There are many surgical options available for the different types of elbow disease. Most long-term studies report a progression of osteoarthritis (OA) regardless of the treatment performed. This article aims to describe both the surgical and nonsurgical treatment options available, and follows on from canine developmental elbow disease part one which looked at the aetiopathogenesis and diagnosis of developmental elbow disease (Fernee-Hall and Janovec, 2021).
Developmental elbow disease is the term encompassing several abnormalities of the elbow joint including fragmented medial coronoid process (FCP), osteochondrosis of the humerus (OC), united anconeal process (UAP), cartilage injuries and incongruity of the elbow joint. These disorders are associated with varying degrees of joint instability, inflammation, and loose fragments within the joint, which result in lameness and osteoarthrosis (Marti-Angulo et al, 2014).
Treatment should ideally involve correcting the underlying causes of the disease before significant joint damage has occurred. Unfortunately, the complex aetiopathogenesis makes identification of the early stages of disease difficult and late diagnosis leads to inconsistent clinical outcomes as the disease progresses (Michelsen, 2013).
Non-surgical management
There is conflicting evidence as to the benefit of surgical management of different forms of elbow disease. In a study by Burton et al (2011) conservative management resulted in the same outcome in dogs at 53 weeks after surgery as dogs treated with arthroscopic surgery. Conservative management involved a 6 week course of a non-steroidal anti-inflammatory drug (NSAID) called Tepoxalin, a week of room rest followed by 5 minutes of lead exercise twice daily for a week, which increased by 5 minutes a week for the next 2 months. Nonsurgical treatment is always part of the long-term management plan as virtually all dogs diagnosed with elbow disease progress to develop variable degrees of OA at some stage of their lives (Krotscheck and Bottcher, 2018; Coghill, 2020). The following conservative measures can be helpful:
- Careful control of bodyweight — weight loss can decrease clinical signs because of the decreased forces placed on abnormal joint surfaces.
- Controlled exercise such as gentle lead walking — avoiding activities such as running, turning at speed, chasing a ball, rough and tumble with other dogs, braking sharply and jumping down to land on the forelimbs.
- Hydrotherapy — this is beneficial as it works the muscles without overloading the elbow joint (Figure 1). Archimedes' principle states that the upward buoyant force that is exerted on a body immersed in a fluid, whether fully or partially submerged, is equal to the weight of the fluid that the body displaces. The force of buoyancy can assist movement in weak or injured limbs, and provide support and reduced loading to painful or healing structures (Monk, 2007). The buoyancy, resistance and hydrostatic pressure properties of water are useful for patients with OA (Mills and Ciuperca, 2015). Studies in humans have shown that hydrotherapy can reduce pain and improve range of joint motion. A study of Labradors with elbow disease by Preston and Wills (2018) found that a single hydrotherapy session increased range of motion and stride length in all the participants with elbow disease.
- Dietary supplements such as omega 3 fatty acids, glucosamine and chondroitin sulphate may help — in particular, administration of the omega-3 fatty acids have been shown beneficial in multiple studies in the context of long-term management of OA in canine patients because of its anti-inflammatory properties. Prescription diets for dogs with OA can also be beneficial as they typically contain higher levels of these specific nutrients. A study by Marti-Angulo et al (2014) split 105 Labradors into two groups and gave one group a supplement containing hyaluronic acid, enzymatically hydrolysed collagen, glucosamine, chondroitin sulphate and gamma oryzanol. They found that at 12 months 18.5% of the treatment group had radiographically confirmed elbow disease compared with 33.3% of the control group. At 20 months the treatment group showed significant improvements in terms of lameness and range of motion.
- Analgesia — analgesia such as NSAIDs or multimodal analgesia may be required on a daily or as-needed basis.
- Intra-articular injections — injections of corticosteroids, hyaluronic acid, and blood derived products into the joint, such as platelet rich plasma, have been reported to improve limb function for up to 6 months (Krotscheck and Bottcher, 2018). However, they have a limited duration of effectiveness and more studies are needed to better assess their potential in managing OA associated clinical signs, such as lameness and discomfort.
- Photobiomodulation therapy (PBMT) — PBMT is the use of red/near infrared light to stimulate healing, provide analgesia and reduce inflammation. Cellular targets absorb specific wavelengths of light, initiating intracellular processes that create biologic effects (Looney et al, 2018). It can be used within physiotherapy to modulate tissue function without creating a thermal effect. It is painless, non-invasive and can be administered in primary care settings (Preston and Wills, 2018). A study of 11 dogs with degenerative joint disease by Preston and Wills (2018) looked at pain scoring, pre and post-treatment lameness scores and NSAID dose and frequency. It found that 82% of dogs undergoing PBMT were able to reduce their dose of NSAID by at least 50%, compared with 0% of the control group. Improvements in gait and pain scoring were also seen in the group undergoing PBMT.
- Home modifications and considerations — little and often exercise is recommended for osteoarthritic joints and over exercising can result in excessive load on a joint and an acute inflammatory response. The following questions may be useful to manage the OA associated with elbow disease:
- Does the dog have a warm, comfortable sleeping area which is easily accessed?
- How frequently and for what duration is the animal walked?
- Does the dog have access to stairs?
- How do family members and other pets play with the dog? For example, is there unlimited ball throwing and play fighting?

Surgical management
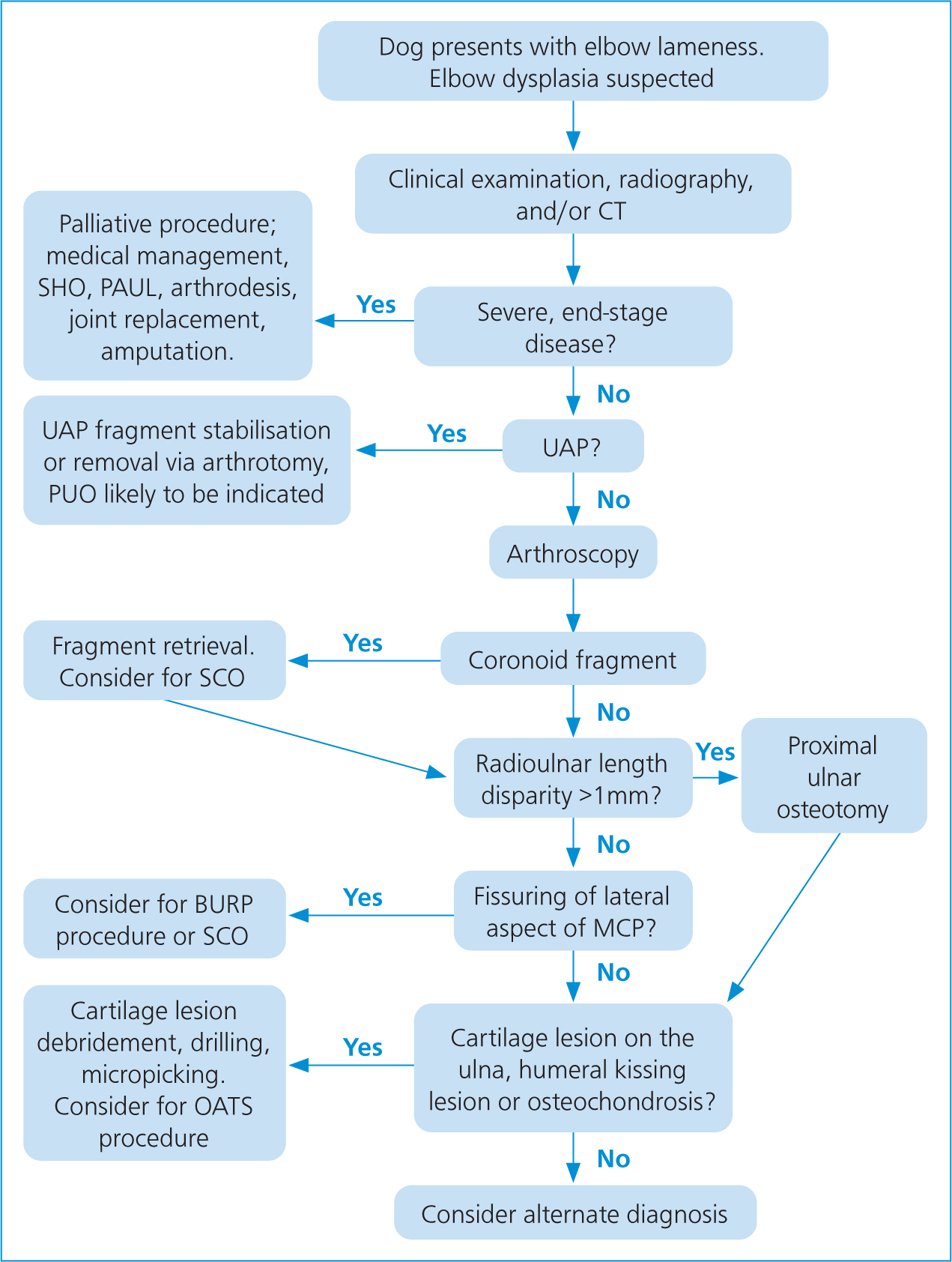
Treatment should be aimed at correcting any pathology within the joint and could include the retrieval of loose fragments, resection of damaged subchondral bone and the debridement or replacement of damaged cartilage. Ideally these procedures should be performed arthroscopically (Michelsen, 2013). A decision-making algorithm is shown in Figure 2.
Palliative procedures are undertaken when the joint disease is so severe that addressing the underlying pathology and secondary consequences is likely to be insufficient or when more conservative treatment has failed. Palliative procedures include those that unload the medial compartment, replace joint surfaces, or manage pain.
It is difficult to say which surgical options are most appropriate because of a lack of objective data, but this article will briefly outline the options available.
Fragmented medial coronoid process
Surgical options for the management of FCP include fragment removal and/or subtotal coronoid ostectomy via a conventional open arthrotomy or as an arthroscopically assisted procedure. In dogs with documented radioulnar incongruity, this can be combined with a bi-oblique dynamic proximal ulnar osteotomy.
Arthroscopic assessment is the ‘gold standard’ in determining the presence of fragmentation or cartilage lesions. It can be used diagnostically to confirm the presence of FCP and therapeutically to extract fragments and remove abnormal cartilage with a burr. Therapeutic arthroscopy to surgically remove the fragments of bone can lead to improvement. Evans et al (2008) concluded via a meta‐analysis of 400 candidate manuscripts that arthroscopy is superior to medical management with an improvement of 17%, and that the probability is arthroscopy is superior to medial arthrotomy with an improvement of 14%. Barthelemy et al (2014) also reported an improvement on gait analysis of dogs treated arthroscopically. If incongruence is a contributing factor, then fragment removal will not necessarily address the issues caused by this. Conventional fragment removal, abrasion arthroplasty of the diseased portion of the medial aspect of the coronoid process may provide short-term mitigation of clinical signs, but progression of OA invariably occurs, and persistence of lameness is common (Fitzpatrick et al, 2009). However, a study of Bernese mountain dogs by Samoy et al (2013) concluded that removal of the FCP lesion without treatment of incongruity was a valuable treatment option.
Bi-oblique dynamic proximal ulnar osteotomy (BODPUO) evolved in an attempt to relieve lameness caused by incongruity of the humeroulnar joint. Making an oblique cut of the osteotomy to the ulna, using an oscillating saw or Gigli wire saw, allows caudomedial rotation of the proximal ulnar. This may improve humeroradial joint loading and reduce the load acting on the medial coronoid ridge. An ulna ostectomy or removal of a small slice of ulna is also an option as it allows rotation of the ulna, which closes the humeroradial gap and improves congruity.
Osteochondritis dissecans
Removal of the flap of cartilage arthroscopically is the conventional surgical treatment, followed by the use of a high speed burr or curette to remove nonviable subchondral bone and bring blood supply and cells to the joint surface to help with healing. However, a defect will remain in the joint surface. Some dogs may improve clinically after treatment, but in many cases, they remain chronically lame and OA progresses despite treatment (Michelsen, 2013).
OC lesions can also be repaired using the osteochondral autograft transfer system; where a circular plug of healthy articular cartilage is harvested from a non-articular site, such as the lateral trochlear ridge of the femur, and placed onto a matching defect created at the site of the cartilage lesion. A study by Fitzpatrick et al (2009) combined arthroscopic assessment and subtotal coronoid ostectomy with debriding of the OC lesion and resurfacing with osteochondral core grafts harvested from the stifle. They reported positive short-term outcomes, but concluded that more investigation was required.
The SynACART system is a synthetic cartilage plug for treating osteochondral defects. The defect is filled by the implant which restores the surface of the articular cartilage. The system is similar to the osteochondral autograft transfer (OATS) procedure, but achieves successful repair of defects without concern for sufficient donor cartilage, correct matching of surface topography or donor site morbidity (Fitzpatrick and Dona, 2018). A study of 13 dogs undergoing placement of SynACART implants alongside surgery to treat medial compartment disease (MCD) and incongruity resulted in outcomes considered excellent at final assessment in five (55.6%) elbows and acceptable in three (33.3%). One elbow had an unacceptable outcome as a result of persistent lameness 4 months postoperatively and obvious progression of OA, requiring revision surgery (Fitzpatrick and Dona, 2018).
Ununited anconeal process
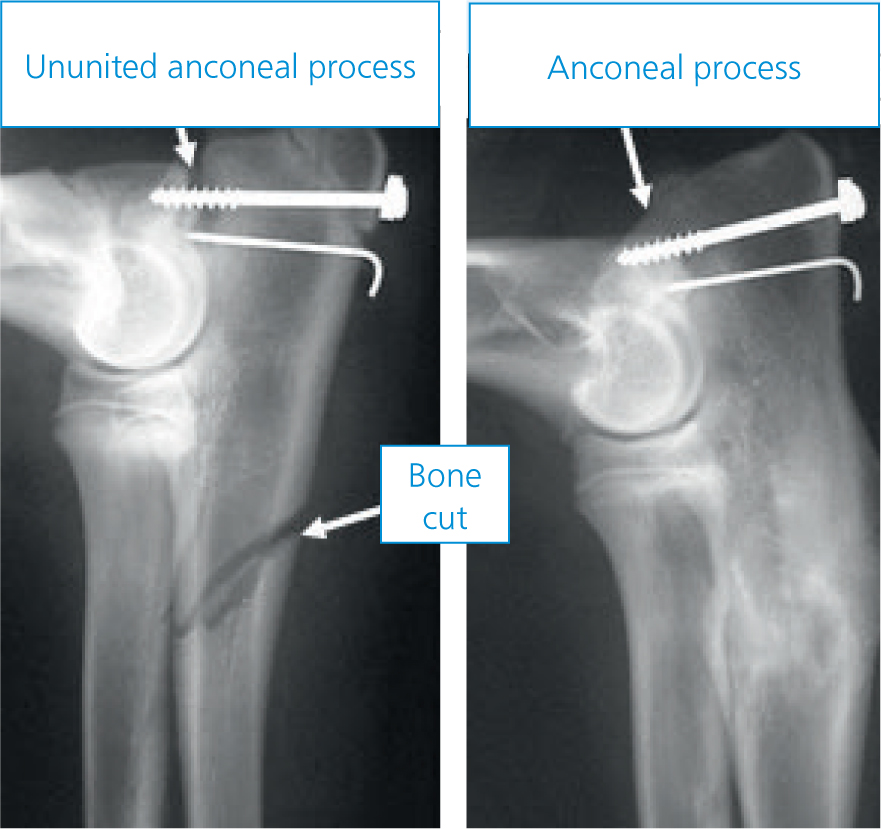
Lameness as a result of UAP can respond to a combination of strict rest and NSAIDs over a 4 to 6-week period. (Burton and Owen, 2008). Failure to respond or recurrent episodes of lameness would be indications for surgical intervention. If the diagnosis is made in young dogs the UAP can be reattached to the ulna with a lag screw. An ulna osteotomy also needs to be performed to take the abnormal pressure off the anconeal process and allow it to heal (Figure 3). Fixation of the UAP fragment combined with an ulna osteotomy appears to provide the best return to function (Pettitt et al, 2009). Arthroscopic examination of these cases is recommended as many will have other changes such as FCP. In older dogs the UAP rarely fuses back onto the ulna, even following surgery, and may have to be removed. Early treatment and fusion of an uncomplicated UAP indicates a favourable prognosis for the joint. However, significant unresolved joint incongruency, delayed diagnosis or treatment and presence of an FCP in an elbow joint suggest that development and progression of osteoarthritis is likely (Shales, 2006).
Medial compartment disease
Micro-cracks can be present in the medial coronoid process, adjacent to the fissure even if it appears healthy so subtotal coronoid ostectomy (SCO) has been proposed in addition to fragment removal (Krotscheck and Bottcher, 2018). Micro-cracks may lead to recurrent fragmentation and chronic pain. SCO may also improve joint congruency.
SCO, a limited surgical approach, is made to the medial joint compartment and an en-bloc resection of the medial coronoid region is performed using either an osteotome and mallet or an oscillating blade. The objective is to remove portions of the coronoid that are visibly diseased. As mentioned above, this procedure can also be conducted using arthroscopy. A study by Fitzpatrick et al (2009) of 263 dogs undergoing SCO concluded that in the medium-term 81.9% dogs remained sound, with significantly improved daily function scores compared with preoperative values.
Adult dogs with MCD and OA, without significant pathology in the lateral compartment (confirmed by arthroscopy) and a lack of response to conservative management, may benefit from a proximal abducting ulnar osteotomy (PAUL) procedure or sliding humeral osteotomy (Krotscheck and Bottcher, 2018). Arthroscopic evaluation should be performed beforehand, and conventional joint debridement carried out. The goal of these procedures is to unload the medial compartment.
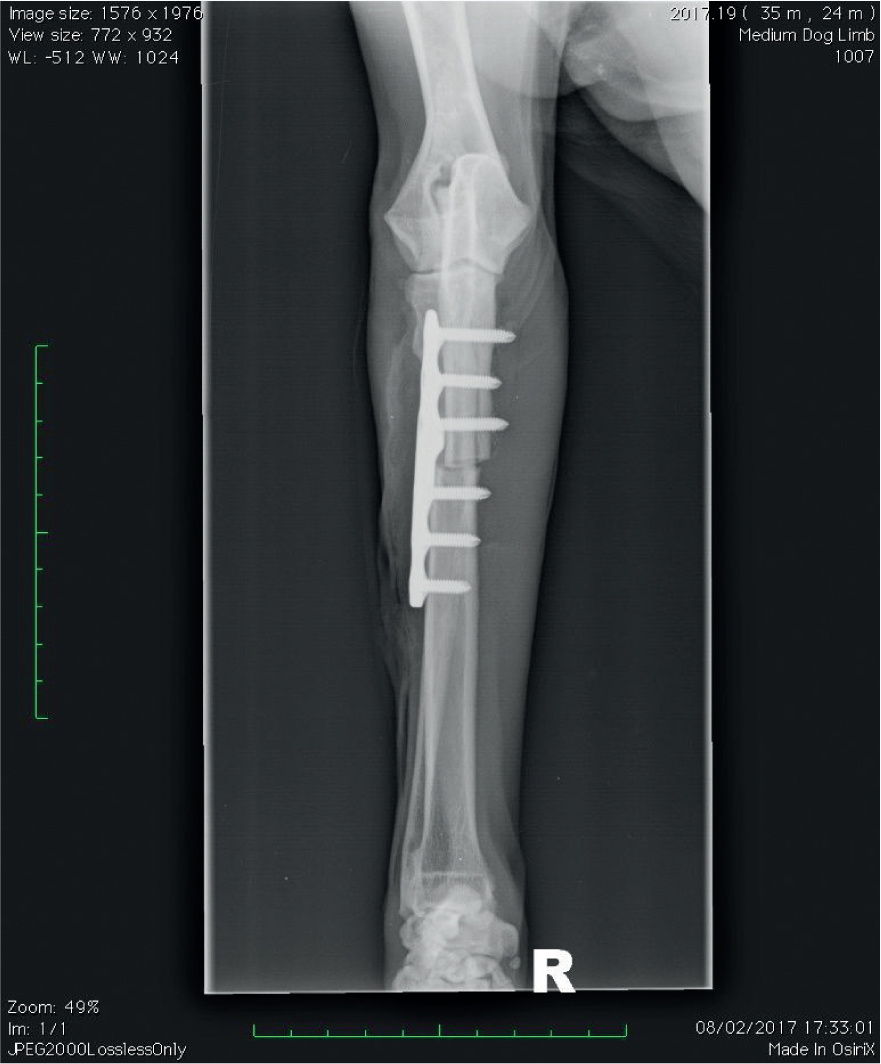
PAUL is a proximal osteotomy of the ulna fixed by a stepped plate (Figure 4). The technique aims to shift the axis of weight-bearing from the damaged inner surfaces of the joint to the healthy outer surfaces of the joint. Coghill et al (2021) compared 30 dogs with medial compartment disease treated with arthroscopic fragment removal and/or PAUL procedure and found the PAUL procedure showed no owner-assessed benefit over arthroscopic medial coronoid fragment removal for dogs with MCD.
Sliding humeral osteotomy is a procedure that involves cutting the humerus and realigning it with a stepped plate to attempt (similar to the PAUL procedure) to shift the weight-bearing forces off the area of cartilage damage in the medial compartment onto the area of ‘good cartilage’ in the lateral compartment. It is a more complex surgery than the PAUL procedure and historically had a relatively high rate of complications. A study of 32 dogs by Wendelburg (2011) reported that 90% of owners felt that lameness had diminished during the final follow-up post sliding humeral osteotomy, and concluded that sliding humeral osteotomy can be performed successfully in dogs to limit the radiographic progression of osteophytosis and increase use of the affected limb. However, 10 dogs suffered complications and six of those were considered major and required further surgery. A study of 60 limbs by Fitzpatrick et al (2015) reported that lameness resolved in 49 of the 60 limbs operated on. They concluded that sliding humeral osteotomy improved the pain and lameness caused by medial coronoid disease at mid-term follow up.
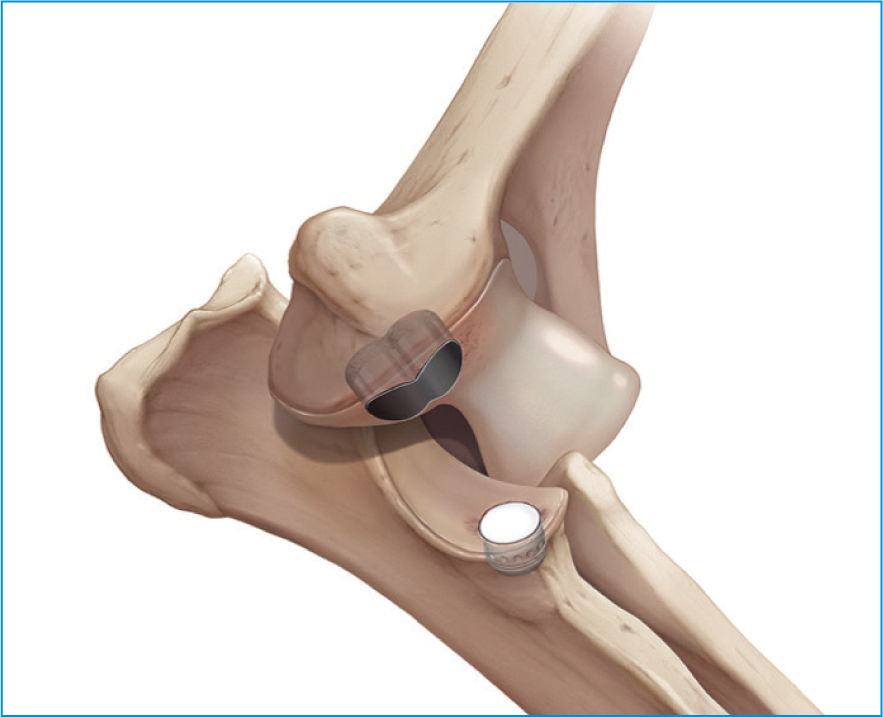
Canine unicompartmental elbow replacement (CUE) is a treatment option for dogs with the most severe form of medial compartmental disease (Figure 5). It involves partially resurfacing the elbow joint. An implant made from cobalt chrome and titanium is inserted into the trochlea of the humerus to restore the gliding surface. The other implant is made from ultrahigh molecular weight polyethylene (UHMWP) and titanium and is placed in the ulna. It articulates with the other implant resulting in low friction, pain free movement for the elbow. It is considered a better option than total elbow replacement as it has faster improvement rates and carries significantly lower risk as it does not require any major bone cutting or a large surgical approach (Coppieters, 2015). This unicompartmental technique has some conceptual advantages compared with the total elbow replacement techniques and the load-shifting osteotomies. First, CUE is designed to restore physiologic medial compartment loading as closely as possible. Second, CUE still allows supination and pronation of the radius and ulna in contrast to total elbow replacement where a fusion is created between the radius and ulna. Third, CUE implantation can be done without violation of the collateral ligaments, which may decrease the likelihood of postoperative complications such as joint luxation. The CUE also allows several strategies for revision in case of complications (Coppieters, 2015). A study by Cook et al (2015) evaluated mid to long-term outcomes in 103 cases undergoing CUE. Canine unicompartmental elbow was associated with one catastrophic (1%), 11 major (10.7%), and 28 minor (27.2%) complications. Outcomes following CUE were reported as full function in 49 cases (47.6%), acceptable function in 45 cases (43.7%), and unacceptable function in 9 cases (8.7%). The study concluded that CUE arthroplasty is an appropriate consideration for treatment of MCD of the elbow in dogs.
Total elbow replacements
A small number of referral hospitals do provide total elbow replacements. As with joint replacements in general, this involves removal of the diseased joint surfaces. These are then replaced with metal implants anchored within the bones and covered with UHMWP to provide low-friction articular surface substitute. Elbow replacements are much more complicated than total hip replacements, for example, because there are three joint surfaces, which come together in the elbow compared with two in the hip. Additionally, it is much more difficult to reproduce the normal motion of the elbow than the hip. As a result of these and other challenges it has been difficult to develop a reliable and commercially available implant system. Furthermore, adequate exposure is difficult to achieve with the elbow joint so surgical times are likely to be longer, leading to increased risk of infection. The complication rate for this surgery is relatively high and the salvage option would be an elbow arthrodesis (fusion of the elbow). This, however, results in a dramatically altered gait and loss of range of movement (Michelsen, 2013). A paucity of objective data on clinical outcomes following total elbow replacement exists. In a study assessing radiographic and clinical outcomes following the Biomedtrix TATE® elbow arthroplasty, a high complication rate (60% perioperative complication rate) and variability in implant placement was documented (De Sousa et al, 2016). In the same study, 24% of dogs were shown to have full, 52% acceptable, and 24% unacceptable outcome.
Conclusion
Developmental elbow disease encompasses multiple abnormalities and disease processes of the elbow joint, including incongruity, medial coronoid disease, osteochondritis dissecans, fragmented coronoid process and UAP. Several abnormalities may coexist in the same joint. Fitzpatrick et al (2009) explained how the spectrum of clinical signs and macroscopic pathology associated with any single disease process complicate the decision-making for treatment. Clearly, there is no single treatment for all the recognised manifestations of elbow dysplasia.
There are many treatment options available. Fitzpatrick et al (2009) have even written algorithms for the treatment decision-making for medial compartment disease. According to Krotscheck and Bottcher (2018) the mid to long-term prognosis for dogs with medial coronoid process disease and/or osteochondritis dissecans, as well as the efficacy of treatment options remains poorly defined. They go on to conclude that most studies report some sort of improvement in lameness despite radiographic progression of OA and that the combined presence of FCP and OC lesions warrants a guarded to poor prognosis. ‘Surgical treatment of end stage medial compartment disease bears a favourable prognosis regardless of the surgical technique performed.’ (Krotscheck and Bottcher, 2018: 884). Several procedures are often combined for the management of MCD depending on the specific lesions identified and surgeon's personal preference. Combining surgical techniques means that it is impossible to compare the efficacy of any one technique. This combined with data often being subjective, the non-standardised definition of a successful outcome and the fact that radiographic changes do not correlate well with clinical signs, limits the ability to identify statistical significance between treatment groups.
A gait analysis study of 20 dogs with medial coronoid disease (Burton et al, 2011) compared dogs treated arthroscopically with removal of coronoid fragments and burring of any associated chondromalacic cartilage and dogs treated conservatively. It was concluded that there is no therapeutic benefit to arthroscopic removal of FCP or chondroplasty of the medial coronoid process. Until a therapeutic modality is created, which can address incongruence, cartilage, and subchondral bone degenerative change concurrently, it is unlikely that surgical intervention will improve outcomes in this disease beyond those achieved with medical management alone.
KEY POINTS
- Treatment should ideally involve correcting the underlying causes of the disease before significant joint damage has occurred.
- Treatment should aim to improve joint pathology by removing fragments or improving incongruity.
- Palliative procedures, such as proximal abducting ulnar osteotomy (PAUL) and sliding humeral osteotomy, can be used to unload the medial compartment, replace joint surfaces or manage pain when conservative treatments have failed.
- Conservative management such as weight management, hydrotherapy and analgesia are important to manage the concurrent osteoarthritis and pain.
- Canine unicompartmental elbow replacement partially resurfaces the joint surfaces and carries fewer complications than total elbow replacement.


