Pain management for veterinary patients can sometimes be lost in the overall care of the patient. Many clients are used to oral medications as the only means of pain management for their pets. There are many other options for pain management in canines; such therapies as therapeutic laser, targeted pulsed electromagnetic field (tPEMF) technology, ultrasound, acupuncture, and massage or passive range of motion (PROM) are additional ways to provide pain relief for canine patients for many conditions, diseases, surgeries, and injuries. All pain management therapies should be carried out under the direction of the veterinary surgeon or rehabilitation veterinarian.
Clients are becoming more open to complementary and alternative therapies for their pets and like to have other options available besides pharmacological to ease their pet's pain (Millis and Pryor, 2015). The veterinary nurse is a crucial member of the rehabilitation team and often carries out the therapies planned by the veterinarian for the patient's care. As the primary care-givers to their patients, nurses can leverage their knowledge and skill set to advocate for their patients (Tear, 2012).
Indications for pain therapies
Complementary and alternative pain management therapies can be used for a number of conditions in canine patients, either alongside traditional medications or alone. The most notable indication for these pain therapies would be for post-operative patients, especially those patients that have orthopaedic or trauma repair procedures.
Patients recovering from surgery, typically orthopaedic in nature, benefit greatly from combined therapies (Levine and Millis, 2014). The laser and tPEMF technologies help to reduce inflammation and quicken the healing process by stimulating the cells around the surgery site (Levine and Millis, 2014).
Massage and PROM therapies help to bring movement, relax the joint, and work the muscles around the surgery site. This helps to avoid tightness of the joint and promotes proper healing and muscle building in the area (Levine and Millis, 2014).
Geriatric patients and patients with weakened joints, arthritis, or neurologic disease processes all benefit from these therapies (Levine and Millis, 2014).
Complementary and alternative therapies help to ease pain and stiffness in joints, encouraging patients to be more willing to participate in exercises and stay mobile. They also help to stimulate neural pathways communicating with the patient's brain and encouraging healing and maintenance of function, even in old age (Levine and Millis, 2014).
Therapeutic laser therapy
Therapeutic laser therapy (Figure 1) has been seen to improve the patient in several ways (Table 1). Laser therapy helps to reduce pain, reduce inflammation, and promote healing within the body. The laser is a physical light that penetrates the patient's body and promotes healing from within, using photobiostimulation (Levine and Millis, 2014). Laser units come with settings for various physical conditions, along with other factors such as the patient's weight, hair density, skin colour. The intensity and depth of the laser is altered by these factors to provide the ideal therapy for the patient (Pryor and Millis, 2015).

Table 1. Benefits of laser therapy (Pryor and Millis, 2015)
| Increase in serotonin |
| Increase in beta endorphins (receptors reduce the sensation of pain) |
| Increase NO, which may enhance oxygen delivery |
| Decrease bradykinins which induce the sensation of pain |
| Normalisation of ion channels |
| Block depolarisation of C-fiber afferent nerves |
| Increase nerve cell action potential |
| Improve axonal sprouting and nerve cell regeneration |
| ATP production |
| Stimulation of vasodilation by induction of NO |
| Stabilisation of cellular membranes |
| Acceleration of leukocyte activity |
| Decrease prostaglandin, synthesis |
| Enhance leukocyte infiltration |
| Increase macrophage activity |
| Early epithelialisation |
| Increased growth factors |
| Greater wound tensile strength |
Laser therapy is indicated for many conditions including: post-surgical treatment, nonoperative muscle ligament, or tendon injury, nerve damage, arthritis, post-surgical incisions, wounds (Levine and Millis, 2014). It eases pain, reduces oedema, improves scarring of tissues, increases healing rates, aids in nerve regrowth, and reduces inflammation.
Caution must be used when working with a laser unit. The two classes of therapeutic laser used in physical rehabilitation—class 3B and 4 — can cause eye damage (Levine and Millis, 2014). Eye protection should be worn by both the patient and any personnel in the room that the laser is being operated (Figure 2). The laser can cause injury to personnel and patients if not used properly and at the recommended dosages. Training courses should be taken before operating a laser unit on a patient. Veterinary nurses can perform laser therapy under the direction of the veterinarian.

It is best to have the patient's fur clipped to allow for better penetration of the laser. However, laser therapy can be performed on patients as long as their hair is clean and there are no matts.
Targeted pulsed electromagnetic field therapy
tPEMF therapy is a magnetic pulse used to relieve pain and promote healing in patients. It is Food and Drug Administration approved for both canines and humans for this purpose. The magnetic pulses mimic those produced by the healthy tissue in the body speeding the healing process by stimulating cells needed for re-growth and healing. This can be used in conjunction with laser therapy.
This type of therapy can be used in patients with any need for healing from post-surgery to arthritis. The therapy is performed with the patient either laying on a tPEMF mat or by using a tPEMF loop placed around the site of the body that needs aid (Figure 3a and 3b). Such products are sold by companies such as Assisi Animal Health: https://assisiani-malhealth.com/.
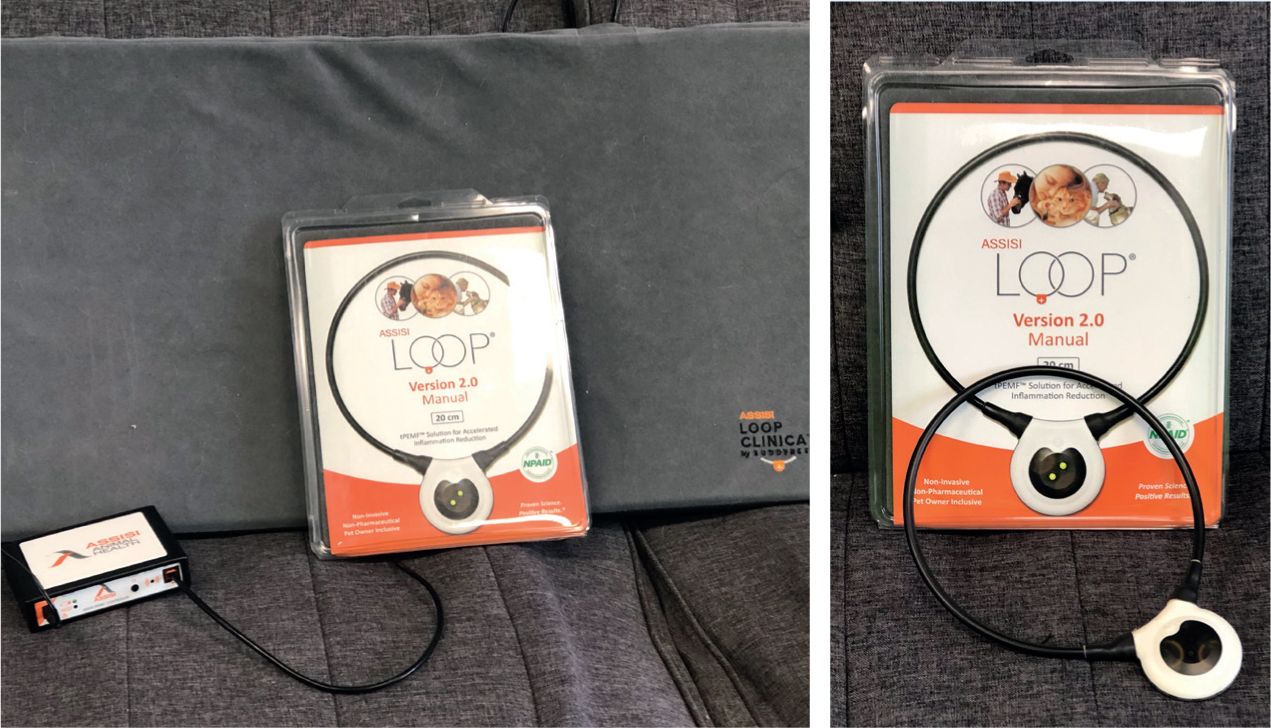
This therapy can be performed up to three times a day. At the author's veterinary rehabilitation practice, this therapy is performed at the same time that the laser therapy is given. This is done at the beginning of the session to warm up the affected area and provide pain relief, so the patient is ready to work on physical exercises (Levine and Millis, 2014).
Acupuncture
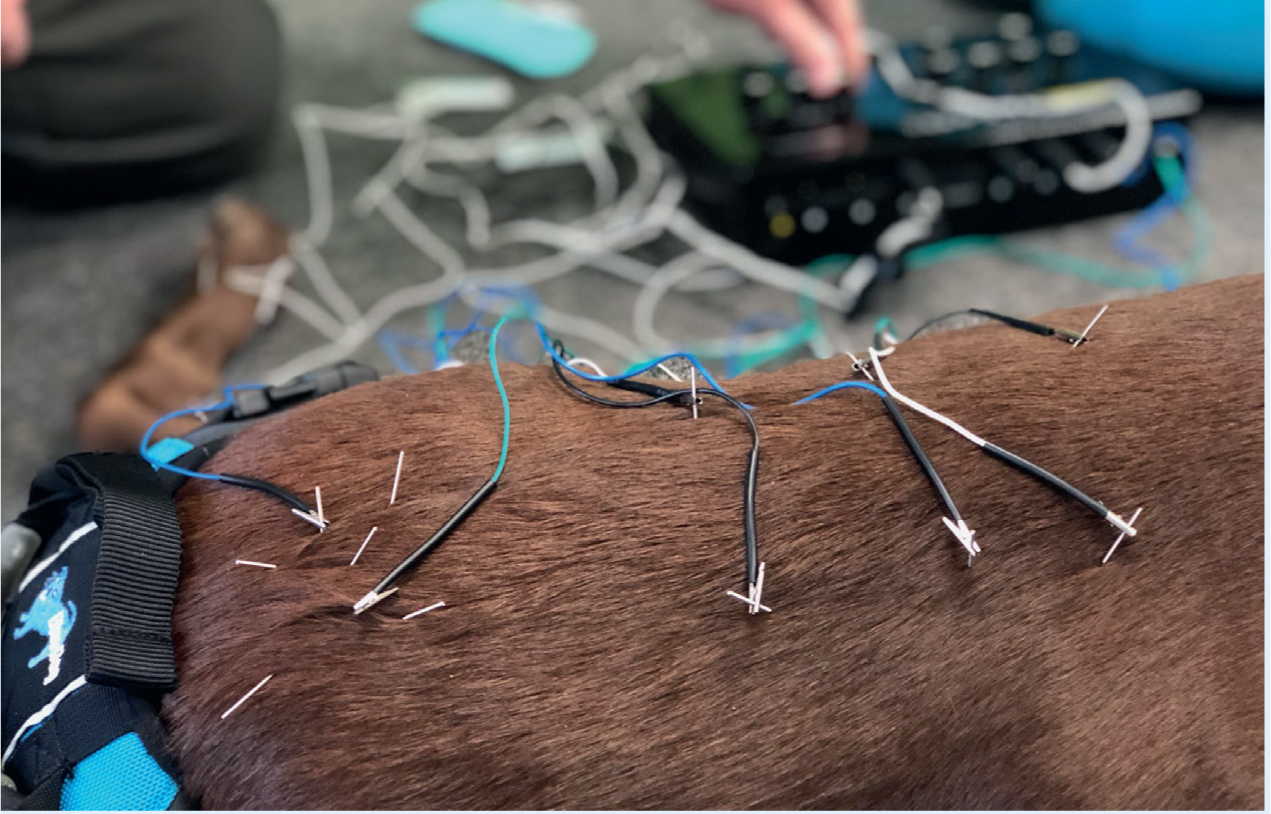
Acupuncture is perhaps one of the most well-known and accepted alternative pain management therapies. The term acupuncture is derived from the Latin word ‘acus’, which means needle, and puncture, and means ‘to pierce with needle’ (Figure 4a) (Bassert and Thomas, 2014) Acupuncture for pain management can be defined as a physiologic therapy co-ordinated by the brain that responds to the stimulation of manual or electrical needling of the peripheral sensory nerves, in which acupuncture does not treat any particular pathologic system, but normalises physiologic homeostasis and promotes self-healing (Levine and Millis, 2014).

Acupuncture is not performed with just needles. Acupuncture points can be stimulated by pressure, injection of fluid, laser, therapeutic ultrasound, surgically implanted material, and electricity (Figure 4b) (Bassert and Thomas, 2014). Acupuncture can be used to treat musculoskeletal, neurologic, cardiovascular, respiratory, gastrointestinal, reproductive, and dermatologic disorders (Bassert and Thomas, 2014)
Massage and passive range of motion
Physical stimulation through the use of massage and PROM techniques is another crucial element to the healing process for canine patients with some injuries, post-operatively, neurological disease, or ageing disease such as arthritis (Figures 5 and 6). PROM is the movement of a joint by external forces. Massage and PROM provide physical motion to joints and muscles stimulating them, easing tension, and increasing muscle flexibility — the affected joint is flexed and extended in a controlled fashion repeatedly.


Massage provides relief to the patient in several ways. Massage aids in the removal of noxious chemicals, releases endogenous endorphins, improves oxygen supply to the tissues, and increases venous and lymphatic return. It also improves proprioceptive awareness, prepares muscles for exercise, reduces muscle fatigue, and reduces tension and anxiety in the patient (Lindley and Watson, 2010). Not all patients will be receptive to this treatment. Some patients will be too nervous or reactive to physical touch.
There are many techniques for massage therapy in canine patients. Each technique provides a different role in the patient's healing process. These techniques can be learned through seminars or by training under a licensed professional.
This technique is used at the author's practice mainly in aiding movement of joints that otherwise can be strained by the patient moving them on their own. This technique is also used on patients with neurological diseases to provide stimulation to the nerves and help the patient feel their affected body parts.
PROM should be carried out with care to ensure that it does not exacerbate the pain in the affected limb or provide discomfort to the patient. It is advisable to warm the muscles before starting this therapy.
Ultrasound technology
Therapeutic ultrasound uses sound frequencies which absorb energy in the body and convert it into kinetic energy (Figure 7). This therapy can decrease pain and inflammation and increase blood flow, metabolic rate, and collagen extensibility (Fox and Millis, 2010).
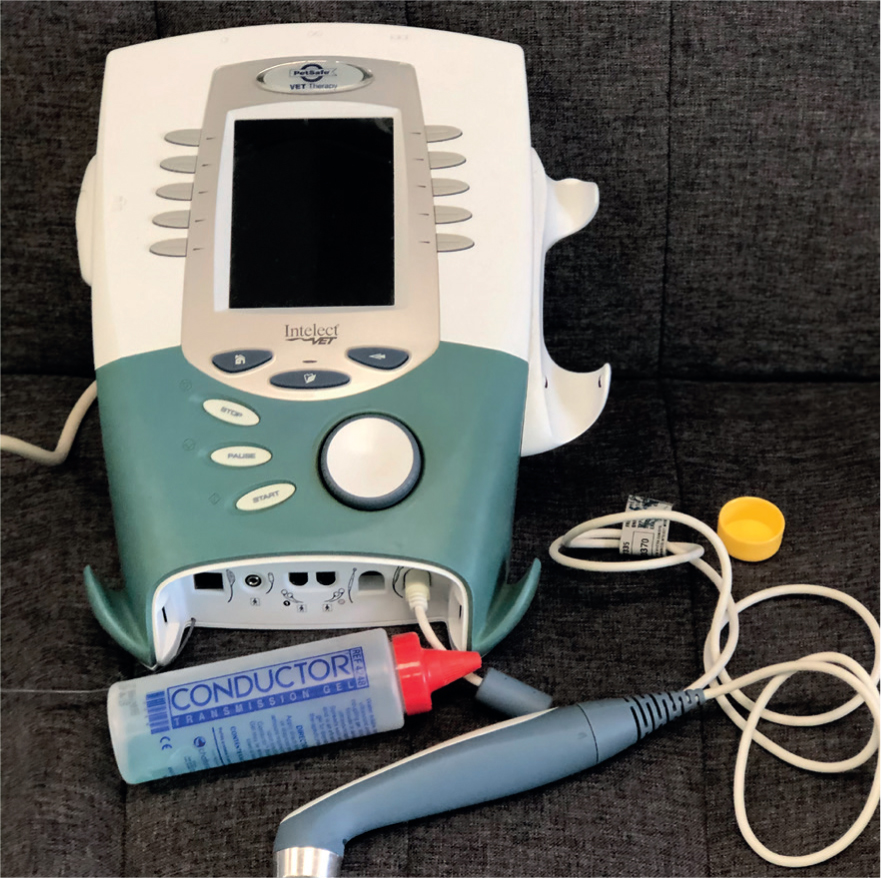
Ultrasound therapy increases local blood circulation and tissue oxygenation which promotes healing by delivering nutrients. It is useful for improving extensibility of connective tissue, which facilitates stretching (Fox and Millis, 2010). This helps with several conditions including arthritis, tendon injuries, neurological diseases, and muscular injuries (Figure 8).

Ultrasound therapy can be delivered in two modes. The continuous mode refers to a constant flow of energy delivered to the tissue. The pulsed mode has regular breaks of energy in between pulses. Different conditions require different modes, depending on the intensity and longevity of the treatment sessions needed for the patient.
Neuromuscular electrical stimulation and transcutaneous electrical nerve stimulation units
There are two modes used most commonly in canine rehabilitation: neuromuscular electrical stimulation (NMES) and transcutaneous electrical nerve stimulation (TENS) (Figure 9).
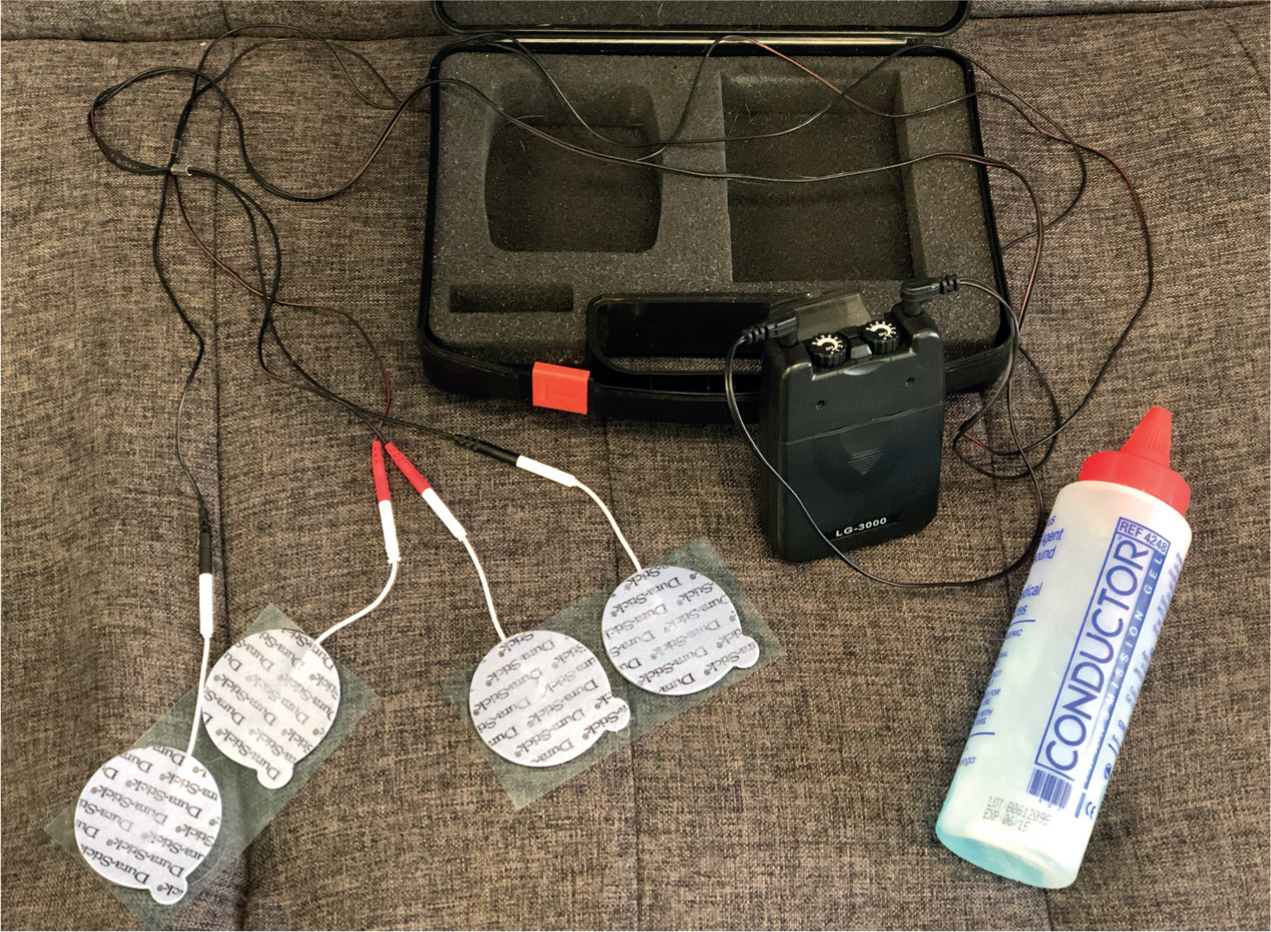
NMES units are used mostly on neurological and orthopaedic patients. NMES is used to provide muscle contraction, by recruiting type II (fast twitch) fibres (Levine and Millis, 2014). This reduces pain by contracting and relaxing the muscles, and stimulates the nerves triggering the brain to respond to them. As NMES stimulates these nerves, it is also stimulating the muscles to contract and relax as the NMES is pulsed (Figure 10). This helps to develop and maintain the muscles of the affected area (Fox and Millis, 2010). Some common conditions that can benefit from NMES are: cruciate repairs, meniscal debridement or repair, spinal cord injuries, or paresis (Levine and Millis, 2014).
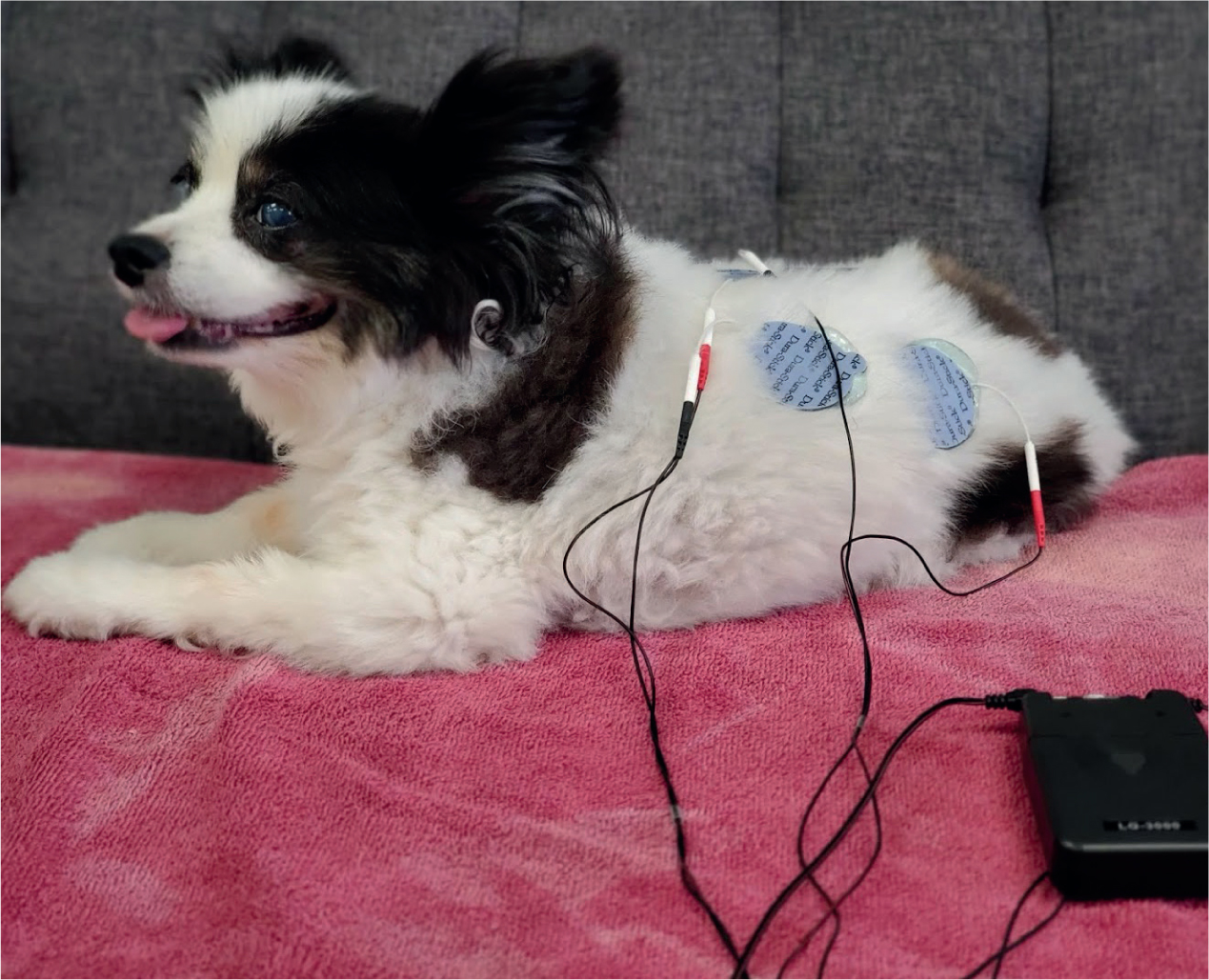
TENS units are used for relieving many types of pain in patients. The TENS units work by sending electrical pulses which flood the patient's nervous system, reducing or blocking transmission of pain signals to the brain. TENS stimulates blood flow to the affected area, which speeds the healing process and relieves inflammation. This is typically given in a continuous flow for a set amount of time during each rehabilitation session. It also increases muscle flexibility and relieves spasticity. This can be used on orthopaedic, neurologic, and tendon injuries/diseases. (Van Dyke and Zink, 2018)
Conclusion
Pain management in canine patients is crucial. There are many ways to provide pain relief and body healing in veterinary patients. Laser, tPEMF technology, massage/PROM, acupuncture, ultrasound therapy, and NEMS and TENS all provide pain relief in different ways aiding the body in self-healing. All of these therapies can be learned and practiced by veterinary nurses under the guidance of their veterinarians. There are many resources to provide training in these therapies for any veterinary team.
KEY POINTS
- There are several other modes of pain relief besides traditional medications.
- Pain therapies such as laser, targeted pulsed electromagnetic field therapy, ultrasound, acupuncture, and massage/passive range of motion, neuromuscular electrical stimulation and transcutaneous electrical nerve stimulation provide unique pain relief.
- Pain therapy techniques provided by the veterinary nursing team under the supervision of the veterinarian aid in faster recovery of patients.
- Alternative pain therapies are beneficial to many patients from chronic illnesses to post-surgical procedures.


