In the UK blood components (products), packed red blood cells, fresh frozen plasma, frozen plasma, cryo-precipitate and cryo-supernatant have only been available since the emergence of blood banks 5 years ago. This has led to advancement in transfusion medicine and a positive outcome for thousands of patients whose previous treatment options were restricted due to the lack of available blood. To date in the UK only canine blood products are available with feline transfusion patients being restricted to the option of fresh whole blood donated from emergency donors at the time.
With blood products now more widely available a greater understanding of using them becomes ever more important not only to ensure transfusions are being carried out safely but also to make best use of the blood donated by donors volunteered by their owners. Blood typing and cross-matching are two screening tests recommended to be performed prior to canine and feline transfusions.
Blood typing background
Dogs and cats, like humans, have blood types — these are species specific.
Dogs
The different canine blood types are described as Dog Erythrocyte Antigens (DEA). In simple terms these are markers on the surface of the red cells. There are eight DEA antigen systems 1.0, 3, 4, 5, 6, 7, 8 and Dal that have been determined through studies to have the potential to cause acute or delayed immunological transfusion reactions (Table 1). There may be many more that have not been defined. Dog blood group systems are inherited independently which allows them to coexist on the surface of the red cell allowing dogs to have more than one blood type.
| Canine blood group system | Antigen phenotypes | Population prevalence | Incidence of naturally occurring antibody | Comments |
|---|---|---|---|---|
| 1.0 | 1.1, 1.2, 1.3, null | 62%, 2%, 0.1% | < 2% | Commercial typing system available for 1.1 only |
| 3 | 3, null | 5% | 8–15% | |
| 4 | 4, null | 98% | Rare | |
| 5 | 5, null | 15% | 8–12% | |
| 6 | 6, null | 96% | Unknown | No available typing system |
| 7 | 7, null | 40–55% | 10–40% | |
| 8 | 8, null | 20–40% | Unknown | No available typing system |
| Dal | Dal, null | 99% | Rare | No commercial typing system |
*Data to be published in 2012 by Pet Blood Bank UK indicates a higher percentage of DEA 1.1 positive dogs in their donor population.
For the purpose of this article the author will concentrate on the only canine blood type that testing is widely available for and that has the most transfusion significance in terms of acute immunologic transfusion reactions: DEA 1.1.
Dogs are either described as DEA 1.1 positive where there is 1.1 antigen on the surface of the red cells or DEA 1.1 negative where no 1.1 antigen is present on the surface of the red cells. Three commercial typing test kits are available to veterinary practices to use ‘in house’ with one of the most common being described in detail in the Step-by-step guide of this article. With regards to the other blood group systems, identification of these is limited to individual laboratories that are internationally distributed, mainly in the USA. Extended typing is of use when dealing with complex multiple transfusion patients and transplant patients. Most of the research into canine blood types used today was performed in 1949 (Young et al, 1949). The science of companion animal immunohaematology will continue to develop as there are a lot of unanswered questions making transfusion medicine an ever-evolving field in the veterinary profession.
Cats
Feline blood groups are inherited. Our understanding is that they have a relatively simple blood group system. Feline blood groups are described as A, B or AB blood type (Day, 2012).
There are three alleles that control the AB blood type. The A allele is dominant over the b allele and the phenotype AB is the result of the third allele (aab) this allows codominance expression of both A and B. Cat breeders are likely to ask for their breeding cats to be blood typed due to its importance in reducing neonatal isoerythrolysis in their kittens. The prevalence of blood types varies with breed and also by country, refer to Table 2 supplied by Feline Advisory Bureau for Type B breeds and www.fabcats.org for more information.
| Only type A | Low type B frequency (1–10%) | Intermediate type B frequency (10–25%) | High type B frequency (>25%) |
|---|---|---|---|
| Siamese* | American Shorthair* | Abyssinian* | British Shorthair*^ |
| Tonkinese* | Maine Coon* | Birman*^† | Cornish Rex* |
| Oriental Shorthair* | Manx* | Burmese ^ | Devon Rex*† |
| Norwegian Forest* | Himalayan* | Exotic* | |
| Bengal** | Persian*^ | Ragdoll* | |
| Scottish Fold* | Turkish Van* | ||
| Somali* | Turkish Angora * | ||
| Sphynx*† |
Compatibility
Identifying blood type antigens is one part of compatibility; the other is ensuring any blood given is not going to be removed from the patient's circulatory system prematurely. Alloantibodies are antibodies that are made against antigens occurring naturally within the same species. Alloantibodies attach to antigens on red cells and may initiate a process that causes destruction or removal of any transfused red cells containing that antigen. Alloantibodies can be naturally occurring or occur due to previous sensitizing to a foreign antigen generally 4–7 days post exposure.
Dogs
Dogs rarely have any naturally occurring alloantibodies in their circulation (Table 1). Sensitization from a previous transfusion with incompatible blood is the main cause of alloantibodies.
On first transfusion DEA 1.1 positive blood should only be administered to a DEA 1.1 positive patient to prevent sensitizing the DEA 1.1 negative patient to the foreign 1.1 antigen and thus creating the potential for production of alloantibodies. Subsequent administration of DEA 1.1 positive blood to a sensitized DEA 1.1 negative patient can produce an acute immune-mediated transfusion reaction which is potentially life threatening and must be avoided by ensuring the correct blood type is administered.
DEA 1.1 negative blood should be administered to DEA 1.1 negative patients. Although no adverse effects occur when administering DEA 1.1 negative blood to a DEA 1.1 positive patient, DEA 1.1 negative donors make up just over 30% of the dog population presented as donors. Using DEA 1.1 negative blood on DEA 1.1 positive patients has ethical and welfare implications, most poignantly it means stocks of DEA 1.1 negative blood could subsequently be depleted to a level that makes it unavailable to DEA 1.1 negative patients (Table 3).
| Donor blood type | Patient blood type | |
|---|---|---|
| DEA 1.1 negative | DEA 1.1 positive | |
| DEA 1.1 negative | Yes | Emergency only — will deplete valuable stock levels |
| DEA 1.1 positive | No will sensitize patient | Yes |
Cats
Unlike dogs, A and B cats develop naturally alloantibodies to other blood groups within the first few months of life (AB cats do not) (Knottenbelt et al, 1999). This means cats are at great risk of transfusion reaction if blood typing is not performed prior to the initial transfusion to allow the correct blood type to be administered. Basic compatibility in cats is illustrated in Table 4.
| Donor blood type | Patient blood type | ||
|---|---|---|---|
| A | B | AB | |
| A | OK | May be fatal | Possible reaction |
| B | Reaction | OK | Reaction |
| AB | Reaction | May be fatal | OK |
Type A cats generally have low levels of anti-B alloantibodies in their serum whereas type B cats usually have high levels of anti-A alloantibodies in their serum; AB type cats have no alloantibodies to either A or B however donors are hard to find. Due to the low level of anti-B alloantibodies in serum if a search for a rare AB type matched donor is unsuccessful, it is recommended to use a type A donor for transfusion, some reaction will be seen. Type A packed red cells or washed type A red blood cells would be even better — however these are not usually available or produceable in general veterinary practice.
In-house available blood typing tests
Step-by-step guide to typing
Step 1 (Figure 1)
Step 2 (Figure 2)
Step 3 (Figure 3)
Step 4 (Figure 4)
Step 5 (Figure 5)
Step 6 (Figure 6)
Step 7 (Figure 7)
Step 8 (Figure 8)
Step 9 (Figure 9)









Cross-matching
Dogs
As discussed in the introductory typing section above, dogs have many blood types that can coexist on the surface of their red cells and with the absence of in-house testing kits for all of these blood types, DEA 1.1 is the only status a general practitioner can detect quickly and easily. It must be assumed that even when DEA 1.1 typed blood is given correctly to patients there is still the potential to introduce other antigens that may be seen as foreign and that in turn the patient may create antibodies against them (Young et al, 1949). It is therefore recommended in dogs to perform a cross-match prior to transfusion if:
Cats
Cats are likely to have additional blood types recognized as transfusion medicine advances, as an example in 2007 the Mik antigen was discovered (Weinstein et al, 2007) and no in-house testing kits are available to date. For these potential rare instances cross-matching cats prior to any transfusion is recommended.
Cross-matching techniques
Cross-matching is an in vitro test that looks for potential reactions between a donor's and patient's blood, these show as agglutination or haemolysis. Agglutination is more commonly seen in canine incompatibilities — haemolysis is less common. In cats both agglutination and haemolysis can be seen.
Performing a cross-match for dogs with immune-mediated haemolytic anaemia can be challenging due to background agglutination and haemolysis. It is therefore recommended to transfuse the patient with red cells that are the ‘most’ cross-match compatible in these circumstances.
The cross-match test required depends on the type of product being transfused: major cross-match for red cell products and minor cross-match for plasma products. Anticoagulated whole blood contains both red blood cells and plasma therefore performing both a major and minor cross-match is recommended when administering whole blood:
Step-by-step guide to cross-matching
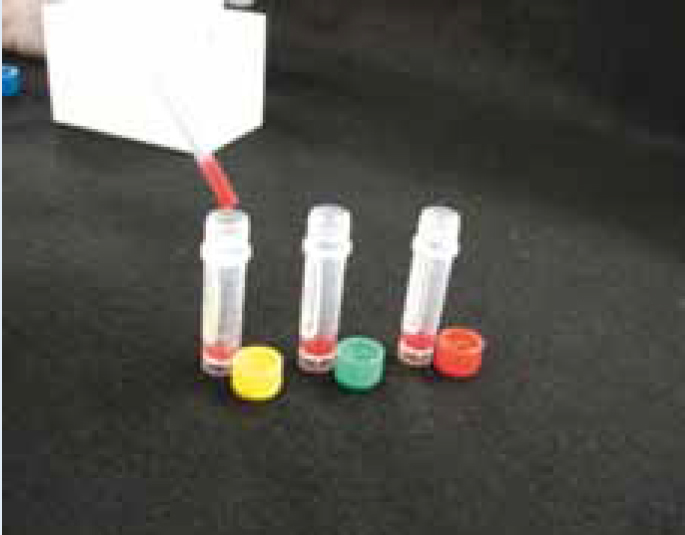
Test requirements (Figure 1)
Step 1 (Figure 2)
Step 2 (Figure 3)
Step 3 (Figure 4)
Step 4 (Figure 5)
Step 5 (Figure 6)
Step 6 (Figure 7)
Step 7 (Figure 8)
Step 8 (Figure 9)
Step 9 (Figure 10)
Step 10 (Figure 11)
Step 11 (Figure 12)
Step 12 (Figure 13)
Step 13 (Figure 14)













Cross-matching can be performed in a laboratory with minimal equipment and takes up to 60 minutes or an in-house gel cross-match kit that identifies agglutination reactions is simple to use, and provide a quicker solution taking 15–20 minutes to perform. Alternatively blood from both donor and patient can be submitted to many commercial laboratories for cross-matching but this can take up to 24–48 hours before results are available.
In-house available cross-matching tests
Conclusion
In house, clinically relevant blood typing is a quick and easy procedure that reduces the risk of transfusion reactions and should be performed in both dogs and cats prior to initial transfusion. Cross-matching should be considered in all feline patients due to the discovery of the Mik antigen and other undiscovered antigens that are thought to exist. All canine patients where time allows should have a cross-match performed as gold standard however this is often not practical. It is however essential if a canine patient requires a subsequent transfusion and has received blood products more than 4 days previously.
