The patient was referred to a veterinary hospital as an emergency, with an acute onset of progressive tetraparesis.
Signalment
Species: Canine
Breed: Border Collie
Age: 10 years 2 months
Sex: Male neutered
Weight: 19.3 kg
Assessment
On presentation the patient was bright, alert and responsive but unable to stand or support their own bodyweight. Clinical examination was unremarkable aside from moderate dental disease and the non-ambulatory tetraparesis; the patient's vital parameters were all within normal limits.
A clinical history was taken, revealing a 5-day history of progressive tetraparesis which was not thought to be painful. A softer bark than normal was also reported by the owners. Normal bladder function was maintained and the patient was able to wag their tail. Taking a detailed history is an important step in diagnosis of neurological conditions, as the time and nature of onset, together with a thorough neurological examination, will help to localise the disease and aid in selection of further tests and interventions (Platt and Olby, 2004).
A neurological examination by the veterinarian confirmed a non-ambulatory tetraparesis (Table 1), with voluntary movement in all four limbs but significant weakness and proprioceptive deficits (Figure 1); this is assessed by knuckling the patient's paw to see if they correct the placement (Platt and Olby, 2004). If a patient is weak then they may not be able to correct the paw position even if they do have the correct sensory pathways (awareness of where the limb is placed). The patella reflexes were intact, but reduced withdrawal reflexes were observed in all four limbs.
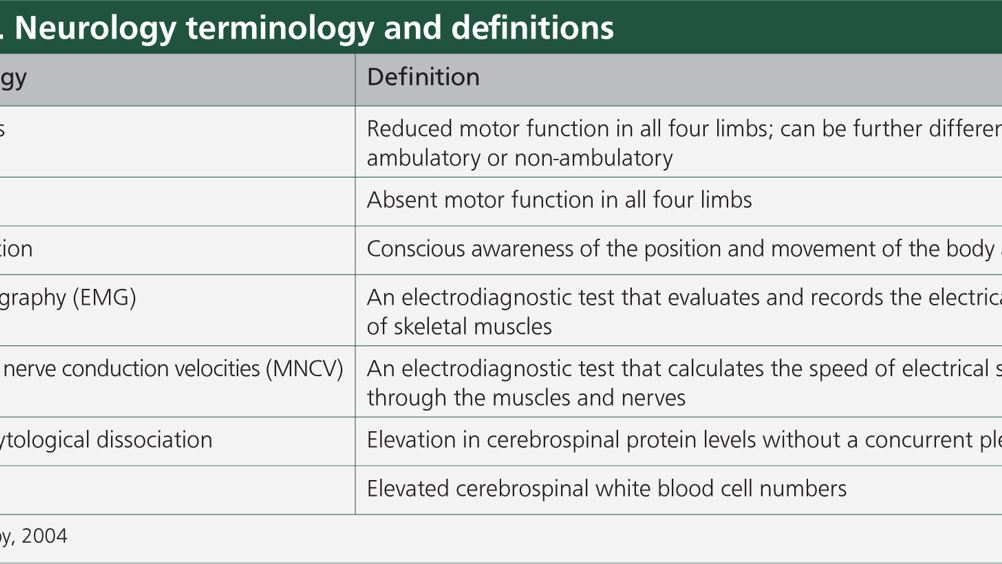
Table 1. Neurology terminology and definitions
| Terminology | Definition |
|---|---|
| Tetraparesis | Reduced motor function in all four limbs; can be further differentiated as ambulatory or non-ambulatory |
| Tetraplegia | Absent motor function in all four limbs |
| Proprioception | Conscious awareness of the position and movement of the body and limbs |
| Electromyography (EMG) | An electrodiagnostic test that evaluates and records the electrical activity of skeletal muscles |
| Muscle and nerve conduction velocities (MNCV) | An electrodiagnostic test that calculates the speed of electrical signals through the muscles and nerves |
| Albuminocytological dissociation | Elevation in cerebrospinal protein levels without a concurrent pleocytosis |
| Pleocytosis | Elevated cerebrospinal white blood cell numbers |

Testing of reflexes is done to assess peripheral nerve pathways independently from the central nervous system (CNS) (de Lahunta, et al., 2014). Reflex pathways have a sensory and a motor component, with no input from the CNS in order to activate the motor neurons; this is predominantly a protective mechanism to avoid tissue trauma that may occur in the time it takes for the sensation to reach to brain. Instead the sensory neuron is activated and the action potential is conducted to the dorsal grey matter of the spinal cord, where it synapses directly with the motor neurons in the ventral horn that then act to prevent damage to the body. In this patient the withdrawal reflexes were reduced in all limbs, localising the problem to the peripheral nervous system (PNS). Electrodiagnostics were therefore recommended as opposed to magnetic resonance imaging, as these would identify where in the PNS the problem was located (Cuddon, 1998; Dewey and da Costa, 2016).
Investigations
The patient was admitted to the hospital and an intravenous (IV) catheter was placed aseptically in the left cephalic vein. A jugular blood sample was taken and the following tests performed: biochemistry, haematology, electrolytes, Toxoplasma spp. and Neospora spp. serology and basal cortisol. All of these tests came back within normal limits; this excluded any infectious or metabolic cause for the patient's generalised weakness. The patient was placed on intravenous fluid therapy with Hartmann's solution (Aqupharm 11, Animalcare) at a maintenance rate (2 ml/kg/hour). A conscious right lateral chest radiograph detected no abnormalities, ruling out a megaoesophagus.
Differential diagnoses for the patient included myasthenia gravis, an immune-mediated disease of the neuromuscular junction, which can also cause megaoesophagus. It is essential to rule out any megaoesophagus as part of the initial investigation as this would put the patient at a higher risk for aspiration pneumonia, and assisted feeding would be required to minimise this risk (Platt and Olby, 2004).
Electromyography (EMG) and muscle and nerve conduction velocities (MNCV) were completed under general anaesthetic. The aim of electrodiagnostics is to localise the disease further and identify where in the neuromuscular system the problem is (Dewey and da Costa, 2016). There are three possibilities: a problem with the nerves (neuropathy); a problem with the muscles (myopathy); or a problem at the neuromuscular junction itself.
Spontaneous muscle activity was observed in all muscles tested during the patient's EMG. In a healthy patient, no muscle activity should be noted because of the general anaesthetic; spontaneous muscle activity indicates denervation of the muscles, suggesting a neuropathy or a myopathy (Cuddon, 1998). The MNCVs then demonstrated reduced compound muscle action potential amplitudes and reduced motor nerve conduction velocities, further narrowing the diagnosis to a likely neuropathy, predominantly affecting the motor neurons. A lumbar cerebrospinal fluid (CSF) sample was taken, demonstrating an elevation in cerebrospinal protein levels without a concurrent pleocytosis. This presentation of CSF is defined as albuminocytological dissociation (Platt and Olby, 2004).
Based on the clinical history, electrodiagnostics and CSF results a diagnosis of acute idiopathic polyradiculoneuritis (APN) was made. Also known as Coonhound paralysis because of its historical association with racoon bites, the pathophysiology of APN is not well understood, but it is thought to be a result of immune-mediated inflammation of the ventral nerve roots of the spinal cord, where the motor neurons originate (Kingma and Catcott, 1954; Cuddon, 2002). Severe cases may require artificial ventilation as the skeletal muscles of the respiratory system may fail. Cranial nerves are also affected in 80% of dogs, with dysphonia a common presenting sign (Rupp et al, 2013). Numerous risk factors for APN have been suggested, including raw chicken consumption, breed and season (Laws et al, 2017; Martinez-Anton et al, 2018). Decreased vitamin D levels have also recently been found in dogs with APN, though the clinical significance of this is not yet known (Laws et al, 2018). As a self-limiting condition, most patients improve without treatment within 3–5 weeks.
Nursing care
There is no treatment for APN, but intensive nursing care is required within the 3–5 week recovery period to manage the flaccid tetraparesis/tetraplegia and minimise associated complications (Fenn, 2019). Basic monitoring of the patient was undertaken, to include heart rate, respiratory rate and temperature checks twice daily, but further specialised care was also vital.
Recumbency care
The patient was turned at 4 hourly intervals from left to right lateral, and vice versa. Attempts were made to support the patient in sternal recumbency, but the flaccid tetraparesis made this difficult and most often they would sink back into a lateral recumbency again. In patients unable to move themselves it is vital to manage their recumbency to prevent complications such as urine scalding, decubitus ulcers and atelectasis (de Lahunta et al, 2014). Patient positioning is of particular importance in patients with neuromuscular disease, as muscle mass is lost quickly and puts them at a higher risk of pressure sores (Fenn, 2019).
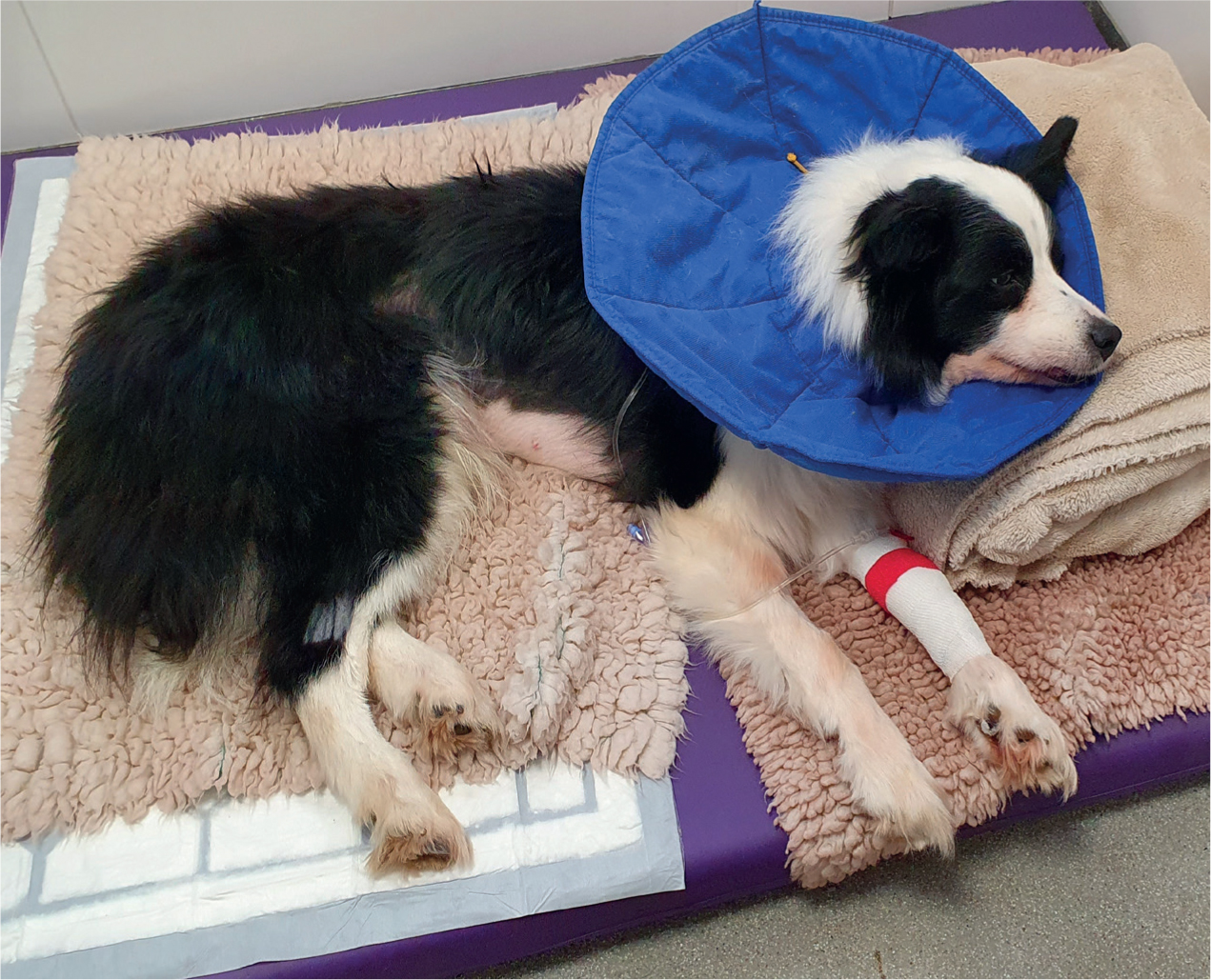
Soft, padded bedding should be used, ideally of a type that wicks moisture aware from the skin to prevent urine scalding should the patient soil themselves (Figure 2). Bladder function is retained in patients with APN, and in this case the patient was able to urinate independently, but bladder management should be considered in all recumbent patients. As the patient was turned every 4 hours, their bed was also checked for soiling, and if any found the bed was cleaned and replaced and the patient bathed to ensure no urine remained on the skin. The acidic pH of urine irritates the skin and can lead to urine scalding if not managed effectively.
If hydration status is a concern, or a patient is expected to have reduced bladder function for a prolonged period of time, a urinary catheter can be considered to help keep the patient clean and record urine output accurately. This was not required in this case.
Physiotherapy
Physical rehabilitation aims to reduce tissue adhesions, maintain muscle and joint flexibility and prevent stiffness and pain (Hesbach, 2014). It is an important therapy in neuromuscular cases because of the rapid loss of muscle mass, as it is important to preserve and maintain muscle and joint function as much as possible (Fenn, 2019). Physiotherapy is an important part of holistic nursing care, and in this case was carried out by the registered veterinary nurse (RVN).
Massage and passive range of motion (PROM) exercises were employed in the patient three times daily, in all four limbs. Massage involves the manipulation of soft tissues in the limb, and helps to increase circulation and decrease adhesions formed by inflammation and immobility, alongside helping with anxiety and distress in some patients (Millis and Levine, 2014). PROM exercises improve joint and muscle motion and help to lessen the effects of immobility seen in neuromuscular disease (Millis and Levine, 2014). Each of the patient's joints in each limb were moved gently to full extension, and then full flexion, and held in each position for 10 seconds. All physiotherapy was well tolerated by the patient and helped the nursing staff to bond with him. Building a rapport with the patient helps to increase nursing and patient satisfaction (Ackerman and Aspinall, 2016) and makes the patient's hospitalisation a more pleasant and stress-free experience.
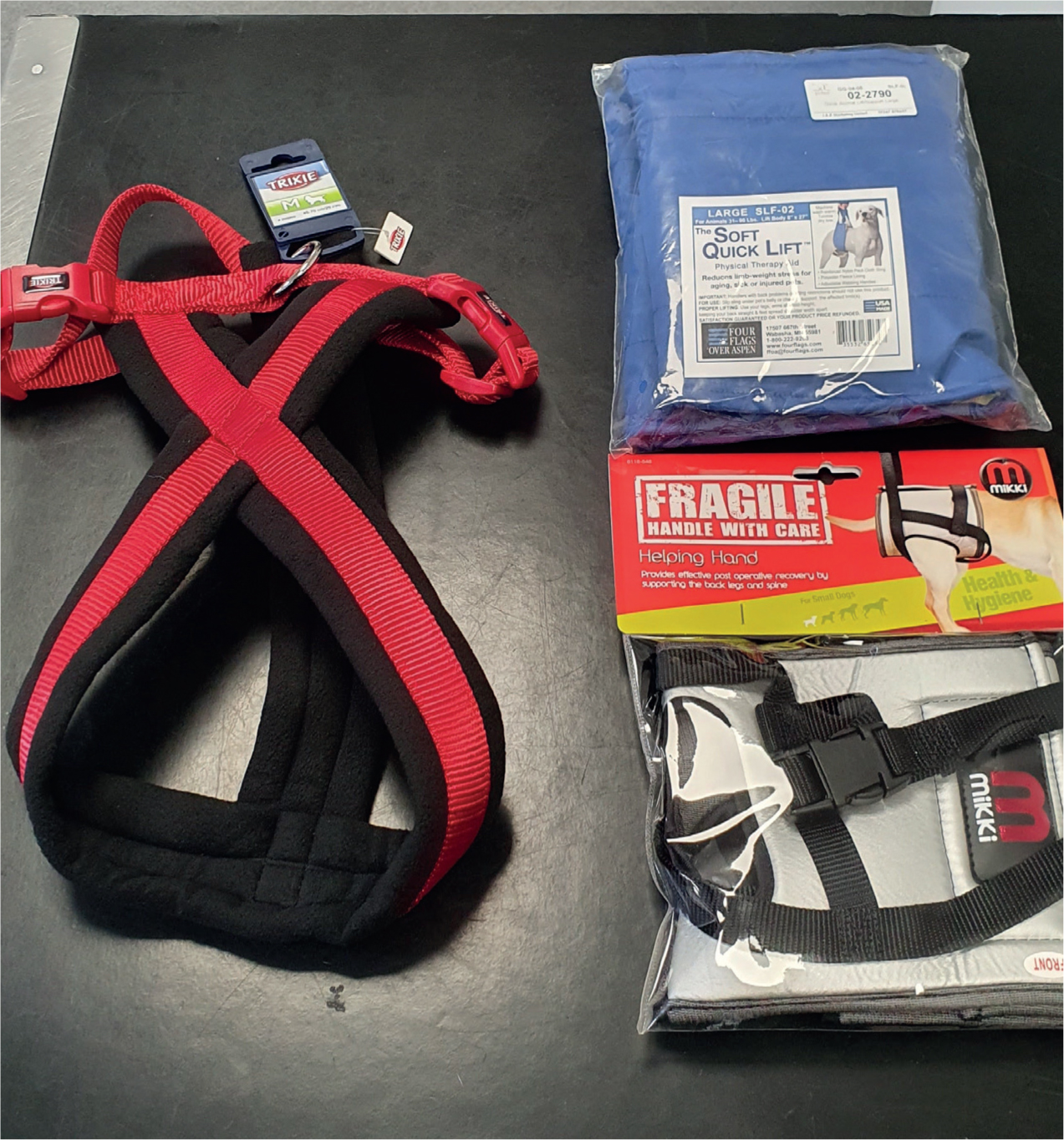
Alongside passive physiotherapy, the patient was regularly assisted with standing upright and opportunities to urinate and defecate outside. A harness and helping hands lifting pants (Mikki Pet) were used by the RVN to support the patient appropriately (Figure 3).
Pneumonia
Nosocomial respiratory conditions are an important consideration in any recumbent hospitalised patient. Appropriate nursing care aims to reduce the incidence of both hypostatic and aspiration pneumonia.
Hypostatic pneumonia is a result of immobility and the animal's own weight impairing blood flow to the lung parenchyma, reducing tissue perfusion and putting the patient at risk of fluid movement into the pulmonary space from the circulation (Elphee, 2011). This fluid accumulation can be a source for secondary infection, alongside reducing the animal's capacity for gaseous exchange.
Aspiration pneumonia occurs as a result of inhalation of foreign material such as saliva or regurgitated stomach contents, which then becomes a focus for bacterial infection in the lungs (Egleston, 2018). Most aspiration events are not observed in veterinary patients, with pneumonia only subsequently diagnosed when respiratory compromise develops 2 to 6 hours later (Egleston, 2018). Neurological patients are at a higher risk of aspiration pneumonia than other patients, as are recumbent patients, putting APN cases at increased risk of developing a nosocomial pneumonia during hospitalisation (Kogan et al, 2009).
Respiratory rate should be monitored during hospitalisation to identify early when any respiratory compromise may be occurring; in this patient it was recorded at 4 hourly intervals. On day eight of hospitalisation an increased respiratory effort was noted by the RVN, alongside a pyrexia of 39.7°C. Respiratory rate was normal at 20 breaths per minute. A conscious chest radiograph showed no evidence of pneumonia, but a pulse oximetry reading confirmed an oxygen saturation of 91% on room air. Oxygen supplementation was provided via nasal prongs (Figure 4) and broad-spectrum antibiotic therapy was started with IV cefuroxime (Zinacef, GSK) and marbofloxacin (Marbocyl, Vetoquinol UK Limited) administered by the RVN, under direction of the veterinary surgeon. IV paracetamol (Paracetamol, Braun) was also administered to assist in bringing the patient's temperature down.

Oxygen supplementation was tailored to the patient's respiratory rate, effort and oxygen saturation in the following days. By day 11 of hospitalisation the patient was no longer oxygen dependent.
Nutrition
It is important not to forget a patient's nutritional demands during a prolonged hospitalisation period (Fenn, 2019). The strange environment of a veterinary hospital, together with lack of physical and mental stimulation, can lead patients to become depressed and refuse food. In this case the patient required frequent tempting to eat in order to meet their resting energy requirements (RER). The RVN used a variety of techniques to tempt the patient to eat, including offering a variety of diets, hand feeding and warming the food. RER was calculated from the patient's bodyweight for each diet to ensure that it was being met sufficiently. He was weighed daily and this was recorded on the hospital sheets as a way to monitor for any weight loss. Water was also offered frequently, as the patient was unable to move themselves to the water bowl.
Immunoglobulin therapy
Intravenous human immunoglobulin (IVIg) therapy has previously been used in dogs suffering from immune-mediated haemolytic anaemia (IMHA), with only one study demonstrating a trend towards a faster recovery in APN cases (Hirschvogel et al, 2012). APN is commonly compared with Guillain-Barré syndrome in human medicine, for which the treatment is an IVIg infusion on five consecutive days (Cummings and Haas, 1967; Cuddon, 2002). Humans suffering from Guillain-Barré syndrome treated with IVIg demonstrate a faster recovery, with a shortened time until they are able to ambulate independently and reduced incidence of artificial ventilation being required (Nobile-Orazio and Terenghi, 2005).
IVIg therapy was initiated on day ten of hospitalisation because of the patient's lack of improvement (they had in fact deteriorated to become tetraplegic) and subsequent aspiration pneumonia. The hope was that by encouraging a faster recovery from APN the patient would be able to ambulate independently, which in turn would aid in recovery from the aspiration pneumonia.
A 0.5 g/kg dose of IVIg (Intratect, Biotest) was administered IV over a 6-hour period, as described by Hirschvogel et al (2012). A protocol for the use of IVIg in IMHA was consulted in the absence of a thorough protocol for the use in APN cases (Whelan et al, 2009). A new IV catheter was placed and a giving set with a microfilter and an infusion pump was used to infuse the treatment, ensuring accurate dosing.
Close monitoring of the patient was carried out throughout the infusion because of the risk of an anaphylactic reaction; this was the responsibility of the RVN. Observations included systolic blood pressure measurement, heart rate, respiratory rate and effort, rectal temperature, mucous membrane colour, capillary refill time, mentation and demeanour (Whelan et al, 2009). These were recorded every 5 minutes for the first hour of the transfusion and then every 30 minutes for the remaining 5 hours (Hirschvogel et al, 2012). The infusion finished without any suspected adverse effects.
Literature for APN and Guillain-Barré syndrome describe usual IVIg therapy as administration of an infusion on 3–5 consecutive days (Cummings and Haas, 1967; Cuddon, 2002; Whelan et al, 2009; Hirschvogel et al, 2012). Financial constraints in this case meant that only a single infusion was given.
Outcome
The patient was discharged on day 14 of hospitalisation. The patient had become tetraplegic prior to the infusion but over the 4 days before discharge they regained some voluntary movement in all four limbs. At the time of discharge they were non-ambulatory tetraparetic, with some voluntary movement in all four limbs. The respiration rate and respiratory effort were normal off oxygen. The patient was discharged on oral marbofloxacin (Marbocyl, Vetoquinol UK Limited) and cephalexin (Rilexine, Virbac) as ongoing treatment for his aspiration pneumonia. The owners flagged a previous diagnosis of hip osteoarthritis on discharge that was thought to be causing the patient an element of discomfort, and so oral robenacoxib (Onsior, Elanco) was also dispensed. The owners were given in-structions for recumbency care and physiotherapy to carry out at home.
A week later the patient was presented for re-examination and the decision was made to euthanase because of poor non-ambulatory status and failure to improve as hoped. All non-ambulatory patients are difficult to manage at home, and despite the owner's best efforts the patient was considered to be suffering, with poor quality of life.
Conclusion
Though a sad outcome, this was an interesting and rewarding case to nurse. Patients presenting with APN, as with all recumbent cases, require intensive nursing care to support and enrich their hospitalisation and recovery. The use of IVIg therapy in APN is still considered novel, and though its use in this case did not change the outcome, it remains an intriguing area of research in the treatment of APN.
KEY POINTS
- Acute idiopathic polyradiculoneuritis (APN) is a poorly understood disease, thought to be immune-mediated, that causes inflammation of the ventral nerve roots of the spinal cord and subsequent flaccid tetraparesis and/or tetraplegia.
- APN is a self-limiting condition and usually resolves without treatment, but patients require intensive nursing care because of ongoing recumbency.
- Nursing care for these patients includes recumbency and bladder management, nutritional support and supportive care for any complications that may develop.
- Intravenous human immunoglobuin therapy is a novel new treatment for APN that has been shown to improve recovery times.
- Common complications in APN patients include hypostatic and/or aspiration pneumonia, muscle atropy and pressure sores.
- Nursing APN patients is an intensive and time-consuming job, but ultimately rewarding if they do well.