was used to clean his eye thoroughly and flush out any remaining debris.
A paradoxical effect is seen on dilution of povidone-iodone, with more dilute solutions exhibiting a greater antibacterial action. Dilutions of 1:10–1:50 for ocular surgery are reported in the literature based on tissue tolerance and bacterial counts (Hartley, 2010).
For the duration of the procedure, the patients’ unaffected eye was taped down to prevent the surface of that eye from dessicating. Respiratory effort, oxygenation levels and heart rate were monitored using capnography.
IOP
It is very important that IOP does not increase during surgery. The anaesthetist will aim to maintain IOP within normal limits, which is in the region of 15–25 mmHg.
A rise in IOP may impair operating conditions and may cause an expulsion of intraocular contents, causing permanent damage to the eye. Too high a pressure may also risk evisceration of the globe and can make surgery very difficult. At worst, it may result in a rupture of the globe. Too low a pressure may result in distortion of the globe making placement of sutures difficult (Brearley, 1999).
Factors increasing IOP can include:
Factors lowering IOP can include:
Recovery
The patient had a smooth recovery. He was placed in a quiet kennel and fitted with an Elizabethan collar to prevent self trauma.
For the 3 days the patient was in hospital, he was walked using a harness rather than a collar and lead to avoid putting unnecessary pressure on his neck. He required regular topical medication so it was important to minimize his stress as much as possible. His Elizabethan collar was replaced after medication was applied to prevent him from causing further trauma to his eye.
Ofloxacin (Exocin, made by Allergan) antibiotic therapy was continued at one drop six times daily. An antibiotic preparation, clavulanic acid and amoxicillin antibiotics (Synulox, made by Pfizer), and an NSAID, meloxicam (Metacam, made by Boehringer Ingelheim), were prescribed for him; these were started the day after surgery.
His pain status was assessed regularly to ensure he was comfortable. The Glasgow Composite Measure Pain Scale (Orskov, 2010) was used as a pain assessment score system to allow a more objective assessment of the patient, which proved very beneficial, especially when it came to a change of nursing shift.
Training clinical staff to recognize the signs of pain and encouraging the use of pain scales helps to improve everyone's observation skills in this area and will promote a more tailored approach to patient analgesia (Orskov, 2010).
The patient was monitored for changes in demeanour, pawing/rubbing at his face or head pressing, all of which indicate of pain. Any changes were recorded and reported to the veterinary surgeon in charge of his care, and his analgesia adjusted accordingly.
IOP was measured once daily to check it remained within normal limits.
The patient remained in hospital for 3 days to ensure the graft was securely in place and viable and so the nursing team could administer his medications (Figure 4).

Conjunctival graft post surgery
Conclusions and recommendations for future practice
Obtaining intravenous access is essential for these patients. On admission, a cephalic catheter was placed. While the patient was anaesthetized, it became apparent that the saphenous vein would have been a better choice for ease of administration of medications and access away from the head.
A routine disposable drape was used for this surgery, with towel clips holding it in place. An adhesive barrier drape would have been a better choice to avoid the trauma and irritation that towel clips can cause. An adhesive drape would also have prevented the irrigating solution leaking onto the patient's head and causing his body temperature to drop. A Bair Hugger warming system was used; heat and moisture exchangers could also be used to help prevent hypothermia.
The author is now aware of the potential obstacles an ophthalmic patient may pose. With knowledge of the procedure to be undertaken and careful planning, these obstacles can be overcome with ease.
