As recognised by Tivers (2011), surgical complications are an unfortunate element of both medical and veterinary practice. Up to 50% of complications reported within human health care occur within the peri-operative setting and of those, 50% are considered to be preventable (Gawande et al, 1999; de Vries et al, 2008).
‘Never events’ are serious, largely preventable patient safety incidents that should not occur if available preventative measures are implemented (Kizer and Stegun, 2005). While some of these events are unavoidable, it is widely accepted that others are attributable to human error (Christian et al, 2006; Tivers, 2011). Although this has been acknowledged in the veterinary literature, in particular in reference to retained surgical swabs (Tivers, 2011), there has been less veterinary focus on how such ‘never events’ can be reduced. This is despite the presence of an evidence-based initiative developed by the World Health Organisation (WHO), known as the Safe Surgery Saves Lives campaign (World Health Organisation, 2008). What follows here is a discussion of the WHO Surgical Safety Checklist (SSC) devised as a result of this campaign and observations on its adaptation and subsequent implementation into a veterinary practice.
The origins of SSCs and the evidence base for their use in the peri-operative period
The operating room (OR) is acknowledged to be one of the most complex work environments in human health care, so it is perhaps unsurprising that it has such a high potential for complications (Christian et al, 2006; Haynes et al, 2011). Due to the nature of the treatment and care provided in the OR, these complications are closely associated with increased patient morbidity and mortality (Haynes et al, 2009). As a result, much research in medical practice has focused on finding the root causes of these events which compromise patient safety.
A prospective study by Christian et al (2006) suggests that communication breakdown and information loss, in combination with high workloads, competing tasks and rapidly changing situations, pose the greatest risks to human patient care in the surgical environment. Further to this, Mazzocco et al (2009) link team behaviours in the OR to improved outcomes, demonstrating that human patients have an increased likelihood of complications or death when there are difficulties with both teamwork and information sharing during key intraoperative phases. As none of these elements are exclusive to human ORs, it is proposed that avoidable surgical complications in veterinary ORs may have similar causes. For example, Figure 1 illustrates a surgical team working together in a veterinary OR during a period of intra-operative haemorrhage, a time where teamwork and communication are vital in order to safeguard the patient.

On the basis of WHO guidelines identifying multiple recommended practices to ensure patient safety (World Health Organisation, 2008), Haynes et al (2009) devised a 19 item checklist intended to reduce the incidence of significant surgical complications. Checklists have a long-standing history within high risk industry and occupation, such as aviation, where a checklist was introduced in 1937 to overcome the acknowledged human error associated with flying a complex aeroplane that was continually modified to improve performance. Aviation is frequently compared to the peri-operative period in its demand for meticulous preparation and overcoming critical steps to achieve success (Weiser et al, 2010). It was therefore hoped that a similar regimen would prove useful to the surgical setting; studies have now shown this to be the case (Haynes et al, 2009; Haynes et al, 2011). Most strikingly, the use of the WHO SSC in human hospitals is linked with the reduction of both peri-operative complications and deaths by over a third (Haynes et al, 2009). Additionally, nearly all human healthcare professionals questioned in one study expressed that they would want the checklist used if they were undergoing surgery (Haynes et al, 2011). Following such positive results the National Patient Safety Agency (NPSA) adapted the checklist for use within England and Wales and mandatory use within the National Health Service was targeted for February 2010.
Core values of the SSC
Three distinct phases of care are covered by the SSC. ‘Sign in’ occurs before the induction of anaesthesia and focuses on consent, identification and agreement of surgical sites and the patient's needs with respect to safe anaesthesia practices. ‘Time out’ occurs immediately before the start of surgery and the checking steps are designed to share information about the patient's procedure and ensure all necessary equipment is available and functional. ‘Sign out’ is the final set of checking steps at the end of surgery, before the patient leaves theatre, where essential information about the procedure is recorded and a post-operative plan devised to facilitate care in recovery. It is beyond the scope of this article to discuss each step of the checklist sequentially, but in essence the checklist as a whole is designed to disseminate essential information pertaining to the patient and initiate a focused, meaningful and purposeful conversation between the OR team, with an overall aim of improving safety. As established above, poor communication within the surgical team is one of the most frequently cited root causes of error in the OR. It is proposed that by empowering the individual within a safety culture, SSCs help to diminish the hierarchical nature of staff working within the OR, allowing any team member to voice their concern if procedural policy is not followed.
Each section of the SSC should not take more than 1 to 2 minutes to complete. There is no specific requirement in how the SSC is conducted other than that it is read out aloud to the whole team, who should ideally pause any activity. Checklist steps either ask a question to the team, or state a matter of fact if it is known to be correct to the checklist coordinator. Throughout the checklist, discussion and concerns should be patient specific rather than general.
Criticisms and potential limitations of the SSC
Overall, the SSC is a tool that provides a framework to develop safer surgical practices. It should be acknowledged however, that it has been viewed by some as a tick box exercise (Vats et al, 2010; Walker et al, 2012). This criticism fails to acknowledge that the SSC cannot achieve success by working in isolation and that the most positive outcomes are encountered when the team works together and fully engages in a safety culture (Vats et al, 2010; Walker et al, 2012).
For example, it is interesting to note that although the SSC includes a specific section within the time out checklist confirming correct swab counts, incidences of retained swabs are still reported (Department of Health, 2012). It is asserted by the authors that retained swabs and other similar errors will still occur if the surgeon refuses to believe that a missing swab could be within the patient. In such a case, the SSC has failed to change behaviours if it is simply viewed as an exercise not requiring follow-up action. In the authors' experiences however, surgeons are more fully engaged with the counting process since the introduction of the SSC and in the event of a count discrepancy they will initiate a full exploration of the surgical site alongside other OR searches until the count is rectified. A topic for future discussion therefore is that of the continuing development of non-clinical or non-technical skills, which seek to further recognise and address the human factors which can contribute to scenarios such as the one described above.
Adaptation of the SSC for veterinary practice
The WHO SSC was not designed to be prescriptive. It encourages modification to suit local policy in recognition of the fact that different OR teams will inevitably work in different ways (World Health Organisation, 2009). Before modification however, it is essential to consider the value of each step added to, or omitted from, the checklist. For example, duplication of a step is not considered wasteful if each repetition serves a purpose.
The Animal Health Trust (AHT), a veterinary referral centre, introduced a modified SSC in November 2008 for all animals undergoing invasive procedures within the Small Animal Centre's theatre suite. Later it was modified for further use within all areas of the hospital for patients that needed to be sedated or anaesthetised. An example of the SSC for soft tissue and neurosurgery is shown in Figure 2; please note that further SSCs and a short implementation and user guide are available to download at www.aht.org.uk/cms-display/sa_resourecepsf.html
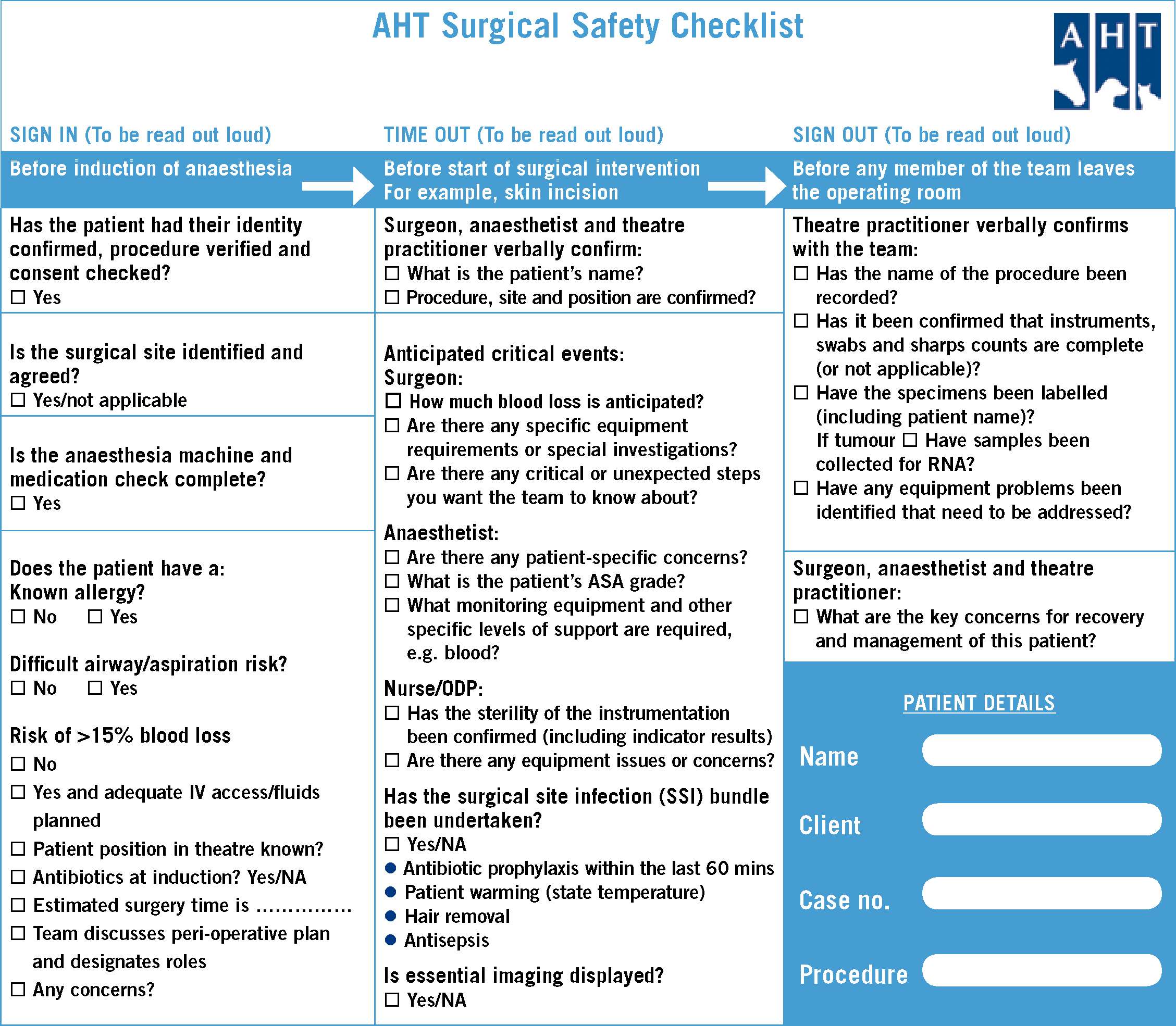
As illustrated in Figure 2, the AHT SSC follows a very similar format to the WHO SSC, with the inclusion of three stages of sign in, time out and sign out. Within the AHT ORs, it has been designated as routine that it is the circulating nurse who has responsibility for completing the checklist, although any member of theatre staff may initiate it.
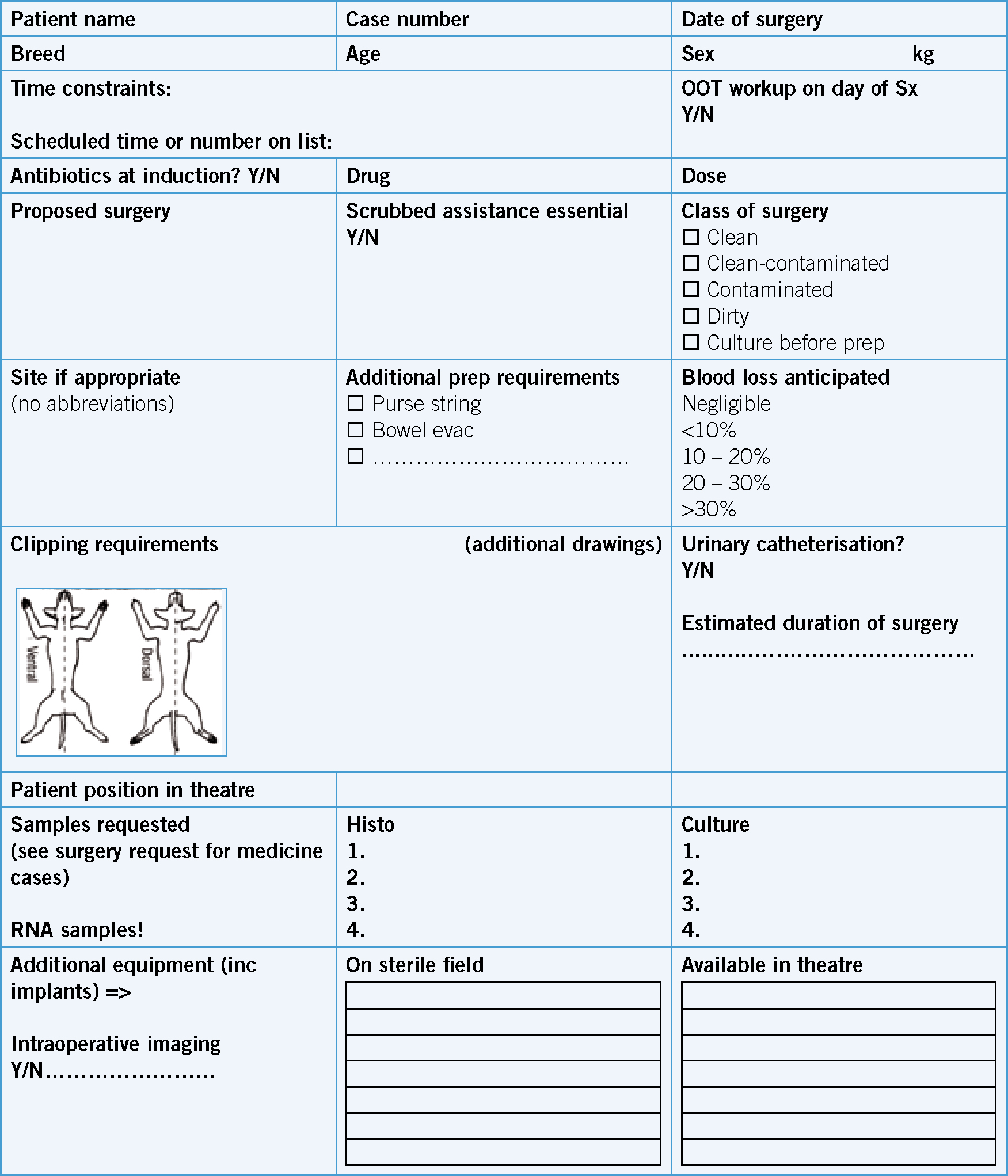
Although the WHO SSC fulfilled the requirements of the AHT, it became clear from the outset that additional information would be required from the admitting surgeon in order to complete the sign in phase. Ideally, the surgeon would be present for this process, or a team briefing to discuss the peri-operative plan for each patient would occur at the start of the day, as recommended by the National Patient Safety Agency (2010). Due to the time constraints of individual surgeons within the hospital however, this is not possible. A paper-based surgical request form was therefore devised to use alongside the SSC, in or der to fulfil this need, as shown in Figure 3. In smaller teams, this would be unnecessary.
Observations of using the SSC in practice
In the opinion of both of the authors, the implementation of SSCs within the AHT has been overwhelmingly positive, helping to ensure that all vital information regarding the patient and the procedure are transferred between all the attendant personnel. It is also felt that they bring unity to a work environment where multiple specialist teams are often working independently, as observed by Donaldson (2013):
‘The theatre nurse in charge of the checklists often needs to be stern to bring order to the proceedings, ensuring all the involved teams have a voice and importantly that that voice is heard. As a surgeon I feel that the effect of this initial checklist is immediate and that instead of having a theatre filled with independently operating teams, the staff become unified and focussed on common objectives, with an awareness of the other disciplines present, their roles, and more critically their concerns. Patient care benefits from the collective expertise of the staff present and the risk of problems arising from poor communication are minimised.’
Like any tool, the SSC must be reviewed and amended to include changes in practice. Similarly, critically reflecting on adverse events is an essential component of safer surgery. Following a fatal incident involving gastro-oesophageal reflux (GOR) during the intra-operative period of one patient at the AHT, a decision was made to review the use of the SSC and ensure that evidence-based remedial actions regarding the prevention and management of GOR were agreed in advance. As a result of this critical incident analysis, two further standard operating procedures were developed, both of which were subsequently incorporated into the AHT SSC sign in as supplementary items when ‘yes’ was answered to the question ‘Are you anticipating a difficult airway or increased risk of regurgitation/aspiration?’ Additionally, in recognition that GOR may occur at any stage of procedures, a review of issues concerning this complication was also added to the time out stage of the SSC for those patients assessed to be at risk. This ensures that the operating surgeon is also included in the discussion.
Recommendations for practice
It is asserted that veterinary practice, and most importantly veterinary patients, would benefit from the implementation of SSCs. The WHO SSC can be modified to suit any veterinary setting, following an appraisal of each step and the value it brings to the process.
Most healthcare professionals, both medical and veterinary, are familiar with the ‘five rights’ of drug administration (Grissinger, 2010). It is proposed that whatever the local modifications made to either the WHO or AHT SSCs, that the principal essence of establishing a similarly essential ‘five rights’ of peri-operative practice is maintained. These should include consideration of:
- The right patient
- The right surgical site
- The right procedure (both the correct surgical intervention and the one that has been consented to)
- The right provision of safe anaesthesia and correct surgical equipment and
- The right surveillance of patient asepsis, instrument sterility and swab, instrument and sharps counts.
The form that any such checklist takes can also be adapted to suit the needs of the individual practice. As a verbal checklist, it is designed to be brief and engage all members of the theatre team. The AHT checklists are printed and form part of the patient's permanent surgical record; the checklist could however be printed on a reusable whiteboard.
Conclusion and suggestions for further research
Due to the reduction it causes in serious surgical complications through enhanced teamwork and communication in the OR, the SSC is now considered an essential part of safe and responsible practice in human hospitals. As the similarities between the demands of medical and veterinary OR environments on which the SSC was devised, together with the positive experiences of utilising such checklists in the veterinary setting, have been established here, it is asserted that the SSC should be viewed as an equally important part of veterinary practice.
To finish by again echoing the thoughts of Tivers (2011), the authors propose that the veterinary profession would benefit from continuing to learn from their medical colleagues about the frequency and nature of surgical complications and how to reduce their incidence, in order to maximise the safety of our patients. Studies exploring these issues would therefore make useful additions to the literature.
Key points
- Many peri-operative complications are attributable to human factors such as failures in communication and teamwork.
- Surgical Safety Checklists were devised to address the human factors which can compromise patient safety.
- The use of Surgical Safety Checklists in the human healthcare setting is now routine practice and has been linked to improved outcomes.
- The World Health Organisation Surgical Safety Checklist can be successfully modified for use in veterinary practice.
