Cardiac disorders are a particularly important consideration in anaesthesia because many of the main side effects of most analgesic and almost all anaesthetic drugs is cardiovascular depression. In turn, heart diseases can have pharmacokinetic effects on the drugs utilised, for example poor peripheral perfusion may result in lowered drug bioavailability after sub-cutaneous or intra-muscular injection (Clutton, 2007). Heart disease can be evident in veterinary patients in many forms so it is first important to ascertain the nature of the problem. An understanding of the anatomy and physiology of the cardiovascular system is also important to critically evaluate how different anaesthetic and analgesic drugs will affect the system, and whether these effects will be beneficial or detrimental to different heart diseases. There is no single protocol that will be effective in all patients with heart disease due to the differing pathophysiology of these disorders. There are differing opinions on drugs for use in cases with heart disease between specialist veterinary anaesthetists and the recommendations provided by textbooks and continuing education articles are generally based on personal opinion as there is an extremely limited clinical evidence base. Often drugs and drug combinations that are recommended in these cases are unlicensed and veterinary surgeons and nurses may have limited experience of their use and side effect profiles. A prime example of this is the induction agent etomidate which is often recommended, but not licensed or widely available in the UK (Figure 1).

A good working knowledge of the cardiovascular effects of the common anaesthetic, analgesic and sedative drugs is fundamental to safe anaesthesia and this is all the more important when dealing with a case that has altered cardiac function. It is also important to recognise that the sometimes subtle differences between drugs may become more relevant in patients with cardiac disorders, e.g. alfaxalone will maintain heart rate more than propofol during the induction period as it has been suggested that propofol blunts the baroreceptor reflex (Sellgren et al, 1994; Muir et al, 2008).
Cardiac disorders
It will, of course, be the veterinary surgeon who makes a diagnosis of cardiovascular disease and develops an anaesthetic plan, but veterinary nurses must have an awareness of the condition and how it will affect the anaesthetised patient. This is required in order to discuss potential adverse events with the veterinary surgeon so an appropriate plan can be made for any complications that may arise. One critical decision which the veterinary surgeon will have to make is whether the risks of anaesthesia outweigh the benefits of performing the proposed procedure. The degree of increased anaesthetic risk to a patient that has a particular cardiovascular disease is not known, however it is likely that the more a patient is affected by the disease, the greater the risk. Therefore, it may be necessary to postpone a procedure to allow further diagnostics or stabilisation, or even to cancel it altogether if it is an elective procedure.
Common cardiac disorders that may be encountered in dogs and cats include: mitral valve disease (MVD)(dogs); dilated cardiomyopathy (DCM) (dogs); hypertrophic cardiomyopathy (HCM) (cats); aortic stenosis (dogs); pericardial effusion; and arrhythmias such as atrial fibrillation (AF) and ventricular tachycardia (VT). It is important to discuss and evaluate: how much the cardiac disorder is affecting the patient; whether any further investigation is warranted prior to anaesthesia; whether the patient can or should be stabilised further; whether the patient is on any medication and if so what the side effects and interactions of them may be; and whether there are any other comorbidities.
While the veterinary surgeon will have performed a full history and clinical examination it is important for the nurse monitoring the case to assess the patient for themselves to ascertain normal baselines. Historical signs such as cough, breathing difficulties, panting, collapse and exercise intolerance should all raise alarm bells and warrant further discussion with the veterinary surgeon. Clinical examination parameters such as pulse quality and rate; heart rate and rhythm; mucous membrane colour and capillary refill time; respiratory rate, pattern and effort; heart and lung sounds, may all be altered and can help to indicate the degree to which the patient is being affected by the heart disease (Clutton, 2007). Once the clinical examination has been performed by the veterinary nurse, the case should be discussed with the veterinary surgeon and likely adverse events identified and prepared for. These will be largely dependent on the particular cardiac condition diagnosed and the severity of the disease.
Anaesthetic considerations
In all cardiac cases stress should be kept to a minimum and one important nursing factor to consider is minimal restraint. Both stress and pain can alter heart rate, increase circulating catecholamines and increase myocardial oxygen demand and these are all factors that could cause a previously stable patient with cardiac disease to destabilise during the peri-anaesthetic period. It is also important to remember that the provision of adequate analgesia will undoubtedly reduce the amount of anaesthetic induction and maintenance agents required and it is these agents that often have the more detrimental effects on the cardiovascular system. Consequently pain assessment and adequate analgesic provision is key in these cases (Curtis-Uhle and Waddell, 2010).
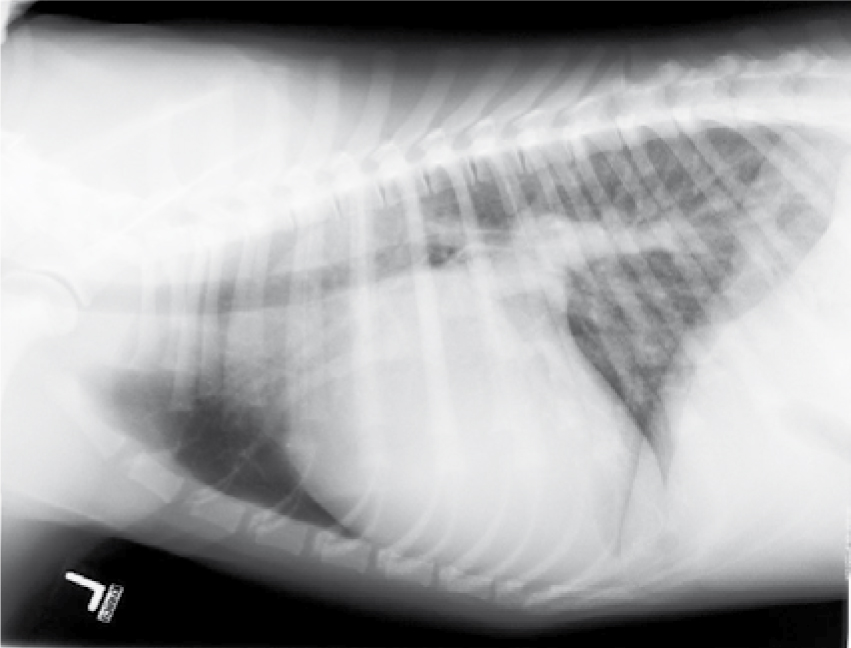
When preparing an anaesthetic plan it should be considered that almost all cardiac disorder cases will benefit from pre-oxygenation unless performing this causes undue stress (Figure 2). It is also vital that fluids be carefully managed in order to avoid fluid overload, which can readily lead to congestive heart failure and consequences such as pulmonary oedema and pleural effusion (Rush et al, 2002) (Figure 3). A number of additional drugs may be warranted if adverse events are encountered and it is important to consider these prior to anaesthesia so they can be close to hand, with the appropriate drug doses calculated, during anaesthesia. Depending on the underlying disease process anti-arrhythmics (e.g. lidocaine), anticholinergics (e.g. atropine), vasopressors (e.g. noradrenaline) and inotropes (e.g. pimobendan and dobutamine) may be indicated (Figure 4). Beyond this, knowledge of the diagnosed or likely heart disease becomes important as each disease process affects physiology in a slightly different way which in turn affects anaesthesia.


MVD
One of the most common heart abnormalities detected in dogs is mitral valve regurgitation. Mitral valve regurgitation is commonly seen with acquired heart diseases in dogs, often being caused by MVD or DCM. MVD is highly prevalent in small breed dogs, especially the Cavalier King Charles Spaniel, but can occur in medium to large breed dogs. It is more common in geriatric dogs, but may also be found in younger patients. The diseased and dysfunctional valve leads to a proportion of the ejected fraction of blood regurgitating (flowing back) from the ventricle into the atria during systole. This reduces the stroke volume and as such decreases cardiac output and subsequently blood pressure. The body has to compensate to maintain blood pressure by increasing heart rate, retaining water and sodium through increased resorption in the kidney and through peripheral vasoconstriction. Pulmonary venous pressure can gradually increase, which may in turn lead to pulmonary congestion and ultimately oedema.
When thinking about the pre-medication, it is important to consider the effects of vasoconstriction and vasodilation on the patient's cardiac condition. If vasoconstriction occurs in a patient with mitral valve regurgitation (e.g. following medetomidine administration) then the downstream vascular resistance will increase making forward blood flow more difficult. The regurgitated fraction and myocardial workload will be increased and cardiac output will be reduced. This is often worse when patients are symptomatic as it becomes increasingly difficult for the heart to compensate. Sedative drugs that cause vasodilation may provide a better alternative as these will decrease downstream resistance, encourage forward flow and decrease the regurgitated fraction. This may improve cardiac performance through increasing cardiac output without significantly increasing myocardial workload. However, it is important to note that doses will need to be adjusted as the dog may not be able to fully compensate for the vasodilation. Other anaesthetic considerations for patients with MVD include maintaining preload (central venous pressure), minimising changes to myocardial contractility and aiming to maintain the heart rate near to the conscious normal for the patient (Dugdale, 2010).
DCM
DCM is most commonly seen in large breed male dogs such as Doberman Pinschers and Great Danes (Clutton, 2007). This disease is characterised by severe, left ventricular systolic dysfunction due to the thin dilated wall of the left ventricle. Stroke volume can be severely compromised by the reduced contractility and therefore cardiac output reduces. Again compensation occurs through increasing heart rate, vasoconstriction and water and sodium retention. Atrial and ventricular arrhythmias are common with DCM and left and right heart failure in combination with pulmonary oedema usually eventually developing (Clutton, 2007). Pleural effusion and pulmonary oedema, if present, should be managed where possible by the veterinary surgeon using diuretics and/or thoracocentesis prior to anaesthesia. It is likely that these patients may be on medication to manage heart failure at the time of anaesthesia. The last dose of each medication should be noted on admission and any potential side effects and drug interactions discussed between the veterinary surgeon and registered veterinary nurse involved in the case. Reduced myocardial compliance in these cases means that cardiac output becomes reliant on heart rate so anaesthesia aims to avoid large changes in heart rate and maintain central venous pressure (preload) through fluid therapy (Dugdale, 2010). In terms of anaesthetic drugs for dogs with DCM, one experimental study looking at propofol in dogs with induced DCM has been published (Pagel et al, 1998). Propofol was demonstrated to reduce preload and afterload, and decrease inotropy, but had limited effect on heart rate (Pagel et al, 1998). This indicates that propofol had both favourable and unfavourable effects in dogs with DCM. It should be noted that no studies investigating alfaxalone use in dogs with DCM have been published to date.
Left ventricular outflow tract obstruction (LVOTO)
Another commonly encountered problem that requires a slightly different approach compared with MVD and DCM is that of LVOTO. LVOTO disrupts flow of blood from the heart and is commonly caused by aortic stenosis in dogs and HCM in cats. The narrowing of the left ventricular outflow tract (due to a stenotic valve, or myocardial hypertrophy, or anterior motion of the mitral valve during systole) will increase the resistance to forward flow of blood resulting in turbulent flow with a high velocity. This increases myocardial workload and reduces myocardial blood flow, but stroke volume tends to remain fairly fixed. Vasodilation should be avoided in these cases because if vasodilation occurs (e.g. through administering acepromazine), the downstream vascular resistance decreases, the pressure gradient across the LVOTO increases, and blood flow turbulence increases. This will in turn increase myocardial workload and decrease cardiac output. In this situation it becomes increasingly hard for the heart to compensate as the harder it pumps the greater the pressure differential becomes. Anaesthesia should aim to maintain the pressure drop across the obstruction as much as possible and ensure adequate pre-load (Dugdale, 2010). Cardiac depression should be minimised and changes to contractility should be minimised (Dugdale, 2010). Drugs that provide an element of vasoconstriction alongside the sedation required for premedication may be advantageous in these cases. Vasoconstriction will increase the downstream vascular resistance and decrease the pressure differential across the left ventricular outflow tract. This will reduce the turbulence and velocity and may help to improve the performance of the heart.
HCM
HCM is the most commonly diagnosed cardiac disorder in cats. Despite this it is probably underdiagnosed, with approximately 15% of perceptually ‘normal’ cats with no heart murmur detected on auscultation having HCM (Paige et al, 2009). HCM is characterised by a stiff left ventricle with poor diastolic function, but systolic function may also be affected (Tranquilli et al, 2007). One clinical sign specific to cats with heart disease is the presence of a gallop rhythm. This is not an arrhythmia, but the presence of an additional heart sound which makes the heart sound like a galloping horse. The presence of a gallop rhythm may be a sign that the cat's heart is struggling and beginning to decompensate (Payne et al, 2013). In these cases stress is perhaps worse than the side effects of many analgesic and anaesthetic drugs. Anaesthesia, fluid therapy and surgery have been identified as risk factors for the development of congestive heart failure in cats with HCM (Rush et al, 2002). Interestingly, medetomidine has been demonstrated to improve cardiac performance in a small study of cats with HCM and associated LVOTO (Lamont et al, 2002). This suggests that alpha-2 agonists can perhaps be used safely in these cats, however they should be used with caution; perhaps only being used in asymptomatic cats. Clinical signs such as the absence of a gallop rhythm or the finding of a large left atrium seen on echocardiography or thoracic radiography should act as a warning sign that the cat could deteriorate following anaesthesia.
Pericardial effusion
Pericardial effusion where fluid accumulates in the pericardial sac surrounding the heart may result in cardiac tamponade. This results in an inability of the heart to pump effectively and maintain cardiac output as the low pressure atria (especially on the right) are unable to fill. This can be idiopathic, neoplastic, traumatic or iatrogenic in origin and results in reduction of left ventricular stroke volume. Clinical signs may include: jugular distension and pulsations; muffled heart sounds; tachycardia; hypotension; ascites; pleural effusion and pulmonary oedema (Dugdale, 2010). The veterinary surgeon will need to consider whether the drainage of some of the pericardial fluid before induction may significantly improve the patient's anaesthetic outcome, however this process may require anaesthesia to perform safely. Reduction in heart rate should be avoided and intravenous fluid therapy to maintain venous return should be used cautiously to avoid fluid overload (Dugdale, 2010).
Arrhythmias
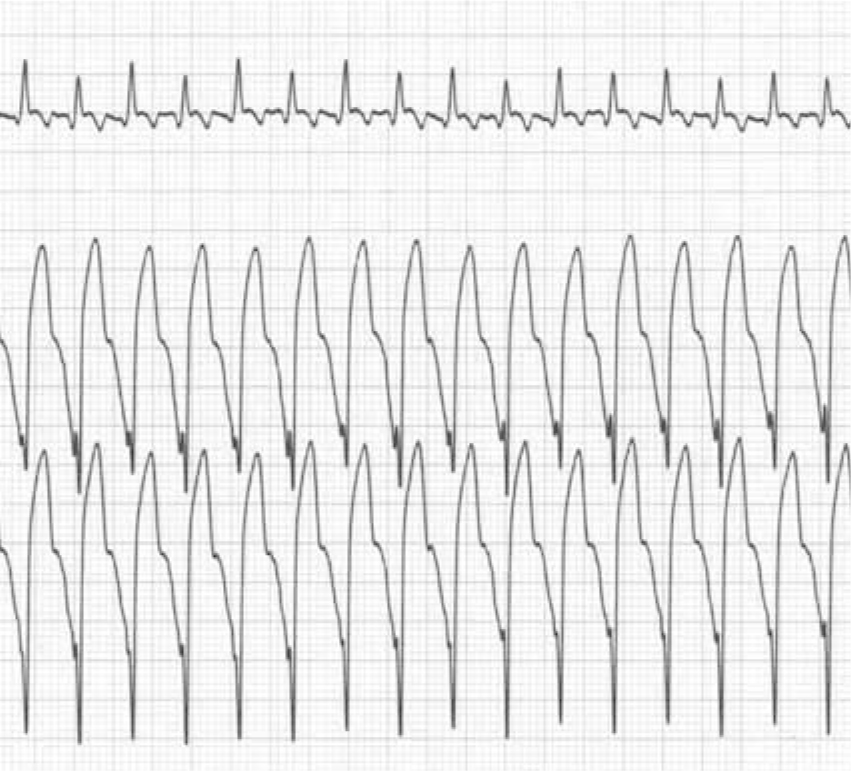
Arrhythmias can be standalone cardiac disorders or may develop secondary to cardiac disease; arrhythmia such as AF (Figure 5) and VT (Figure 6) may be caused by either. AF is common in some large breeds of dog including Wolfhounds and Great Danes and may be secondary to DCM or atrial enlargement secondary to MVD (Menaut et al, 2005). If AF is suspected then an electrocardiogram should be observed prior to anaesthesia as a diagnosis of AF may alter the decision for surgery especially if elective. AF is identified on clinical examination as an irregularly irregular rhythm which often has pulse deficits when associated with a high heart rate. Echocardiography to assess cardiac rate and rhythm should also be performed. VT is also a relatively common problem which can be primary or secondary in nature (Figure 6). Abdominal diseases such as splenic neoplasia or pancreatitis as well as cardiac diseases can cause VT. Breeds such as the Boxer are prone to developing VT, which may or may not be associated with arrhythmogenic right ventricular cardiomyopathy. In most situations in animals with pre-existing arrhythmia, attempts to stabilise the rhythm disturbance before anaesthesia should be attempted as the cardiovascular effects of the arrhythmia may become more pronounced under anaesthesia. This is because, for both AF and VT, when heart rate becomes very fast the cardiac output will begin to drop as the atria are unable to contribute to ventricular filling. Filling is therefore passive and is dependent on preload and diastolic time (which will be shortened during tachycardia). Blood pressure and perfusion will therefore drop. Anaesthesia involving both of these arrhythmias should be aimed at managing heart rate by reducing sympathetic drive and thus managing increases in heart rate — this is generally achieved through the administration of appropriate analgesics. Anti-arrhythmic agents, such as lidocaine for VT, should be available during the perianaesthetic period.

As a general rule the minimum effective dose of induction agents should be used which can be achieved through slowly administering drugs such as alfaxalone or propofol to effect. The use of inhaled anaesthetic agents should be minimised and this is most effectively achieved through the optimisation of analgesia. Fluids should be carefully administered at cautious rates, ideally using fluid pumps or syringe drivers (in the case of cats and small dogs), in order to avoid over administration.
Monitoring of cardiac patients where possible should include general clinical parameters, blood pressure, ECG, alongside capnography and pulse oximetry. Monitoring should be continuous as much as possible during the recovery period until the patient appears to be fully recovered. After this, care should be still be taken to regularly monitor the patient as anaesthesia may cause acute deterioration in an animal's cardiac condition (Rush et al, 2002). Care should be taken to monitor: respiratory rate and effort; pulse rate, rhythm and quality; and heart rate and rhythm, all of which may alter following deterioration in the patient's condition.
Conclusion
The veterinary surgeon should be alerted to any abnormalities or changes in parameters that are detected. For example the development of a gallop rhythm following anaesthesia in a cat is a significant sign of deterioration. Again appropriate analgesia tailored to the patient perhaps through the use of pain scoring methods such as the Glasgow Composite Pain Scales for dogs and cats should be administered to reduce the impact of increased sympathetic tone and stress on the patient. The veterinary nurse's approach to patients with cardiovascular disease undergoing anaesthesia involves preparing for the potential problems that may be encountered, awareness of the patient's condition and the effects on anaesthesia and an understanding of drug effects on the cardiovascular system. All cardiovascular diseases are not the same and different drugs will be considered appropriate by the veterinary surgeon for different conditions.

