Head trauma is a common emergency presented to veterinary clinics, and injuries can be fatal: Sharma and Holowaychuk (2015) reported a mortality rate of 18–24% in dogs. However, treatment and nursing care of head trauma patients can be very rewarding, and the majority of patients recover and return home as long as prompt nursing and medical treatment are initiated (Elias et al, 2019). Brain injury can be classified as either primary or secondary. Primary brain trauma is when there has been direct trauma and force applied to it including accelerating, decelerating or rotational forces, which the brain is unable to tolerate because of the lack of support around it, leading to skull fractures and cerebral haemorrhage (O’Dwyer, 2013). Common causes of primary head trauma include: road traffic accidents; falling from heights; kicks to the head; gunshot wounds or animal bites (Lowrie, 2013).
Secondary head trauma occurs anywhere between minutes to days after the initial primary impact. During this time bio-molecular events happen causing continuing and progressive brain pathology (Elias et al, 2019). Haematomas and oedema caused by the primary injury cause changes to the normal brain parenchyma and reduce cerebral blood flow (O’Dwyer, 2013). Primary damage is beyond the control of the veterinary team, it cannot be prevented, therefore the main focus of veterinary intervention is prevention, recognition and treatment of the secondary brain injury (Elias et al, 2019).
The Brain
The brain, along with cerebrospinal fluid and intracranial blood, make up the cranial space, which is all enclosed by skull (Elias et al, 2019). The pressure within the skull, the intracranial pressure (ICP), is tightly regulated to ensure it remains stable. The intracranial blood volume must also be maintained within the normal range because of the high metabolic demands of the brain. Although it only represents 2% of the body's weight, the brain receives 15–20% of the cardiac output with every heartbeat (Lowrie, 2013). ICP is determined by the cerebral perfusion pressure (CPP) and mean arterial pressure (MAP). CPP is the force that drives blood into the calvarium to provide essential oxygen and nutrients to the brain parenchyma and determines the cerebral blood flow, the normal range of which in dogs and cats is 5–12 mmHg (Elias et al, 2019). Blood pressure, cerebral metabolic rates, blood carbon dioxide and oxygen concentrations all have a significant effect on the cerebral blood flow (Lowrie, 2013).
Head trauma causes the volume of the cranial space to increase, because of oedema or haemorrhage, and as this volume increases the cerebrospinal fluid and blood compartments must decrease or the ICP will increase (Platt and Olby, 2017). To regulate against rises in ICP, translocation of cerebrospinal fluid out of the skull occurs and this is followed by a reduction in the production of cerebrospinal fluid and ultimately therefore a decrease in cerebral blood flow. However, this compensatory mechanism will eventually become exhausted and a small further increase in intracranial volume will cause a dramatic elevation in ICP. Additionally, autoregulation cannot occur if the blood– brain barrier has been destroyed as a result of trauma, and this means that cerebral perfusion passively follows; therefore, minor decreases in MAP that may be perfectly safe in a healthy patient may cause a dramatic decrease in cerebro-spinal fluid (Lowrie, 2013).
Why Intracranial Pressure is so Important
ICP is vitally important because of its direct effect on cerebral perfusion. It is the pressure exerted between the intracranial tissues: cerebral blood volume, cerebrospinal fluid and brain tissue and the solid skull (Lowrie, 2013), and hence rises in ICP are responsible for the clinical neurological decline after head trauma (Platt and Olby, 2017). Cerebral perfusion (CP) becomes reduced when ICP increases, and CP is calculated by: CP = MAP – ICP.
Systemic blood pressure increases to try to prevent any decrease in perfusion as well as cerebral blood flow. Therapy should be aimed at maintaining MAP within 50–150 mmHg (Lowrie, 2013). The increased reliance on MAP for cerebral blood flow has been suggested to be one of the reasons for a poor prognosis in patients with hypotension following a head injury (Lowrie, 2013).
A marked increase in ICP triggers a reflex known as the Cushing's reflex; the rise in ICP causes the cerebral blood flow to decrease which leads to a build-up of carbon dioxide (CO2) levels. This increase in CO2 is detected at the vasomotor centre in the brainstem. The sympathetic nervous system responds by increasing MAP which is detected in the baroreceptors in the walls of the carotid arteries and aortic arch, which results in reflex bradycardia (Platt and Olby, 2017). The reduction in heart rate mixed with an increase in MAP are indicative of increased ICP. Other signs of increased ICP include anisocoria, miosis, mydriasis, altered mentation, loss of motor function, development of vertical nystagmus and extensor rigidity. These are the clinical signs veterinary nurse must be primed to respond to (Platt and Olby, 2017).
Patient Triage
Initial assessment of any patient presented to an emergency clinic should follow the ABC: airway, breathing, circulation protocol. It is easy to be distracted by the obvious problem of the trauma to the head, however, assessment should always involve checking the airway as there could be debris or swelling in the oral cavity caused by the impact.
Assess if the patient is breathing normally if they are unconscious, because they may need to be intubated or manually ventilated if they are apnoeic or dyspnoeic as respiratory dysfunction can be common following head injury (O’Dwyer, 2013; Platt and Olby, 2017). Respiratory dysfunction occurs as a result of neurogenic pulmonary oedema, which results from sympathoadrenal overstimulation caused by marked peripheral vasoconstriction and increased venous return. This results in increased ventricular afterload and increased pulmonary capillary hypertension, leading to oedema, which causes severe dyspnoea, tachypnoea and eventually hypoxaemia (Platt and Olby, 2017).
Assess if the patient had a normal heart rate and rhythm, and if the rate is synchronous with the pulse. If not, an electrocardiogram is indicated. It is also vital to monitor blood pressure, because an increased MAP with bradycardia is indicative of increased ICP and potentially impending brain herniation, and the veterinary surgeon should be alerted immediately (O’Dwyer, 2013).
A primary survey should also include assessment of neurological function focusing on mentation, brain stem reflexes and motor activity — the Modified Glasgow Coma Scale can be used and is discussed in more detail later.
Oxygen should be provided to all patients that have suffered head trauma until their cardiovascular and respiratory status is considered to be stable (Lowrie, 2013). It is important that oxygen supplementation is tolerated by the patient as any coughing, sneezing or struggling can cause an increase in ICP, therefore, it is advisable to avoid using nasal oxygen catheters in favour of flow by or oxygen cages with adequate temperature control (Elias et al, 2019).
If the patient is deemed to be stable then a full physical examination should be carried out (Figure 1) and findings documented. Presenting vital signs must be documented as they will become a reference of the patient's condition at the time of presentation and used to monitor for deterioration, as head trauma patients can deteriorate very rapidly and must be monitored closely (O’Dwyer, 2013).

Monitoring trends in the patient's clinical parameters is a vital part of a nurse's role in critical care, and the practice should be suitably staffed to deal with the high demands of an intensive patient, allowing for any changes in the patient's status to be noted, investigated and treated promptly (Humm and Kellett-Gregory, 2016.)
Neurological Assessment
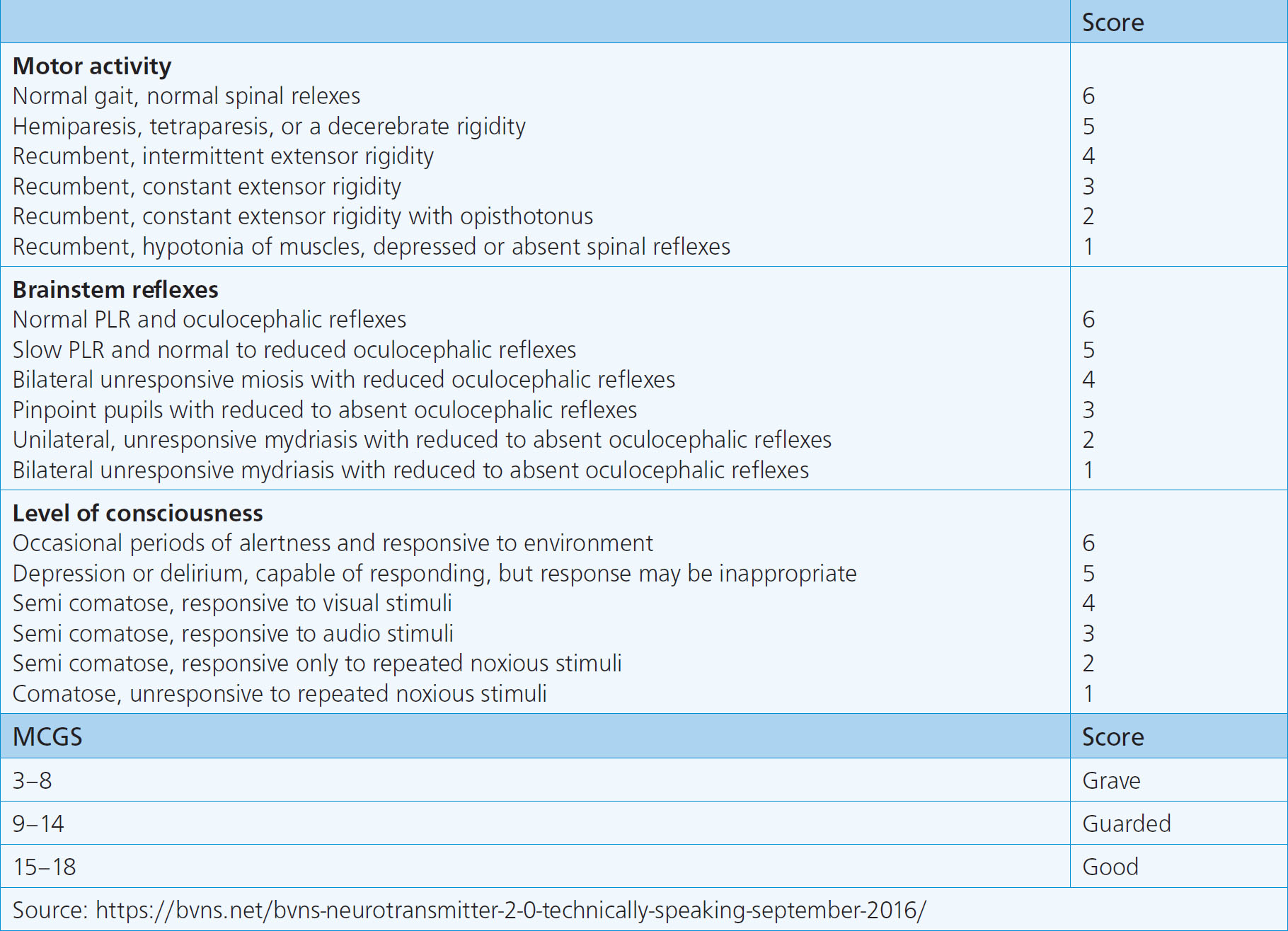
The patient's level of consciousness should be ascertained and the Modified Glasgow Coma Scale is an effective tool to use to assess this (Figure 2). This scoring system uses three categories of examination: level of consciousness; motor activity; and brainstem reflexes (Platt and Olby, 2017). Each category is given a score of 1–6 providing an overall score of 3–18 this allows serial measurements to be taken to assess prognosis as well as progression or regression of the neurological signs. Sharman and Holowaychuk (2015) stated that the probability of survival is positively correlated with the Modified Glasgow Coma Scale score and suggested that a score of 8 within 48 hours of hospital admission predicts a 57% probability of survival. Therefore, the Modified Glasgow Coma Scale is a very effective bedside measurement that can be used by the veterinary team to guide decisions in an emergency setting. However, the scale should not be relied on as the sole indicator of survival, but used alongside serial measurements of vital signs (Sharman and Holowaychuk, 2015).
It is imperative to be able to recognise elevations in ICP and declining neurological status to manage patients with head trauma. Unfortunately, once the threshold for ICP has been reached and autoregulation is no longer possible there will be a rapid increase in ICP with only a small increase in intracranial volume; from continuing haemorrhage, for example, there will then be an immediate decline in the patient's neurological status and brain herniation will occur (Lowrie, 2013). Therefore, neurological deterioration will likely only occur at the end stages of the process so treatment measures should be aimed at helping to reduce intracranial volume.
Monitoring and Stabilisation
The major nursing concerns when presented with a patient having suffered head trauma are: oxygenation and ventilation; handling; positioning; analgesia and nutritional support (Opperman, 2014). As mentioned previously all patients should be provided with oxygen until cardiorespiratory function has been assessed. If a patient is presented unconscious then the airway should be protected, intubation is therefore necessary and constant monitoring should ensue (Opperman, 2014). Hyperventilation can rapidly decrease ICP because of hypocapnia causing cerebral vasoconstriction, which in turn decreases cerebral blood flow, therefore oxygenation should be monitored using pulse oximetry or blood gas analysis (Vite and Galban, 2018). However, jugular blood sampling is contraindicated because of the increase in ICP raising a jugular vein will cause, so a peripheral sample is recommended and this can be taken at the same time an intravenous catheter is placed, which will be vital for the administration of fluid therapy or anticonvulsant drugs should they be required.
Careful handling of patients during nursing interventions such as intravenous catheter placement or phlebotomy is imperative. Causing stress to the patient will increase blood pressure and subsequently will increase ICP, therefore sedation may be necessary; Opperman (2014) suggested that diazepam and ketamine can be used for this purpose. Ketamine is also thought to have a protective effect against cerebral ischaemia. Noise and light levels should also be reduced to prevent patient distress, although the patient should be always within view so they can be constantly monitored.
Positioning is important in patients that are unable to move to prevent aspiration in the occurrence of regurgitation, as well as to keep them comfortable. However, traditional positioning of raising the head to prevent passive regurgitation is outdated as the only direction for the fluid to go if regurgitation did occur would be directly back down the oesophagus and trachea causing aspiration pneumonia (Opperman, 2014). Raising the head over 30° angle is contraindicated as this can increase the ICP, however, some elevation of the head will facilitate venous drainage and reduce ICP (Vite and Galban, 2018). It is advisable to keep the shoulder raised so any regurgitation can flow away from the airway and exit via the mouth. Inducing retching, coughing, sneezing and gagging should all also be avoided because of the increase in blood pressure and thus increase in ICP these cause (Vite and Galban, 2018).
Pupillary size and light response, posture and any signs of seizure activity will also need to be frequently observed and documented. Pupil size is used as a prognostic indicator: a constricted responsive pupil has a more favourable prognosis than a dilated unresponsive pupil. Ocular position and any nystagmus or anisocoria should be documented as well, and care should be taken as stress increases sympathetic tone and dilates the pupils reducing their normal response to light, especially in cats. It is therefore recommended to assess the patient in a calm environment (Lowrie, 2013). Comparing these findings to those at admission will allow changes that may indicate impending brain herniation to be reported to the veterinary surgeon immediately. Dedicating one veterinary nurse to the patient would be a recommended way to monitor these patients so that they receive one to one care and even subtle changes in responsiveness or vital parameters can be identified instantly (Humm and Kellett-Gregory, 2017).
The patient's posture may indicate if the brain is damaged as well as the area of the brain that has been damaged. Opisthotonus posture (Figure 3) can be observed in patients with head or spinal trauma and presents as forelimbs stretched out in front and the head thrown back. Equipment and drugs should also be prepared in case of seizure activity, a ‘seizure plan’ should be drawn up indicating the drugs and dosages needed if a seizure occurs, and the drugs should be to hand at the patient's bedside to allow for rapid administration. Seizure activity is likely in patients with depressed skull fractures and penetrating head wounds (Opperman, 2014).

Analgesia is imperative following a traumatic injury however, accurately pain scoring a patient that may have altered mentation is difficult, therefore it may be advisable to assume that in the presence of soft tissue trauma pain is present and should be treated (Opperman, 2014). Opioids are a common choice for analgesia, however, the sedation and respiratory depression they can cause may be of concern, this can be avoided by aiming to use the lowest dose required to achieve appropriate analgesia (Elias et al, 2019). Fentanyl in a constant rate infusion is often the drug of choice as it provides constant analgesia and is thought to maintain cerebral blood flow, as well as being a potent analgesic with a rapid effect and short duration of action which will help provide the opportunity for frequent reassessment of the patient (Kuo et al, 2018). Buprenorphine is more readily available in most veterinary practices and has less of an effect of the respiratory and central nervous system than other opiates (Opperman, 2014). Hydromorphone and morphine should be avoided because of the probability of inducing vomiting and thus a sudden increase in ICP, however, this is seen less often in patients experiencing pain (Leece, 2018).
Intravenous fluid therapy needs to be administered carefully to avoid overload, but should aim to maintain circulating volume and replace deficits. Monitoring fluid therapy via central venous pressure would be contraindicated in most cases because of the need for jugular occlusion, so fluid balance should be monitored by documenting urinary output, and a fluid pump must be used to prevent accidental overload (Opperman, 2014). Once vascular volume has been stabilised an osmotic diuretic such as mannitol can be administered (Platt and Olby, 2017).
Mannitol is a hypertonic crystalloid that is often used in head trauma cases because of its hyperosmolar effect, which rapidly decreases ICP. It has an immediate plasma expanding effect that reduces blood viscosity, which increases cerebral blood flow and oxygen delivery, this causes vasoconstriction within a few minutes and then an immediate decrease in ICP (Platt and Olby, 2017). Mannitol also has an effect on the blood-brain osmotic gradient, reducing extracellular volume in normal and damaged brain tissue therefore reducing the ICP (Platt and Olby, 2017). Mannitol should only be given if prescribed by the veterinary surgeon and is given in boluses over 15 minutes at a dose of 0.5–1.5 g/kg. It is imperative to make sure that it has not crystallised before administration, — warming the bag before administration will remove the crystals (O’Dwyer, 2013). The effect occurs approximately 15–30 minutes after administration and should last between 2 and 8 hours. Administration of mannitol will be accompanied by diuresis resulting in volume contraction and intracellular dehydration, hence why vascular volume needs to be stabilised before its administration (Platt and Olby, 2017). Withholding water post mannitol administration is recommended when it is used to treat glaucoma, however, when treating ICP normovolaemia should be maintained through isotonic crystalloid administration to avoid severe volume depletion (O’Dwyer, 2013; Senior, 2018).
Avoid mannitol in dehydrated, hypovolaemic patients and in patients with underlying cardiac disease or in hyper-osmolar states (i.e. significant hypernatraemia). Euvolaemia (through fluid administration) should be maintained during mannitol administration.
Nursing care plans must always consider all the patient's needs. A urinary catheter would be recommended to monitor urinary output and will avoid the need to move the patient to either clean away any urination or defecation or attempts to take them outside to urinate if they are recumbent. Nutritional support is also a vital part of the patient's ongoing veterinary care. The patient may be unable to feed themselves so a feeding tube may be required, unfortunately options for feeding tubes are limited as a naso-oesophageal tube may induce sneezing and coughing, and any other type of feeding tube would require a general anaesthetic and this may not be advisable in an unstable patient. Peripheral parenteral nutrition could be a short-term option although it has contraindications and complications because of the method of administration, such as issues with the catheter, contamination and sepsis and metabolic derangements (Michel, 2018). The patient may be unconscious and unable to eat or may be severely depressed, in which case the ability to swallow needs to be assessed. This can be done by testing the patient's gag reflex before offering food and making sure the patient is supervised when being fed and a sensible amount of food is offered.
Conclusion
Nursing patients with head trauma is intensive and requires stringent monitoring and attentiveness to the changes in the patient's condition. Particularly signs that indicate increases in ICP such as bradycardia with increased MAP, and increases in Modified Glasgow Coma Scale scores. Communication with the veterinary surgeon is vital so that prompt interventions to prevent brain herniation can be initiated. These include changes to positioning, administering intravenous fluid therapy, hyperosmolar drugs such as mannitol and importantly analgesia. However, for those armed with the knowledge and confidence in what to be monitoring for, and with vigilance within the veterinary team, these can also be extremely rewarding cases to manage.
Key Points
- Primary brain injury is a result of direct trauma due to accelerating, decelerating or rotational forces that the brain cannot tolerate because of lack of support, secondary trauma in the resulting biomolecular events that follow the initial impact.
- Intracranial pressure (ICP) is vitally important as increases directly impact the patient's neurological status and prognosis.
- The Cushing's reflex, an increase in mean arterial pressure with a decrease in heart rate, is indicative of a rise in ICP and potentially impending herniation and death.
- A systematic approach to assessment and stabilisation should occur before focusing on neurological assessment. The Modified Glasgow Coma Scale is an effective tool to monitor the neurological status and prognosis for a head trauma patient.
- Mannitol is a hypertonic crystalloid that has a hyperosmolar effect that reduces ICP, it should only be used if prescribed by the veterinary surgeon and vascular volume must be stabilised before its administration.
- Nursing interventions such as careful handling, positioning, pain scoring and nutritional support are paramount for successful patient outcomes.


