In 2008 the World Health Organization (WHO) introduced a surgical safety checklist as a part of the Safe Surgery Saves Lives campaign (Weiser and Haynes, 2018). Now, over a decade later, recordings from eight major hospitals around the world (Canada, India, Jordan, New Zealand, The Philippines, Tanzania, UK and USA) show a decrease in mortality and complications of 37–48% after implementing the checklist (Tang et al, 2014).
There is a rising trend within the veterinary profession to perform increasingly complicated and invasive surgery on family pets through the use of more intricate techniques trickling down from human medicine (McMillan, 2014). With these surgeries comes the increasing risk of postoperative complications (McMillan, 2014).
In human medicine, it is estimated that 7 million people will experience surgical complications each year and out of that group, 1 million people succumb to fatal complications (World Health Organization (WHO), 2014). It is thought that half of these deaths could be prevented (WHO, 2014). In 1991, Harvard medical practice first raised an issue with patient safety, showing that 3.7% of patients suffered medical harm or complications while hospitalised (Tivers, 2015). Furthermore, human error is responsible for up to 70% of anaesthesia-related deaths in humans (Hofmeister, et al, 2014). As a result of this, the World Health Organization decided to take inspiration from the use of safety checklists in aviation and other high-reliability industries (Clay-Williams and Colligan, 2015). The flight checklist is used to enforce communication between crew members, and therefore enable mutual supervision and provide a standard operating procedure to minimise complications (Degani and Weiner, 1993). Medical checklists are used as a cognitive aid to free up mental capacity of the practitioners and allow for visual reminders (Ballantyne, 2018). They are also believed to spread responsibility and reduce the emotional distress for clinicians following potential medical mistakes (Oxtoby and Mossop, 2016). In 2008, the checklist was presented by the WHO as a part of the Safe Surgery Saves Lives campaign. It is now used in all National Health Service (NHS) hospitals throughout the UK (Bradbrook, 2018).
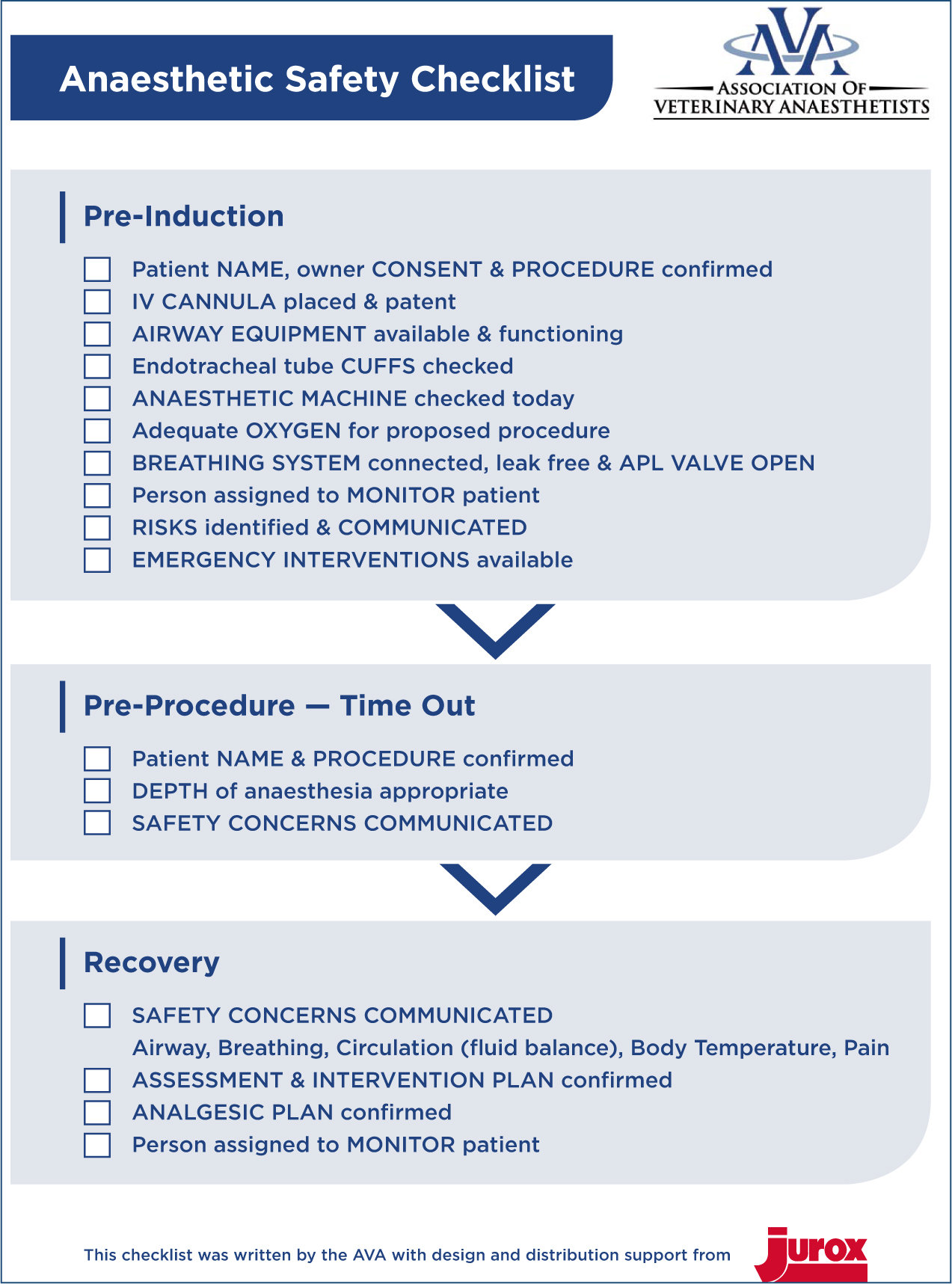
Inspired by the aviation checklist, the medical surgical checklist consists of three parts: pre-induction, pre-procedure and recovery. There is no standard checklist that is implemented throughout the veterinary world; instead, each practice is free to develop their own. The Association of Veterinary Anaesthetists (AVA) published a checklist in 2014, which is available free of charge, online (https://ava.eu.com/resources/checklists/).
This study investigated the potential reduction in postoperative complications as a result of applying a surgical safety checklist, created by The AVA, to veterinary procedures. The hypothesis was that there would be a reduction in complications following the introduction of surgical safety checklists.
Methods
The study ran over 8 weeks between January 13 and March 6, 2020. All owners with cats and dogs scheduled to undergo an elective surgical procedure during this time were invited to participate and informed consent was obtained from those owners choosing to take part in the study. The registered veterinary nurse or veterinary surgeon admitting the patient for the procedure was fully informed on what the study is about, and the researcher was available to answer any questions the owner might have. Following admission, the patient received a full physical examination from a veterinary surgeon. Both minor and major procedures were included, with the exception of non-surgical dental procedures; examples of minor procedures undertaken include cat castrations, and major procedures include orthopaedic surgery. The surgical procedure was then carried out by a veterinary surgeon according to normal practice standards. All patients were induced using propofol or alfaxalone intubated and anaesthesia was maintained using sevoflurane gas delivered in 100% oxygen using a Humphrey ADE anaesthetic circuit. All patients were scheduled for two postoperative checks at the veterinary clinic 3 and 10 days after the procedure, carried out by either a registered veterinary nurse or a veterinary surgeon. After these checks, the researcher noted and recorded the absence or presence of any postoperative complications. Postoperative complications were rated from 1 to 4, 1 meaning no complications noted, 2 meaning some complications noted that required treatment such as medication, 3 meaning extensive complications noted, patient in need of surgical intervention and 4 meaning worst possible scenario and death of patient (Table 1). During the first 4 weeks, every patient with consent for taking part in the study was included in the ‘control group’, in which checklists were not used. The following 4 weeks, every patient with consent for taking part in the study was included in the ‘treatment group’, in which the AVA checklist was applied (Figure 1). The researcher then anonymously compiled the results and evaluated if there was any statistically significant difference in postoperative complications between the treatment and control group. Statistical analysis of the data collected was performed using non-parametric testing using chi-squared. With-holding checklists from one cohort could be regarded as an ethical concern as there has been evidence in previous studies that showed a reduction in complications.
Table 1. Ranking of postoperative complications
| 1 | No complications |
| 2 | Some complications, requiring medication (e.g. gastric upset, infection) |
| 3 | Major complications, requiring surgical intervention (e.g. complete wound breakdown) |
| 4 | Death of patient |
Results
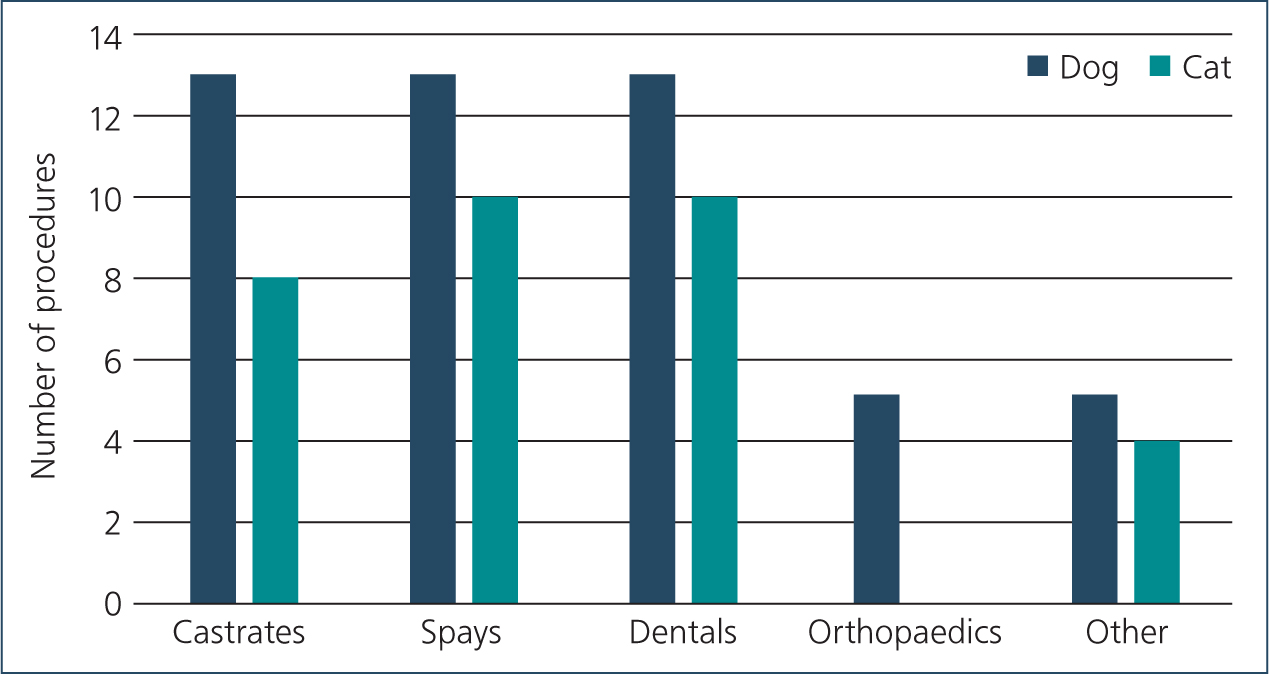
A total of 192 patients were entered into the study. 82 patients were assigned to the control group and therefore not subjected to the surgical safety checklist. Of these 82 patients, 23 (28%) were admitted for dental procedures, 13 (16%) for dog castrations, 13 (16%) for bitch spays, 10 (12%) for cat spays, 8 (10%) for cat castrations, 5 (6%) for orthopaedic surgery and 10 (12%) for other procedures such as lump removals (see Figure 2).
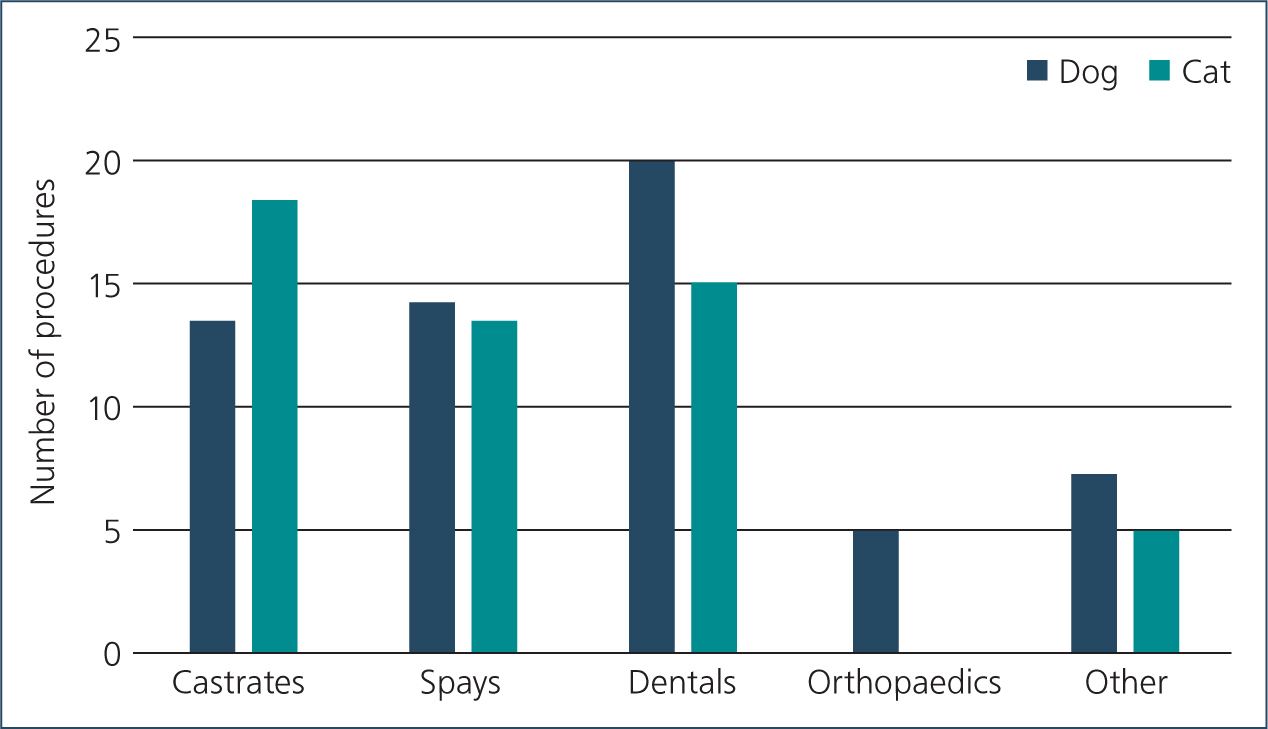
110 patients were assigned to the treatment group and the AVA surgical safety checklist was used for their procedure. Out of these patients 35 (32%) underwent surgical dental procedures, 18 (16%) were cat castrations, 14 (13%) bitch spays, 13 (12%) dog castrations, 13 (12%) cat spays, 5 (4%) orthopaedic procedures and 12 (11%) were other surgical procedures (see Figure 3).
Although 192 patients were entered into the study, 17 were excluded because the client did not bring their pet back for a postoperative check, and therefore the researcher was unable to accurately judge the postoperative score for these patients. This explains the discrepancy between surgeries performed and postoperative scores noted.
The majority of procedures conducted during the first 4 weeks (control group) were surgical dental procedures. This number is so large because the category includes both cats and dogs.
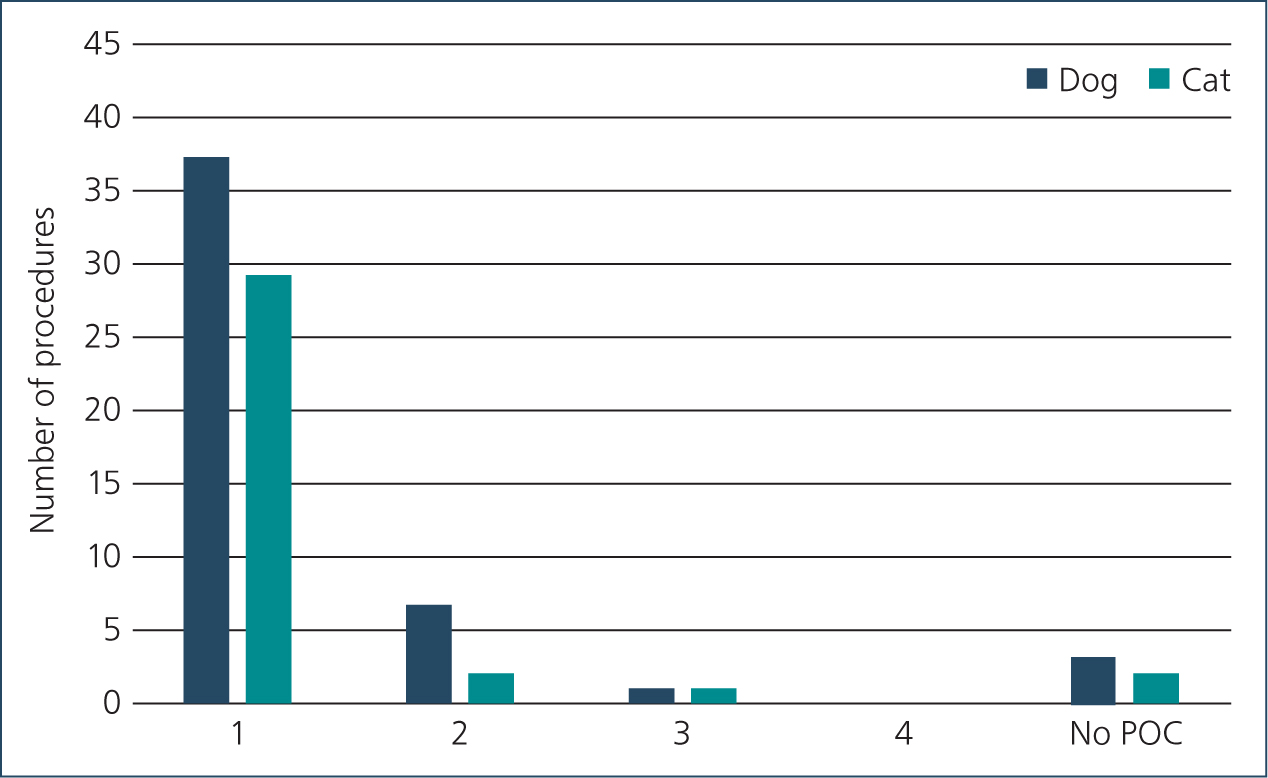
Out of the 82 control group patients 86% (n=66) presented with a postoperative score of 1, 12% (n=9) had a postoperative score of 2, 2% (n=2) patients had a postoperative score of 3 and 0% patients had a score of 4 (0). An explanation of these scores can be found in Figure 4. 7.3% (n=5) of patients did not attend a postoperative check (Figure 4).
The most common postoperative complications in the control group were score 2, gastric upsets and minor infections. Two patients required additional surgery (score 3). One patient presented with an abdominal hernia following a midline cat spay operation. A hernia repair was performed and the patient recovered fully. The other patient underwent a lump removal and then presented with a complete wound breakdown. Bacteria (Escherichia coli and Enterococcus species) was cultured from the site and the wound was instead treated as an open wound and was provided with appropriate care and healed within 3 weeks of the first surgery.
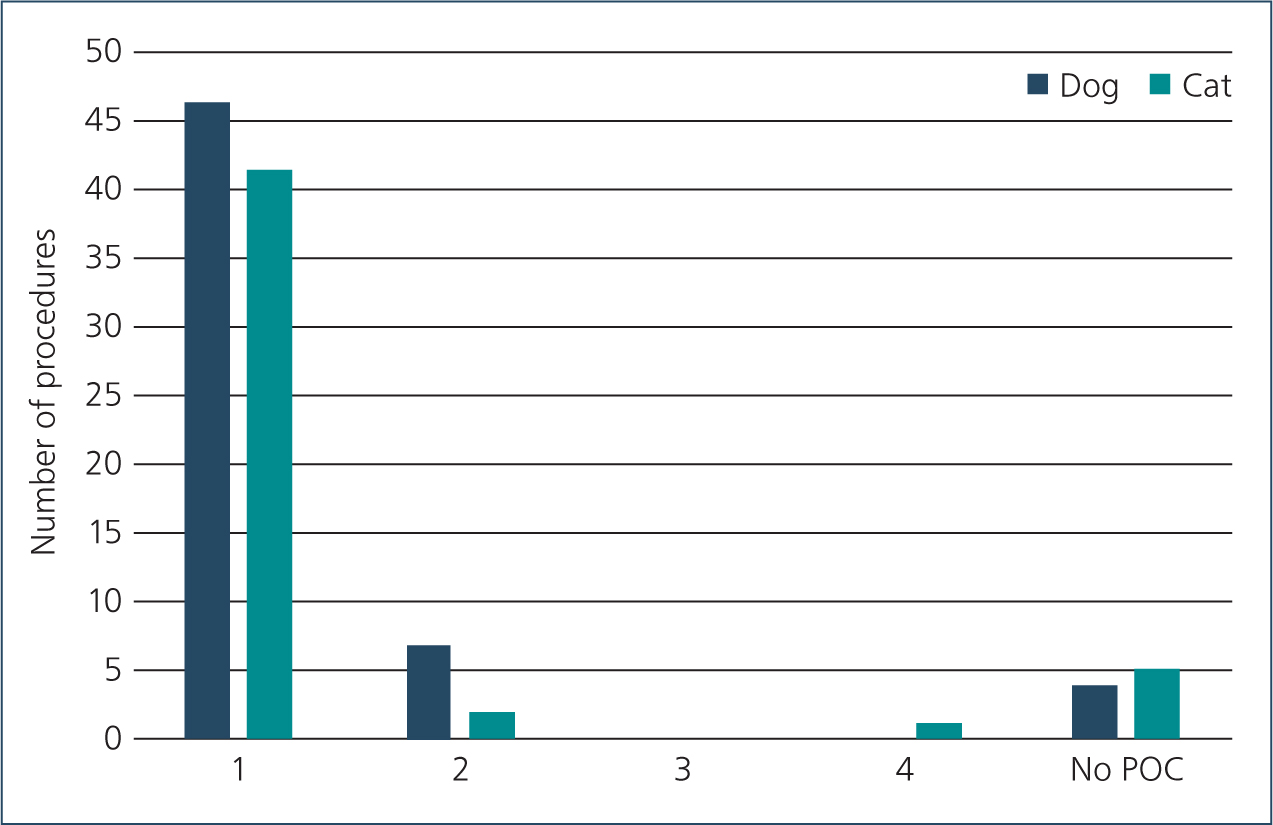
The distribution of procedures for the treatment group is similar to the first 4 weeks of the study (the control group), resulting in a good comparison. Out of these patients 90% (n=89) presented with a postoperative score of 1. 9% (n=9) patients had a score or 2, 0% (n=0) patients had a score of 3 and 1% (n=1) patient had a score of 4. 11 Patients did not attend the postoperative check meaning no data were collected from these patients (Figure 5).
Similarly to the first group of subjects, most postoperative complications were gastric upsets and minor infections, infections being especially common after dental procedures. It should be noted that the patient that died was a high risk patient with an American Society of Anesthesiologists (ASA) score of 5, meaning a moribund patient that is not expected to survive without the operation (ASA Physical Status Classification System, 2019).
According to the data collected, there was a 4% decrease of postoperative complications after the introduction of the surgical safety checklists.
Data analysis
To evaluate whether the results found in this study are statistically significant, a contingency chi-square (X2) test was chosen.
The chi-square statistic with one degree of freedom was 0.2245. The p-value was 0.635626. The result is not significant at p<0.05. The chi-square results indicate that the results from this study are not significant, there is no true difference between the complication/no complication outcome in the presence or absence of the checklist. The chi-square table would require a value of chi that is 3.84 or higher to be significant (Table 2).
Table 2. Chi squared calculation
| No checklist | Checklist | Total | |
|---|---|---|---|
| No complications | 66 (67.05) [0.02] | 89 (87.95) [0.01] | 155 |
| Complications | 11 (9.95) [0.11] | 12 (13.05) [0.08] | 23 |
| Column total | 77 | 101 | 178 |
Discussion
The aim of this study was to evaluate the effectiveness of applying the AVA surgical safety checklist to veterinary procedures to reduce postoperative complications. The study was designed to compare a group of patients that underwent surgery without the use of a surgical safety checklist with a group of patients that underwent surgery with the use of a checklist. The hypothesis was that a difference in postoperative complications would be noted through the use of the AVA checklist. This hypothesis cannot be confirmed as even though a 4% decrease in postoperative complications was noted following the implementation of the checklist, this decrease was not statistically significant. This is in disagreement with previous studies within the veterinary field, which all showed statistically significant reductions in postoperative complications (Bergström et al, 2016; Cray et al, 2018; Launcelott et al, 2019).
Minor complications such as rashes, redness or swelling were not considered to be of significance in this study, and therefore patients with these complications were given a postoperative score of 1. In several records, rashes were noted as being caused by the electrical clippers used when preparing the operating site and therefore not a part of the points on the checklist. Swelling or redness around the operating site is normal and part of the inflammation and healing process, therefore this was not marked as a true complication (Guo and DiPietro, 2010). Judging whether or not the swelling was normal was at the discretion of the surgeon or nurse performing the check.
The most common postoperative complications observed included minor infections treated with antibiotics; the most commonly used antibiotic was amoxicillin. Antibiotics were not used for routine procedures, however, they were provided intravenously (cefuroxime) for any orthopaedic surgeries. No patients in this study were discharged with a course of antibiotics.
Another complication was post-anaesthetic diarrhoea. A study conducted in 2017 monitoring 237 dogs undergoing general anaesthesia for diagnostic or surgical purposes showed that 33.4% of patients suffered with post-anaesthetic diarrhoea (Torrente et al, 2017), meaning that it is a common and expected side effect of a general anaesthetic in animals. The length of anaesthesia, changes in body positioning as well as surgical site were shown to be possible causes (Torrente et al, 2017). The patients that presented with diarrhoea at the postoperative check were commonly prescribed a course of specialised food as well as pro-biotics. The treatment provided was at the discretion of the veterinary surgeon. Further studies into the effectiveness of surgical safety checklists in correlation with drug choices may be warranted as some drugs reduce swelling or pain (e.g. non-steroidal anti-inflammatory drugs and opioids).
For animal procedures, a smaller difference can be seen after the application of a surgical safety checklist than in human medicine, with a 10% decrease seen in animal medicine (Bergström et al, 2016) versus 48% decrease in human medicine (Tang et al, 2014). This discrepancy may be caused by the larger number of procedures performed in humans, which often are more high risk and complicated than those performed in animals (Cray et al, 2018). Owners may also elect to euthanase their pet instead of subjecting them to complex surgery, a choice not available within human medicine, meaning that the high risk, complicated surgeries, which may have caused severe postoperative complications, are never performed in the first place.
Checklists were provided for all procedures in the treatment group, attached to the anaesthetic record sheet. Staff members may have seen the checklist as unnecessary or as a critique on their operating procedures, as this problem has been noted in other studies (Hofmeister et al, 2014; Pugel et al, 2015), however, this was not determined in this study. In their article from 2018, Ballantyne argued this point, saying that relationships between veterinary surgeons and veterinary nurses are often closer than those of doctors and nurses as the veterinary world is much smaller than the one of human medicine, meaning that the staff members may have worked closely together for a long time. She states that this may mean that surgical safety checklists may be less warranted during surgical procedures because communication is more established in those instances (Ballantyne, 2018). Arguably, however, this may be exactly when checklists are most warranted. If staff become too complacent, errors may occur. The Royal College of Veterinary Surgeons (RCVS) supports this view and has reported that communication breakdowns are the second most common error within veterinary hospitals (RCVS, 2020).
This study only provides a single data point, a before and after comparison for one veterinary practice. Enough data to be able to run a chi squared test to test significance were gathered to see if the checklists had an effect at the veterinary practice, but the results cannot be generalised as it has too many confounding variables.
It should be noted that the second part of the study, when the surgical checklists were added, occurred at the same time as the national lockdown as a result of COVID-19. This may have interfered with the final results as people were urged to stay at home and may have been able to monitor their animals more closely following surgery, so spotted more problems than they might have otherwise.
Possibilities for why there was no statistical significant includes but is not limited to: surgical teams being good and not making any mistakes that the checklists could catch; surgical teams being bad and the checklists could not improve the outcome; cohort size; study design; or COVID-19 and a national lockdown interfered with the results.
Limitations
The time allocated for this study was limited to 8 weeks, meaning there was limited opportunity to obtain participants for the study. With more time the study would be able to get a larger pool of participants, providing a better sample (Wright, 2017). As the patients' postoperative checks were performed between 3–10 days after the operations, complications occurring weeks or even months after the procedures were not taken into account, meaning that the true results from the study might not yet be known. Further studies to investigate long-term outcomes could be beneficial.
The study could have been improved by minimising the variables, such as only including one species and one procedure and excluding those patients that were administered antibiotics. More consideration could also have been given to the likeliness of complications in minor and major procedures.
Conclusion
Following the application of surgical safety checklists, the practices that participated in this study experienced a 4% decrease in postoperative complications, which was not statistically significant. These results do not contradict previous results achieved through studies within veterinary medicine (Bergström et al, 2016; Cray et al, 2018; Launcelott et al, 2019) as well as similar studies conducted within human medicine. This study was conducted in a similar way to the Swedish study by Berg-ström et al, using the same methodology and grading of complications. The study by Bergstrom (2016) showed a 10% decrease in complications following the introduction of a checklist.
It is important to note that the checklist assumes that the practitioners are ensuring that steps not mentioned in the checklists are also followed, such as sterility of the surgical field, and the veterinary surgeon performing the surgery is competent and confident in the procedure. Therefore further research is needed in areas including, but not limited to, surgical sterility, patient interference and owner compliance.
The AVA produced a checklist that is available for download online. This means that veterinary practices all around the world are able to implement the checklists without cost, and potentially improve their surgical outcomes. With larger studies, the performance of these checklists can be more accurately assessed, and further studies could benefit from removing variables such as differing species and procedures as well as ensuring consistency in study design and methodology.
KEY POINTS
- Surgical safety checklists, when applied correctly, can reduce the risk of postoperative complications.
- Surgical safety checklists should not be a replacement for surgical sterility or good surgical technique.
- Comprehensive surgical safety checklists can be accessed for free, online.
- Surgical safety checklists have been shown to be effective within human medicine.
- Further research is needed to fully determine the effectiveness of surgical checklists within the veterinary world.


