Common indications for dialysis include acute kidney injury (AKI), chronic kidney disease (CKD) and toxin ingestion (Bloom and Labato, 2011). In the USA, haemodialysis is regularly used to treat patients with CKD; however in the UK, haemodialysis is only available for treatment of patients with AKI and toxin ingestion.
Bloom and Labato (2011) describe the indications for haemodialysis in patients suffering with CKD, including hyperkalaemia, fluid overload and progressive azotaemia. Haemodialysis is also used prior to renal transplantation in the USA — a procedure not carried out in the UK. Bloom and Labato (2011) further described indications for haemodialysis in patients with AKI including persistent azotaemia, electrolyte abnormalities, acidosis and oliguria/anuria despite treatment with appropriate medical management.
Intermittent haemodialysis
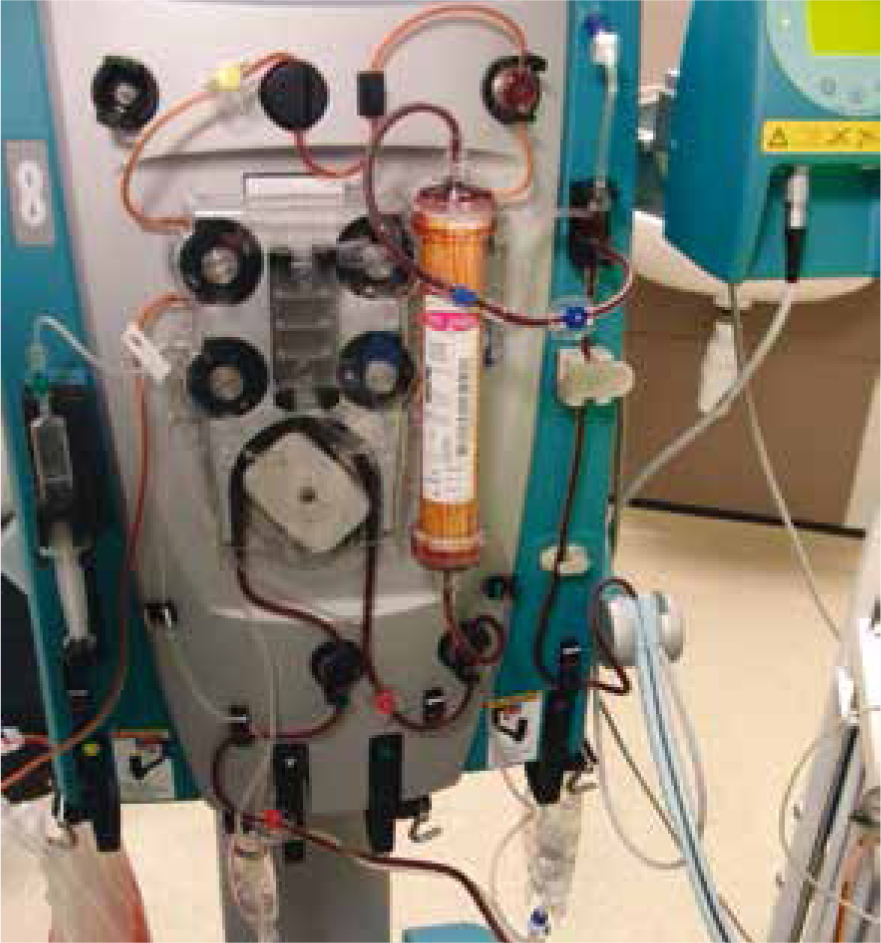
Intermittent haemodialysis (IHD) was first carried out in the early 1900s when a pharmacologist experimented by passing arterial blood from animal patients through an array of semi-permeable membranes suspended in a fluid solution, before returning the blood to the patient. The composition of the patient's blood was altered by changing the solute in which the semi-permeable membranes were fixed (Acierno, 2011). Today, IHD is commonly carried out for patients with AKI, CKD and toxin ingestion by universities and specialist veterinary referral centres (Figures 1 and 2) (Bloom and Labato, 2011).


Continuous renal replacement therapy
More recently, continuous renal replacement therapy (CRRT) has been used in animals. As the name suggests, CRRT is a continuous process carried out until either the patient's renal function returns, or they are able to be started on IHD. Although the process of CRRT is similar to IHD, there are several different treatment options available with CRRT. Unlike IHD, which uses a diffusive process, CRRT combines the use of both diffusion and convection to filter the patient's blood.
The use of convection to filter solutes from the blood is known as haemofiltration (HF), and relies on hydrostatic pressure to filter plasma across the semi-permeable membranes. Haemodialysis (HD) is similar to IHD and uses a diffusion gradient to filter the plasma across the semipermeable membranes. HD is efficient at removing small molecules such as creatinine, urea and potassium from the plasma. However, HF should be considered for removing larger molecules, as this is far more effective. Haemodiafiltration (HDF) combines the use of both convection and diffusion to filter the plasma, and is useful in cases where both smaller and larger molecules require filtering (Pannu and Noel Gibney, 2005).
A significant advantage of CRRT (compared with IHD) is that it more accurately mimics the role of the kidney by slowly filtering the patient's blood, therefore allowing greater control of the patient's electrolyte and acid–base balance (Figure 3)(Acierno, 2011).
Therapeutic plasma exchange
Therapeutic plasma exchange (TPE) is also used in veterinary patients, removing high-molecular weight molecules from the patient's plasma. TPE is often used to remove harmful antibodies from the patient's plasma (Joint United Kingdom Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee (JPAC), 2014). JPAC (2014) describes the need to carry out TPE only when good evidence of its effectiveness is available. In people, there is a wide range of conditions for which TPE may be beneficial. A common crossover for its use in canine patients is in the treatment of myasthenia gravis — an autoimmune neuromuscular condition causing weakness of the skeletal muscles. TPE has also been used for veterinary patients with immune-mediated haemolytic anaemia (IMHA), although its efficacy in treating this condition is still unknown.
Peritoneal dialysis
Peritoneal dialysis (PD) effectively uses the same technique as IHD and CRRT. However, instead of removing the blood and passing it through a semi-permeable membrane, PD uses the peritoneum as a membrane across which to diffuse solutes. Dialysate fluid, high in glucose but low in potassium, is passed into the peritoneal cavity and left for a predetermined period of time before being removed. During this time, diffusion and osmosis occur, allowing the removal of water, electrolytes, toxins and other small molecules from the peritoneal blood, into the dialysate. The most common use of peritoneal dialysis in veterinary patients is to treat AKI (Cooper and Labato, 2011).
HD catheter placement and care
Typically, a dual lumen haemodialysis catheter is placed into a central vein. The lumen removing blood from the patient is termed the arterial port, and the lumen returning the blood to the patient is the venous port (Chalhoub et al, 2011) (Figure 4).

HD catheter care is extremely important, and each member of the team should be familiar with the basic techniques. Chalhoub et al (2011) described that the catheter site should be checked prior to dialysis and cleaned with an antiseptic solution. HD catheter ports should be scrubbed aseptically for 3–5 minutes prior to and after every use, and the veterinary surgeon handling the catheter should wear sterile gloves when the catheter is not in use. After use, the catheter should be bandaged securely, not remaining visible (Chalhoub et al, 2011).
Even though they are produced from antithrombogenic materials, one of the main complications of HD catheters is thrombus formation. Between cycles, all lumens of the catheter must be filled with an anticoagulant solution to prevent thrombus formation. This solution must be removed from the catheter prior to the next dialysis cycle (Chalhoub et al, 2011).
Anticoagulation
Anticoagulation therapy in dialytic patients is required to ensure excessive blood loss does not occur as a result of thrombosis in the extracorporeal circuit. This must be balanced through use of anticoagulant therapy that will not put patients at increased risk of excessive bleeding (Ross, 2011).
Unfractionated heparin
There are two methods of anticoagulation most frequently used during the HD process. The first is unfractionated (UF) heparin, administered usually as a bolus dose, followed by a continuous rate infusion (CRI) (Bloom and Labato, 2011). UF heparin works by binding to antithrombin; the resultant molecule causes the inactivation of many coagulation factors. UF heparin is relatively inexpensive and easy to administer. It is therefore the most frequently used method of anticoagulation in human patients. The administration of heparin results in systemic anticoagulation of the patient, successfully anticoagulating blood within the extracorporeal circuit (Ross, 2011).
The use of heparin may not be appropriate for patients with increased risk of bleeding, and requires careful monitoring of the patient's activated clotting times (ACTs) throughout its use. Results of the ACTs can be used to adjust the CRI administered to the patient (Acierno, 2011).
Citrate
Citrate is the second most commonly used method of anticoagulating the patient, and requires an infusion of citrate anticoagulant into the extracorporeal circuit. Citrate binds to calcium — which is essential to the clotting cascade — and the resulting calcium-citrate complexes formed are removed as they pass through the dialyser (Acierno, 2011). A CRI of calcium must be administered to the patient, and blood calcium levels monitored regularly because of the risk of hypo-or hypercalcaemia. An advantage of citrate anticoagulation is that only local anticoagulation within the extracorporeal circuit occurs, and blood returning to the patient is unaffected, reducing the risk of bleeding (Acierno, 2011).
Administration of blood products
Repeated blood sampling, loss of blood or clotting in the extracorporeal circuit, and the physiological effects of uraemia, all result in the loss of blood in the patient (Elliott, 2011). In some cases, a blood transfusion of either whole blood or packed red blood cells may be required. It is beyond the scope of this article to discuss this in further detail; however, veterinary nurses caring for these patients should have good knowledge and understanding of handling and administering blood products, as well as the risks associated with their use, and possible reaction complications that may occur.
Nursing care
One of the biggest challenges when carrying out IHD, CRRT and TPE, is ensuring there are adequate numbers of trained individuals able to organise and run the procedure. These individuals must not only be competent at running the dialysis machine, but also have an advanced understanding of renal physiology (Acierno, 2011). The veterinary nurse will be required to think about the ongoing needs of the patient throughout the dialysis cycles performed. Patients will most likely be sedated to avoid movement-related catheter complications such as kinking, dislodgement and patient removal. Table 1 considers some of the main nursing considerations of these patients.
| Aspect of care | Nursing consideration |
|---|---|
| Sedation | Ensure the patient is suitably sedated for the procedure and cardiovascular and respiratory function is adequate |
| Temperature | Ensure the patient remains normothermic by use of active warming devices, e.g. Bair Hugger™ (3M) blankets. Fans and active cooling techniques may be used in the event the patient develops hyperthermia unrelated to pyrexia |
| Movement | Ensure the patient remains comfortable and that adequate padding is provided under joints and bony areas. Sedated patients may require turning depending on the length of the cycle. Physiotherapy techniques may be required during continuous therapies |
| Eye care | Eye lubrication should be applied throughout sedation |
| Oral care | Oral care should be provided while the patient is unable to eat and drink. This involves cleaning the mouth with an appropriate solution and ensuring the tongue does not swell or become clamped between the patient's teeth. Mouth gags may be required to prevent this |
| Catheter care | See dialysis catheter care. Any peripheral intravenous catheters should be managed as per practice protocol |
| Nutrition | Nutrition should be considered between cycles. See section on nutritional requirements |
| Urinary catheter care | The patient's urinary catheter should be monitored closely and handled aseptically. Urine output and specific gravity should be monitored based on the clinician's instructions. Patients without a urinary catheter may require their bladder to be expressed to prevent urine scalding (under veterinary instruction) |
| Blood sampling and monitoring | Frequent blood sampling will be required to check a variety of parameters. Results should be reported back to the veterinary surgeon running the dialysis cycle and recorded on the patient's hospital record |
| Blood pressure | Regular blood pressure checks will be required throughout and between dialysis cycles. Interventions may be required should the patient become hypo-or hypertensive |
| Record keeping | It is vital that clear and concise hospital records are kept for these patients. All aspects of care should be documented |
| Administration of medication | Prescribed medications should be administered in accordance with the patient's hospital record. This may include anti-emetic medication or antibiotics |
Nutritional requirements
The ongoing nutritional needs of a dialytic patient are still in debate, with many of the current veterinary recommendations taken from human medicine. Elliott (2011) described a consequence of the dialytic process not only removing uraemic toxins, but also removing free and bound amino acids and peptides, and water-soluble vitamins, further contributing to muscle wasting.
The increased catabolism that occurs in patients with uraemia suffering a chronic inflammatory response is also a concern. Activation of the complement cascade (associated with the process of HD) causing the release of cytokines, combines with acute-phase proteins known to have significant detrimental effects on protein metabolism, to contribute to protein energy malnutrition (PEM). The development of PEM in dialytic patients is significant since PEM is associated with morbidity and mortality (Elliott, 2011).
It is therefore important in these patients to consider an appropriate method of providing nutrition. Ideally, all patients would receive oral nutrition; however, anorexia is a common factor at play in patients with renal disease. Feeding techniques should be trialled to encourage oral intake of food. Techniques include: tempting the patient; warming the feeds; trialling diets; environmental/mental stimulation; and avoiding the development of food aversion.
Placement of a feeding tube may be required, allowing the provision of enteral nutrition either continuously or via bolus feeds. Dialytic patients will often require balanced renal diets. These may be specifically formulated for administration via a feeding tube, or may require blending with water, which can result in difficulty during administration with nasogastric or nasoesophageal feeding tubes that have a smaller lumen. For the administration of thicker diets, an oesophagostomy or gastrostomy tube can be used. Consideration of patient safety/stability is important because of the additional requirement of a general anaesthetic to place these larger bore feeding tubes.
Parenteral nutrition (PN) may be required in patients unable to meet their nutritional requirements through enteral feeding. Total PN requires a central line for the delivery of a hyperosmolar solution of dextrose, amino acids, electrolytes and intralipid, making it a less-than-ideal option for patients that already have a central HD catheter placed (Elliott, 2011). The administration of partial PN is more easily achieved, as the isotonic solution can be delivered through a peripheral catheter—although the patient's full nutritional requirements are unlikely to be met. Veterinary nurses administering PN must use strict aseptic technique when setting up and administering PN owing to the increased risk of catheter-related sepsis (Elliott, 2011).
Conclusion
There are many nursing considerations for the dialytic patient, including nutritional requirements which must be met. These cases can be extremely complex, but can also be rewarding to nurse, and provide great professional and emotional satisfaction.
In the UK, there is currently only one facility offering HD, and PD in veterinary patients is still largely limited to specialist referral hospitals and universities. Both require dedicated veterinary surgeons and veterinary nurses, experienced in performing these procedures.

