Hyperthyroidism is a common endocrine disorder of the cat where there is an excessive production of thyroid hormones (thyroxine (T4) and triiodothyronine (T3)), from the thyroid gland that circulate in the body resulting in clinical signs related to hyperthyroidism. Hyperthyroidism is the most common endocrinopathy in cats with a reported median age of 12-13 years at time of diagnosis (Peterson, 2012) (Table 1).
| Feline | Canine |
|---|---|
|
|
|
Feline hyperthyroidism is usually the result of a functional adenomatous hyperplasia of thyroid tissue involving in approximately 70% of hyperthyroid cats both thyroid lobes (Lucke, 1964; Leav et al, 1976; Wakeling et al, 2005).
Functional adenomatous hyperplasia is present in approximately 95% of the cases (Peterson, 1981; Peterson, 2007; Mooney and Peterson, 2012; Baral and Peterson, 2012). By contrast thyroid carcinoma is affecting less than 5% of the feline hyperthyroid population (Turrel et al, 1988; Hibbert et al, 2009; Peterson, 2011a; Peterson and Broome, 2012). Biopsies obtained from thyroid lobes of hyperthyroid cats, have revealed the presence of mixed adenomatous and carcinoma tissues (Hibbert et al, 2009).
Development of hyperthyroidism is thought to be affected by many factors including contaminants in food or water or environment factors (Table 2). Contributing factors thought to be related to development of hyperthyroidism include:
| Mechanism | Effects | Site(s) of action | |
|---|---|---|---|
| Iodine deficiency | Iodine needed as substrate for thyroid horomone synthesis | Decreased synthesis of T4 and T3, high TSH | Thyroid gland |
| Soy isoflavones Herbicides Methimazole | Inhibition of thyroid peroxidase in thyriod follicles | Decreased synthesis of T4 and T3, high TSH | Thyroid gland |
| PCBs Flame retardants Phthalates | Competitive binding to thyroid horomone binding protein | Decreased thyroid horomone delivery to brain | Bloodstream |
| PBDEs | Altered transport across cell membrane | Increased biliary elmination of thyroid hormones | Liver |
| FD&C red dye #3 PDBs Selenium deficiency | Inhibition of deiodinase activity | Decreased peripheral T3 synthesis | Peripheral tissues (kidney and liver) |
| BPA PBDEs PCBsT | Thyroid receptor antagonist | Altered binding of T3 to thyroid hormone receptor, with altered activation of thyroid hormone-dependent gene transcription | Brain pituitary gland peripheral tissues |
| Pesticides PCBs | Inhibition of TSH receptor | Decreased production of T4 and T3 | Pituitary gland |
PCBs, polychlorinated biphenyis; PBDEs, polybrominated diphenyl ethers; BPA, bisphenol A; TSH, thyroid stimulating hormone
Iodine is an essential component of thyroid hormones. In addition, in human studies it has been shown to help the immune function with its antioxidant and anti-inflammatory properties (National Research Council, 2001; Soriquer et al, 2011). A case controlled study by (Edinboro et al, 2004) revealed that cats eating commercial low iodine or iodine deficient diets were more likely to develop hyperthyroidism compared with cats that ate iodine supplemented foods. Recommended daily iodine requirement for cat foods is 460 µg/kg dry diet for adult cats (Wedekind et al, 2010).
Veterinary nurses are often the first contact when a client telephones the surgery for advice. Understanding the clinical signs of hyperthyroidism will allow the nurse to advise the owner appropriately. The initial consultation would typically cover a physical examination of the cat and history documentation by the veterinary surgeon. A full blood work up including total T4 (TT4) levels if hyperthyroidism is suspected and blood pressure measurement is recommended. Once blood results have been received and hyperthyroidism is confirmed, further investigations are recommended, such as radiographs of the thorax, to check if the heart is enlarged, radiographs and ultrasound of the abdomen to check for metastases, and an echocardiogram if necessary prior to treatment.
This article will focus on the main body systems affected by hyperthyroidism, diagnostic tests, treatment options, radiation safety and nutrition.
Clinical signs
Gastrointestinal tract
Hyperthyroid cats often have a ravenous appetite with weight loss which is due to an increased metabolic rate. This increased metabolic rate is caused by increased levels of T3 and T4 which increases energy usage. Initially glucose stores are used, but once depleted the body catabolizes muscle protein to amino acids so that the amino acids can be converted by the liver to an additional source of glucose. This catabolism of muscle protein results in atrophy, which can be best seen along the lumbar spine.
Hyperthyroid cats often eat fast and gulp their food down due to their ravenous appetite. This may cause gastric distension and could lead to vomiting.
Renal system
Polyuria and polydipsia are seen in less than 50% of hyperthyroid cats but can be marked in some (Broussard et al, 1995). The high levels of thyroid hormones increase the glomerular filtration rate (GFR) forcing more water and solutes into the nephron, which alters the sodium concentration in the renal medulla (‘medullary wash out’) reducing the ability of the kidney to concentrate the urine, and causing electrolyte abnormalities.
Chronic kidney disease is often seen in older cats (Polzin, 2011). The hyperthyroidism causes increased filtration at the glomerulus, the overall GFR and elimination of metabolic wastes remains within normal limits even though there is a reduced number of functional nephrons. Therefore once euthyroidism has been restored and the effect of the hyperthyroid state on the kidney has been removed, the normal level of filtration results in a lowering of the GFR, accumulation of urea and creatinine, which unmasks the underlying chronic kidney disease.
This emphasises the importance of monitoring the renal function as well as the response to anti-thyroidal medication, before a definitive treatment like thyroidectomy or radioiodine therapy is considered (see below).
Cardiovascular system
The excess thyroid hormone produced by the metabolic state of hyperthyroidism is known to cause significant cardiovascular effects (Connolly et al, 2005). Auscultation of the heart may reveal tachycardia and systolic murmurs. The most common cardiovascular consequences of hyperthyroidism are hypertrophic cardiomyopathy (HCM) and systemic hypertension, both of which are usually controlled when euthyroidism is achieved.
Hyperthermia/stress intolerance
Hyperthyroid cats can be sensitive to heat; due to the increased metabolic rate this may cause mild elevation of body temperature (Mooney and Peterson, 2012). Hyperthyroid cats are not tolerant to stress and are normally anxious (Thoday and Mooney, 1992). When held for examination by the veterinarian, this can prove difficult as these cats can become aggressive with physical restraint. Often less restraint is more effective in the hyperthyroid patient.
Apathetic hyperthyroidism
Apathetic hyperthyroidism does not show the usual clinical signs relating to the hyperthyroid state, e.g. hyperactivity, restlessness, polyphagia. The clinical signs of apathetic hyperthyroidism are lethargy, anorexia, weight loss, depression and weakness.
Apathetic hyperthyroidism is an occult form of hyperthyroidism where there are other concurrent illnesses (e.g. renal failure, heart failure or neoplasia), which account for the clinical signs. The underlying disease will need to be treated independently to the hyperthyroidism, as only restoring euthyroidism will not resolve the other problems.
Diagnostic tests
The diagnosis of feline hyperthyroidism in most cases is confirmed with an elevated serum concentration of TT4 (Broussard et al, 1995; Baral and Peterson, 2012; Mooney and Peterson, 2012).
Fluctuations of serum TT4 concentrations can happen in cats with mild hyperthyroidism (Peterson et al, 1987). These fluctuating levels can be at the low to middle, or normal to high reference range. This may be due to concurrent illness; the concurrent disease is stabilised first, once this has resolved, serum TT4 concentrations will increase again. Therefore, TT4 tests should be repeated either in a couple of weeks and/or 2 to 6 months depending on the severity of the clinical signs. Patients with serum TT4 results remaining in the high to normal reference range after re-testing and the concurrent disease resolved, may require further tests.
Once the concurrent disease has been stabilised and TT4 results have been re-tested and are still inconclusive, then further diagnostic tests can be performed to aid with diagnosis. Free T4 can be measured along-side TT4, not alone, as the specifity of the test can be unreliable and give a false positive Thyroid stimulating hormone (TSH) test can help diagnosis of feline hyperthyroidism; however kits have only been devised for canines (Ferguson et al, 2007; Wakeling et al, 2008a; Wakeling, 2010; Wakelin et al, 2011; Ruiz-Drebing et al 2012). Hyperthyroid cats usually have a low TSH reading or it is not detectable (Wakeling et al, 2008a; Wakeling, 2008b; Wakeling, 2010; Wakeling et al, 2011; Ruiz-Drebing et al, 2012). Testing TSH must be accompanied by TT4 and T4. Triiodothyronine suppression test can also be included in the thyroid panel; the disadvantage is owner compliance in administering the medication.
The diagnostic results must be evaluated with the cats clinical signs, (especially weight loss with an increased appetite and a palpable thyroid nodule) and history before a diagnosis can be confirmed (Peterson, 2013).
Scintigraphy is also useful to diagnose hyperthyroidism by thyroidal uptake of radioisotope (e.g. technetium) by the hyperactive tissue. In addition, it can provide information on ectopic thyroid tissue, and sometimes will provide additional support for a thyroid carcinoma if functional metastases are detected. This will show the extent of spread of disease and help decide which therapy is best for this patient (e.g. surgical thyroidectomy or radioiodine treatment) as medical management will not control the metastatic disease.
Alongside the TT4, the minimum database should include haematology, serum biochemistry and urinalysis in order to assess the general health of the patient. Elevated liver enzyme concentrations (alanine aminotransferase (ALT) and alkaline phosphatase (ALKP)) can be identified in most cases. Feline leukaemia virus (FeLV) and feline immunodeficiency virus (FIV) status might provide additional information in the process of discussing the optimal treatment regimen and prognosis.
A urinalysis will help rule out diabetes mellitus, since the clinical signs of diabetes mellitus are similar to hyperthyroidism (e.g. polydipsia, polyuria and polyphagia). Urine specific gravity can help differentiate whether an elevated urea and creatinine is due to dehydration (pre-renal azotaemia) or reduced kidney function (renal azotaemia). A urine sample can be obtained either from a free catch using nonabsorbable granules or via cystocentesis if urine culture is required to rule out an infection.
Blood pressure should be monitored to ensure early detection of hypertension, to provide adequate therapy to prevent end organ damage (e.g. retinal detachment, retinal haemorrhage, renal failure) (Figure 1).

Further diagnostic tests to comprehensively assess the patient and rule out concomitant disease are based on the clinical examination and history (e.g. lethargy, respiratory distress, heart disease or gastrointestinal disease). Assessment of advanced heart disease or respiratory illness, thoracic radiographs and/or cardiac ultrasound may be necessary. Tachycardia or arrhythmia might also require an echocardiogram (ECG). In patients with gastrointestinal signs, survey radiographs and abdominal ultrasound might provide additional information (e.g. abdominal lymph node enlargement and intestinal wall thickening often described in gastrointestinal lymphoma or inflammatory bowel disease).
Treatment options
There are three options to stabilise hyperthyroidism: conservative treatment (anti-thyroid drugs), surgical thyroidectomy, and radioactive iodine therapy (131I).
Oral anti-thyroid drugs
Oral antithyroid drugs interfere with the synthesis of thyroid hormone. The currently used drugs are methimazole and carbimazole. Methimazole is available in a transdermal form.
These drugs can be used as a long-term treatment or for the initial stabilisation prior to other treatment modalities such as thyroidectomy and 131I treatment. Administration of the antithyroid drugs will improve systemic complications of hyperthyroidism (e.g. hypertension), therefore keeping anaesthetic risks to a minimum prior to surgery and improving body condition prior to hospitalisation for 131I.
The dosage of these drugs is adjusted according to the level of TT4, urea and creatinine values which are measured every 2 weeks initially. As mentioned above, a renal insufficiency can be unmasked when the cat becomes euthyroid and the treatment needs to be adjusted in order to control the clinical signs without affecting the renal parameters too much.
Methimazole and carbimazole may produce adverse reactions in the first 3 months of treatment (see below) (Peterson, 2008; Baral and Peterson, 2012; Mooney and Peterson, 2012; Peterson, 2012).
The main disadvantage of the oral treatment is the poor compliance of some cats when they need oral medication. The symptoms include vomiting, anorexia, or depression in approximately 10–15% of cats, usually within the first 3 weeks of treatment (Mooney and Peterson, 2012; Peterson, 2012). In the majority of cats the side effects will disappear and medication can be continued. Symptoms may progress and need an alternative method of administering the drug. Transdermal methimazole is associated with fewer gastro-intestinal side effects and may be a suitable option for the cat (Sartor et al, 2004)
There is a growing concern with thyroid nodules that are left for a long period. These tumours may develop into a carcinoma rather than remaining as an adenoma. Therefore a curative treatment for hyperthyroidism is strongly recommended.
Surgical thyroidectomy
Surgical thyroidectomy is a fairly straight forward curative procedure and often considered the preferred treatment in general practice. However, to decrease the cardiac and metabolic complications associated with anaesthetising hyperthyroid cats, prior medical management and control of the clinical signs related to hyperthyroidism are required.
The surgical procedure removes the abnormal thyroid tissue using either the modified intracapsular or the modified extracapsular technique to minimise damage to parathyroid tissue and prevent hyperthyroidism recurring. The excised tissue should always be submitted for histopathological analysis in order to exclude a malignant neoplasia.
The most serious complication that could occur after the surgery is hypocalcaemia secondary to iatrogenic hypoparathyroidism if the parathyroid glands were damaged or removed during surgery, especially in bilateral thyroidectomy. To reduce the incidence of hypocalcaemia, the parathyroid glands can be preserved or transplanted. If hypocalcaemia occurs the treatment is vitamin D and calcium supplementation. If parathyroid tissue is preserved, hypocalcaemia is not usually permanent. Other complications include: Horner's syndrome, laryngeal paralysis, voice changes and clinical hypothyroidism is rare (Mooney, 2010).
The nurse's role after surgery may involve taking blood samples for calcium measurement, monitoring for signs of hypocalcaemia (e.g. pawing at the face, muscle tremors, tetany, and convulsions) and pain.
Hyperthyroidism could recur following thyroidectomy, for this reason it is advisable to measure the TT4 levels at 6 to 12 monthly intervals (Mooney, 2010).
Radioiodine therapy
Radioactive iodine (131I) affects the abnormal thyroid tissue, sparing the normal tissue. The increased levels of thyroid hormones produced by the thyroid nodules create the normal negative feedback effect on the hypothalamus and pituitary, to decrease the production of TSH and TRH. Thus, the lack of TSH stops the normal thyroid tissue from functioning. This unstimulated thyroid tissue will atrophy and become less functional. Therefore, when the radioactive iodine is administered, the less functional atrophied tissue takes up far less of the radioactive iodine than the tumour, and is less affected by the cytotoxic effects of the radiation than the thyroid tumour.
This treatment achieves euthyroidism with one treatment and, euthyroidism is expected in more than 90% of cats with a single dose (Mooney, 2010). A small percentage of cats remain hyperthyroid, but eventually attain euthyroidism weeks to months later without further treatment (Mooney, 1994; Peterson and Becker, 1995). Recurrent hyperthyroidism is rare (Slater et al, 1994).
Hypothyroidism has been suggested to occur in up to 30% of cats after a 3 month period post 131I treatment (Nykamp, 2005). A study of association of iatrogenic hypothyroidism with azotaemia and reduced survival time in cats treated for hyperthyroidism concluded that iatrogenic hypothyroidism appears to contribute to the development of azotaemia after treatment of hyperthyroidism, and reduced survival time in azotaemic cats (Williams et al, 2010). Oral anti-thyroid drugs are normally recommended to be discontinued 1 to 2 weeks prior to 131I treatment as they may interfere with the efficacy of the treatment.
The 131I treatment can be administered subcutaneously (SC) or intravenously (IV). Both routes are effective, although SC is less stressful for the cat, an IV catheter placement is not needed, and only one person is required, reducing the number of personnel exposed to radiation. A sedative may be required depending on the cat's temperament.
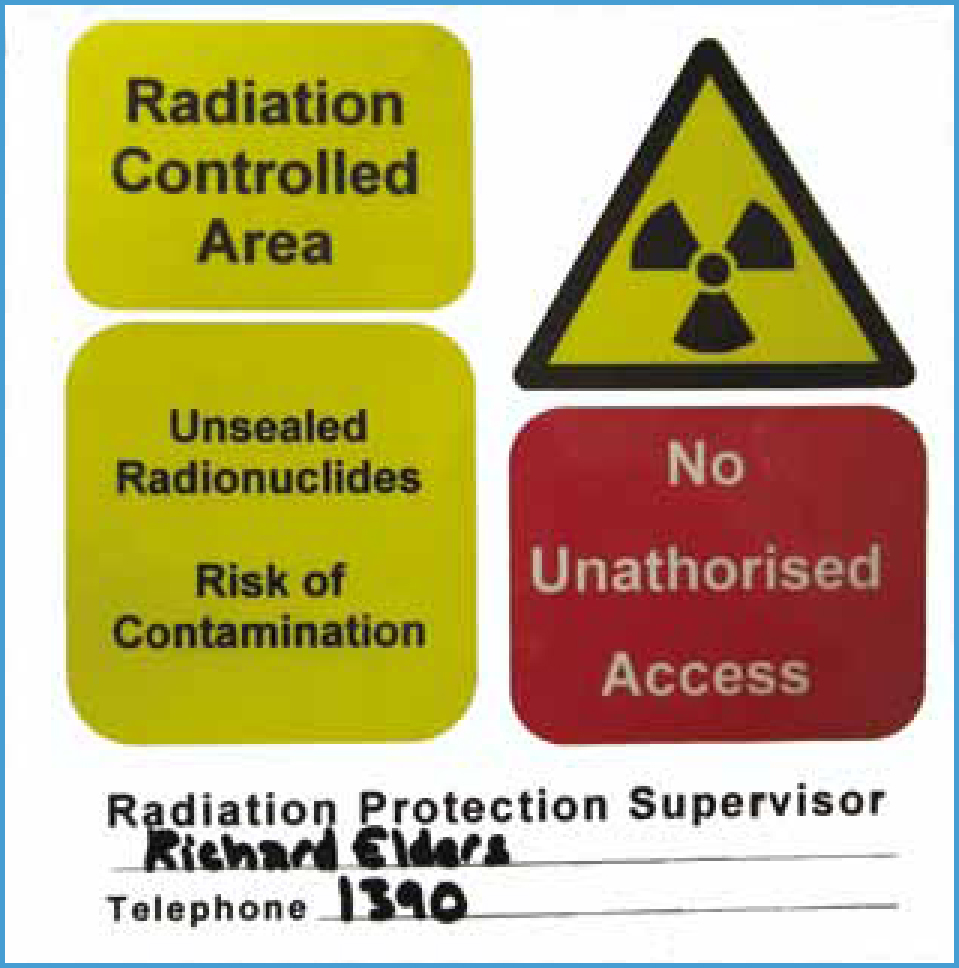
The main disadvantage of this treatment is the 3 week hospitalisation period that is required, this ensures the radiation levels emitted from the cat are at a level that is safe for the cat to go home into the family environment. Urine levels are monitored regularly using a Geiger counter until the reading is safe for the cat to go home (see local rules for radiation). Only trained personnel can access to the controlled area and the time spent with the cat has to be minimised in order to decrease exposure to radiation (Figure 2and3).


Radiation safety
The injection of 131I is prepared by a trained veterinary surgeon wearing a finger thermoluminescent monitor, wearing protective clothing and using a syringe shield.
Once 131I has been administered to the cat, the cat becomes a source of radiation and only authorised personnel (wearing thermoluminescent dose monitors) are allowed to enter the controlled area (Figure 4 and 5). Each person can only access the controlled area for 10 minutes twice a day, and pregnant women should never enter the controlled area. Handling of the cat is kept to a minimum especially avoiding the neck/thyroid area. Disposable aprons, gloves and foot covers should be used to avoid radiation contamination to the clothing when handling the cat. Clinical waste should be disposed of following very strict regulation. Litter trays and food bowls should be cleaned with disinfectant to remove any residue of radiation. Before leaving the controlled area the protective clothing should be disposed of in the designated area, and hands should be thoroughly washed with soap and water (Figure 6).


Detection for possible radiation contamination (e.g. on hands and feet) should be carried out with a Geiger counter, immediately on leaving the controlled area.
The first 2 weeks the cat is at home, owners are advised to empty litter trays into a bag immediately once soiled, fasten with a knot, and place into an outside bin as soon as possible. Hands must be washed thoroughly after handling soiled litter and owners should avoid cuddling/stroking the cat near the thyroid area for these couple of weeks.
Nutrition
Cats are obligate carnivores requiring protein in their diet and during hyperthyroidism they need higher levels of protein than normal to prevent muscle wastage from the catabolism caused by the thyroid hormones. Depending on whether renal disease is present and the stage it is at, the diet will need to be modified (usually less protein and phosphorus).
Glucose and insulin metabolic rates can fluctuate in hyperthyroidism; this can be affected by stress causing a mild hyperglycaemia (Peterson et al, 1981; Baral and Peterson, in press). These physiological changes could cause glucose intolerance and insulin resistance, which over time could progress to diabetes mellitus (Peterson, 2011b). A low carbohydrate diet is recommended to help regulate glucose metabolism and improve response to insulin and prevent obesity when euthyroid (Rucinsky et al, 2010).
Recent studies have indicated that use of a diet with severely restricted iodine levels (Hills prescription Diet y/d Feline – Thyroid Health) can result in normalisation of T4 levels in hyperthyroid cats and provide a further option for medical management of this disease (Melendez et al, 2011; Zoran and Buffington, 2011). With this diet there would be less iodine available to the thyroid gland to create T4 and T3, and thyroid hormone levels eventually fall.
This diet can be useful in the initial stabilisation of the patient before treatment with 131I or surgery, especially if the owner finds it difficult to administer tablets or the cat experiences side effects from methimazole orally or transdermally.
This diet is designed to starve the thyroid from the iodine it needs to create T3 and T4, however, as treats and other foods are high in iodine, other foods should not be given while feeding a low iodine diet. The low iodine diet is useful for treating/stabilising hyperthyroidism initially but, it may not be appropriate as a long-term diet. If the cat has concomitant disease the diet may need to be modified and another method to stabilise hyperthyroidism would need to be considered.
Conclusion
The clinical signs related to hyperthyroidism are caused by elevated TT4 levels which cause a hypermetabolic state affecting all organs. A thorough clinical and physical examination must be carried out when a cat is presented with suspected hyperthyroidism, and if suspicious of an underlying disease then further diagnostic procedures are recommended. Treatment options are conservative treatment, medical therapy or surgical intervention.
Nutrition must not be overlooked in the hyperthyroid cat; due to their hypermetabolic state and the catabolic effect of the thyroid hormones they require more energy. The ideal diet for a hyperthyroid cat is high protein, which is easily digestible and low in carbohydrates. This diet may need to be modified if a concomitant disease is present.

