References
Corneal ulcers part 1: aetiology and management of superficial corneal ulcers
Abstract
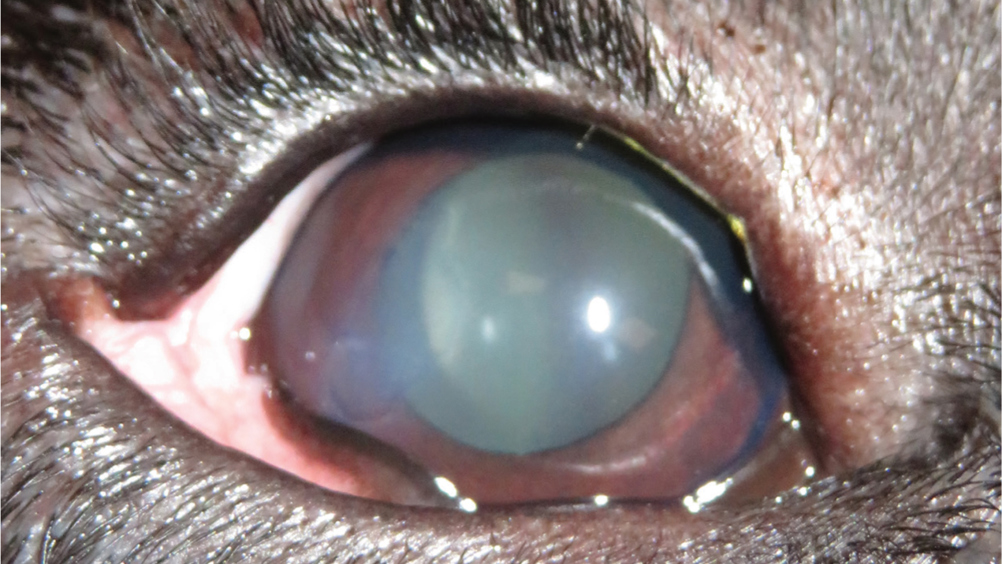
Corneal ulceration is one of the most common ocular problems presented in first opinion practice. Ocular diseases in dogs can be distressing for both the patient and the owner, registered veterinary nurses can provide advice to distressed owners and ensure that patients are provided with evidence-based and holistic care. Part one of this two-part series discusses the aetiology and management of superficial corneal ulcers. The second part of this article will discuss deep corneal ulcers and will explore the role of registered veterinary nurses within ocular diseases.
Corneal ulceration is one of the most common ocular disorders presented in first opinion practice (Startup, 1984; O'Neill et al, 2017). Corneal ulceration is described as a break in continuity of the corneal epithelium with exposure of the underlying stroma; they can be classified according to depth and extent (Maggs, 2013). Anecdotally, registered veterinary nurses (RVN) are often underutilised in veterinary practice and the author has noticed a particular underutilisation in ophthalmic nursing in first opinion practice (Gerrard, 2017; Harvey and Cameron, 2019). RVNs can be well utilised in corneal ulceration cases — their role extends from the recognition and understanding of corneal ulcers, ensuring appropriate handling and restraint, performing routine ophthalmic tests, recognising ophthalmic pain and supporting and educating owners.
The first part of this two-part series looks at the aetiology of superficial corneal ulcers and spontaneous chronic corneal epithelial defects (SCCED), the associated complications and the medical and surgical treatment options. The second part will discuss the aetiology, diagnosis and treatment of deep corneal ulcers and descemetoceles, and will explore the role of veterinary nurses in ophthalmology including: routine ophthalmic tests, patient handling and client education.
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

