Canine visual impairment is commonly presented in first opinion practice resulting from a variety of acute and progressive diseases or trauma. With pets living much longer because of scientific advances in medicine and nutrition, age-related ocular conditions are also seen more frequently (Pandey et al, 2018). Registered veterinary nurses (RVNs) play a crucial role in helping owners understand why their dog has developed ocular impairments and what options are available to help the dog adjust to visual impairment.
Canine visual impairment and blindness are usually well-tolerated, and dogs can adapt well with minor adjustments to their lifestyle. RVNs are often involved in behaviour and training techniques and should be able to provide considerate and ethical advice and support. Often, owners find the subject very emotional and imagine themselves being blind and the implications it would have on their lives.
Vision loss can occur acutely or manifest gradually; acute onset vision loss is usually very noticeable and clients will often report disorientation, clumsiness and the dog being easily startled or nervous (Sheldon, 2012). However, gradual vision loss can be harder for the owner to notice and may only be picked up during routine veterinary consultations or nurse clinics. Signs of gradual vision loss that the owner may notice include: changes in the appearance of the eyes; struggling to navigate in the dark; and walking more slowly or cautiously.
Causes of gradual vision loss
An example of a disease which can cause gradual vision loss is progressive retinal atrophy, a group of hereditary conditions which result in progressive degeneration of the retina and loss of vision (Jeong et al, 2013). Owners may notice subtle changes to the appearance of the eyes, such as abnormally dilated pupils and increased reflection from the eye known as tapetal hyper-reflectivity. Owners may also note night blindness (nyctalopia) as the initial changes as a result of progressive retinal atrophy is the loss of rod photoreceptor responses leading to difficulty seeing at night (Narfstrom et al, 2013). Although harder to notice than mature cataracts, owners may notice the development of secondary posterior cataracts which commonly occur in the advanced stages of progressive retinal atrophy (Park et al, 2009; Jeong et al, 2013)
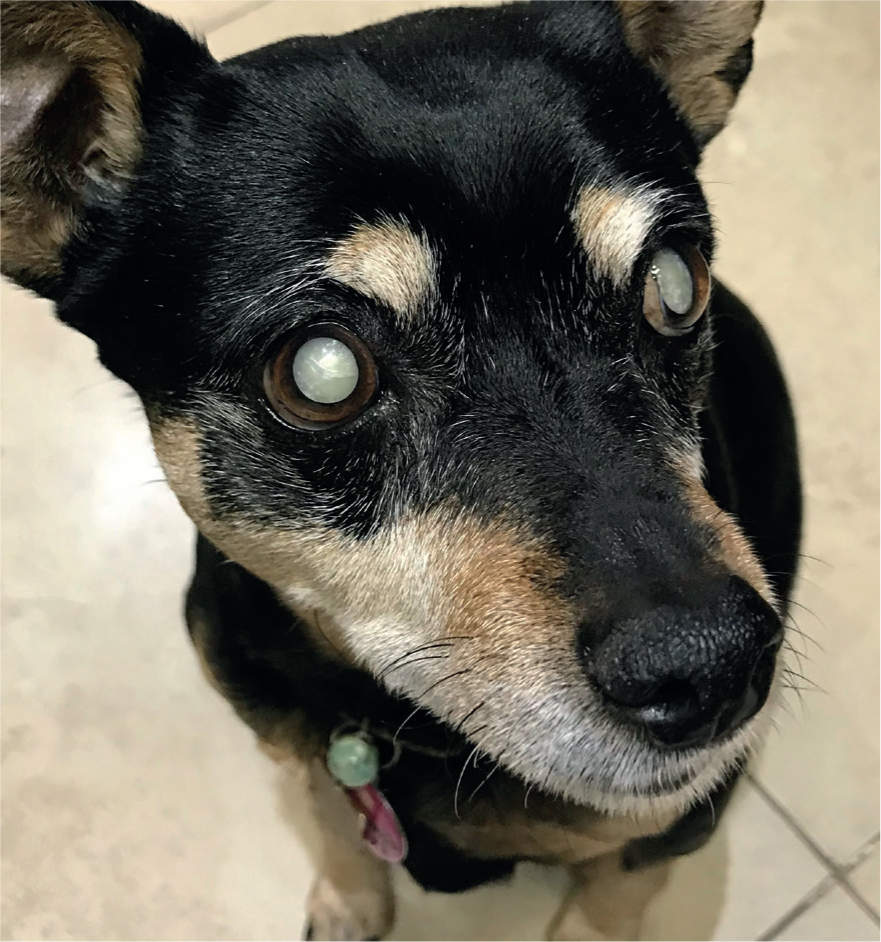
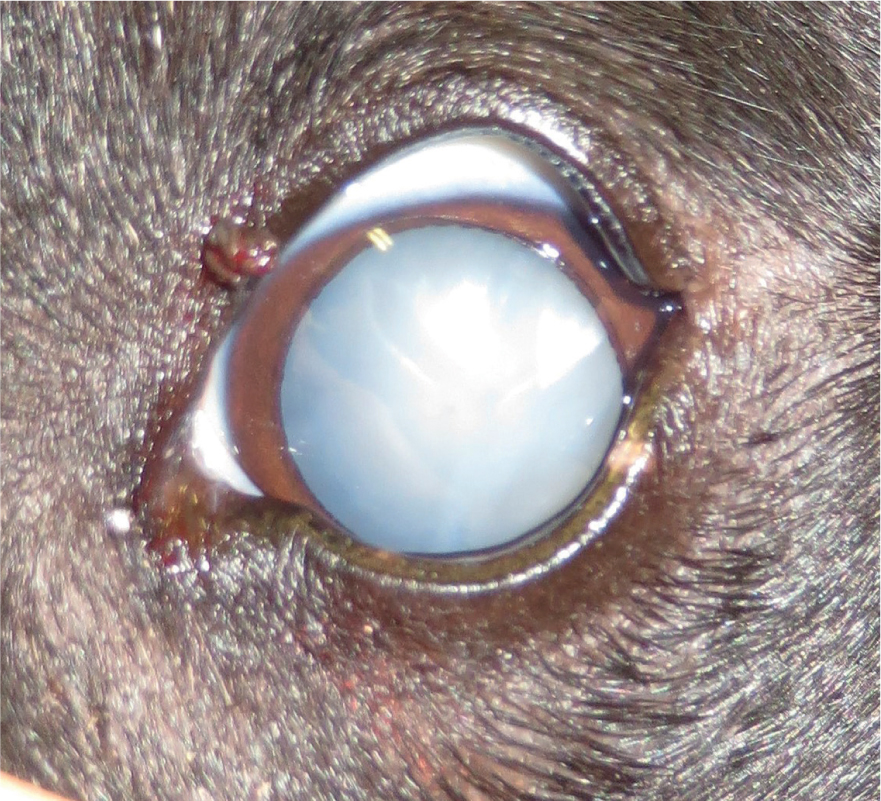
Cataracts are another common cause of visual impairment and blindness in dogs (Gould, 2002). Cataracts have a highly variable nature and appearance and can be classified according to their progression, location, age of onset and aetiology (Fischer, 2019). Owners may report ‘cloudiness’ or opacity of the lens or a grey appearance of the eyes accompanied by gradual or acute vision loss (Figures 1 and 2).
Causes of acute vision loss
Acute vision loss is often very abrupt and disconcerting for all involved, and clients may make hasty conclusions with regards to the treatment options. A dog presented for acute vision loss should be examined with patience and care; a full ophthalmic examination and a thorough diagnostic approach is vital for these patients. RVNs can assist the veterinary surgeon (VS) by obtaining a full ophthalmic history including when the vision loss was first noticed, if there have been any changes in the appearance of the eyes and any behaviour changes (Plummer, 2016). Under veterinary direction, RVNs are able to assist in ophthalmic examination by performing basic vision assessments, including Schirmer tear testing and tonometry, however, results should be relayed to the VS for diagnosis (Table 1). It is important to note that some elderly dogs or those with neurological disease may behave as if they have vision loss although their visual systems are functional; thus, a thorough ophthalmic examination with a VS or ophthalmologist is necessary (Plummer, 2016).
Table 1. Routine ophthalmic tests
| Menace response | The menace response test is performed by making a ‘menacing’ gesture with the hand towards the patient's eye, blink is a positive indication of functioning central and peripheral ophthalmic systems (take care to not touch the patient because excessive air movement which could induce a false-positive result) |
| Maze tests | An obstacle course to assess vision in daylight and dim conditions, obstacles should be adjusted to avoid memorisation and mapping |
| Cotton wool test | Cotton balls tossed into the visual field to assess the patient's visual placing response |
| Schirmer tear testing | The measurement of test tear production for the diagnosis of keratoconjunctivitis sicca (KCS), normal tear production is between 15–25 mm/min |
| Tonometry | The measurement of intraocular pressure for the diagnosis of glaucoma, normal intraocular pressure is between 15 mmHg and 25 mmHg |
The VS may also choose to perform blood pressure testing, ocular ultrasonography and an electroretinogram (ERG) to further support their diagnosis (Webb and Cullen, 2013). Ocular ultrasound is an essential tool in ophthalmology, if the fundus cannot be visualised because of cataractous lenses, vitreal haemorrhage or inflammation. Ocular ultrasound can aid with the assessment of ocular haemorrhage, retinal detachment and ocular neoplasia (Bentley et al, 2003; Dar et al, 2014). Furthermore, an ERG is a reliable diagnostic tool which measures electric potentials occurring in the retina in response to light stimulation, it may be used to differentiate vision loss caused by retinal disease from that caused by optic nerve disease (Ofri, 2002; Ekesten, 2013).
A dog presented for acute blindness should always be considered an emergency as vision can potentially be restored with rapid and appropriate management (Busse, 2012). Glaucoma, diabetic cataracts, deep corneal ulceration, severe uveitis, intraocular haemorrhage and anterior lens luxation should all be considered ocular emergencies (Plummer, 2016); there are a number of prevalent blinding conditions including cataracts, progressive retinal atrophy and sudden acquired retinal degeneration syndrome (SARDS), which should be examined urgently. With improvements in veterinary care and referral widely available, clients have the option for specialist ophthalmic surgery to treat blinding conditions. There are a number of advanced ophthalmic surgical interventions for blinding conditions, such as cataract extraction surgery by phacoemulsification, retinal detachment surgery and laser endoscopic cyclophotocoagulation (ECP).
A notable disease that RVNs may have significant involvement in is glaucoma: canine glaucoma is characterised by the elevation of intraocular pressure (IOP) with associated optic neuropathy and retinal damage (Figure 3) (Turner, 2010; Komaromy and Petersen-Jones, 2015). Canine glaucoma is not a single disease entity, rather ‘the glaucomas’ should be considered to represent a large, diverse group of disorders (Gelatt et al, 2008). However, ‘the glaucomas’ share a unified final pathway of characteristic optic neuropathy and retinal damage resulting in loss of vision (McLellan and Miller, 2011; Komaromy et al, 2019). Canine glaucoma is a leading cause of irreversible vision loss and can be classified by the underlying cause of impaired aqueous humor drainage and the duration of glaucoma (Reinstein, 2019). Despite advancements in medical and surgical treatments, there is no known cure and affected dogs often have eyes enucleated because of painfully high, uncontrollable IOP (Komaromy et al, 2019).

RVNs can provide thorough information in layman's terms to allow owners to understand that the aim of medical or surgical therapy is to stabilise the IOP. Although there is no cure for glaucoma, owner compliance with medical management can prevent further vision loss and control pain. Poor compliance or poor understanding of the condition before starting a treatment plan can lead to inadequate IOP control and enucleation of blind, painful eyes (Ofri, 2019). However, in cases of primary glaucoma, medications become less effective over time and the IOP will continue to rise (Reinstein 2019). Therefore, advanced surgical procedures such as ciliary body laser ablation or anterior chamber shunts should be considered for visual patients, while blind patients may eventually require enucleation (Figure 4).

Assessing the quality of life of visually impaired dogs
Unfortunately, there are a number of blinding conditions which cannot be reversed including SARDs, retinal atrophy and glaucoma (Turner, 2005; Plummer, 2016). Discussion regarding euthanasia is probable in these situations as dogs with acute blindness often present abruptly and owners are often distressed. Understandably, owners often have empathy for their dog and imagine themselves being blind and the implications it would have on their lives. However, many dogs cope remarkably well with blindness and are able to maintain a good quality of life (Knott, 2020). It is often the blind painful patients that cope poorly; RVNs should use quality of life (QoL) tools and good communication skills to reassure owners that although acute blindness presents abruptly, dogs can adapt well to their new lifestyle.
RVNs are often involved in assessing a dog's QoL, and there are a number of QoL tools which can be used prior to implementing a treatment plan (Yeates and Main, 2009; Villalobos, 2011). QoL assessments aim to provide a methodical and ethical evaluation of animal welfare, they have the potential to identify welfare deficiencies and allow RVNs and VS to target improvement strategies (Mullan, 2015).
The HHHHHM is a quantitative QoL scale which stands for hurt, hunger, hydration, hygiene, happiness, mobility, and more good days than bad (Villalobos, 2011; Table 2). The HHHHHMM scale is easy to implement and provides useful guidelines for owners to follow and understand their dog's QoL. A score of above 35 points is an acceptable quality of life for pets; however, when using this QoL scale to assess a visually impaired dog's lifestyle it is also important to focus on individual factors such as happiness and mobility. If the dog is displaying depressed, anxious or aggressive behaviours which are significantly impacting the dog and owners lifestyle then the scale may not be relevant for that patient. It is also important to assess how the treatment plan will affect the patient; many ophthalmic conditions require multiple topical medications applied daily, which may cause significant distress and changes in behaviour in nervous dogs.
Table 2. HHHHHM QOL Scale
| Quality of Life Scale: The HHHHHMM ScaleAdapted from: Villalobos (2011). | |
|---|---|
| Criterion | Score (1–10) 10 being the highest quality of life) |
| Hurt: Adequate pain control, including breathing ability, is first and foremost on the scale. Is the pet's pain successfully managed? Is oxygen necessary? | |
| Hunger: Is the pet eating enough? Does hand feeding help? Does the patient require a feeding tube? | |
| Hydration: Is the patient dehydrated? For patients not drinking enough, use subcutaneous fluids once or twice daily to supplement fluid intake. | |
| Hygiene: The patient should be brushed and cleaned, particularly after elimination. Avoid pressure sores and keep all wounds clean. | |
| Happiness: Does the pet express joy and interest? Is the pet responsive to things around him or her (family, toys, etc.)? Is the pet depressed, lonely, anxious, bored or afraid? Can the pet's bed be close to the family activities and not be isolated? | |
| Mobility: Can the patient get up without assistance? Does the pet need human or mechanical help (e.g., a cart)? Does the pet feel like going for a walk? Is the pet having seizures or stumbling? (Some caregivers feel euthanasia is preferable to amputation, yet an animal that has limited mobility but is still alert and responsive can have a good quality of life as long as caregivers are committed to helping the pet.) | |
| More good days than bad: When bad days outnumber good days, quality of life might be compromised. When a healthy human–animal bond is no longer possible, the caregiver must be made aware the end is near. The decision needs to be made if the pet is suffering. If death comes peacefully and painlessly, that is okay. | |
| *A total over 35 points represents acceptable life quality | |
Behaviour changes
There are a number of behaviour changes which a visually impaired dog may display which can be discussed with a RVN or a behaviourist. How a dog adjusts to vision loss will depend on the speed of onset, the severity of the loss and the individual temperament of the dog. Because of the disruptive onset of acute blindness, dogs will often display abrupt behaviour changes such as clumsiness, nervousness and being easily startled (Turner, 2005). Nervous behaviour as a result of vision loss may also lead to aggression towards the owner (Gerrard, 2013). Dogs can appear to be in a depressive state, which is expressed by sleeping excessively and limited interaction with the owner (Turner, 2005). On the other hand, gradual blindness is much more likely to cause progressive behaviour changes, such as difficulty navigating in unknown environments and little interest in games or toys. It is important to note that any behaviour changes may apply to acute or gradual blindness depending on the dog.
Adaptation to lifestyle
Generally, dogs rely less on vision than sound and smell; a dog's vision lacks visual acuity compared with humans, meaning that they rely more on shape, movement and contrast between light and shade than detail (Byosiere et al, 2017). Often the transition and adaptations implemented are more difficult for the client than the dog. Adaptations that can be implemented include maintaining a consistent environment, and modifying the methods of communication and training commands. It is important to discuss the value of maintaining a consistent home environment — dogs are capable of ‘mapping’ their environment and are less likely to bump into furniture and become disorientated if the home environment is kept the same. Clients can also leave a quiet radio on where the dog spends the most time, as they will be able to map where the sound originates from to navigate around the home. RVNs should also reinforce the recommendation not to move the dog's food and water bowls as they may stop eating and drinking if they are unable to locate them.
Owners can encourage their dog to utilise the remaining senses to enable stress-free navigation and the ability to express normal behaviour. Training a visually impaired dog can take time and patience; it is important to be consistent and positive with any routines implemented (Dogs Trust, 2020). Touch should always be a positive experience when training a visually impaired dog; it is essential to approach the dog calmly to allow the dog to use their other senses to adapt before any interaction. Owners can also teach verbal commands such as ‘step-up, step-down’ and directional commands such as ‘this way, forward, wait’ to guide the dog when in an unknown environment.
There are a number of resources and tools which an owner can be referred to, directing owners to web resources and support groups can provide inspiration and show how dogs can cope well with visual impairment (PDSA, 2020, BDRUK, 2020). Charities such as the People's Dispensary for Sick Animals (PDSA) and Blind Dogs Rescue UK (BDRUK) have a number of web resources including caring for blind dogs and inspirational stories. Moreover, there are ‘bumper guards’ available for visually impaired dogs which allow them to navigate without injuring, frightening or losing confidence in themselves by bumping into unseen objects (Muffins Halo Guide for Blind Dogs, 2020, Figure 5).

Conclusion
Canine vision loss, whether acute or gradual, should be considered an emergency or urgent case, and warrants prompt evaluation by a VS or ophthalmologist. RVNs can help throughout the diagnosis and treatment of a visually impaired dog, both clinically and through client support. In some cases, prompt medical treatment can result in the return of vision, however, RVNs should be prepared to provide guidance and support for owners to adjust to life with a visually impaired dog, while keeping the dog's health and welfare a priority.
KEY POINTS
- Registered veterinary nurses (RVNs) must be able to communicate effectively with owners regarding the care of a visually impaired dog to ensure the patient has a good quality of life.
- RVNs should have a thorough understanding of the disease processes of canine visual impairment to be able to discuss canine blindness, treatment options and educate clients.
- Maintaining routines, providing a safe environment and supportive therapies can reduce anxiety and stress while visually impaired dogs adjust to the change.


