Multimodal analgesia should be incorporated into any surgical procedure; this article will discuss the use of thoracic limb and pelvic limb locoregional blocks as part of a multimodal analgesic approach to pain management in the canine and feline surgical patient.
Locoregional blocks use local anaesthetic agents to attempt to totally block transmission of any pain sensation from the neurons stimulated during nociception. Local anaesthetics work on blocking any impulse in myelinated and unmyelinated nerve fibres by inhibiting voltage-gated sodium channels, and are therefore the most effective way to prevent sensation of the central nervous system.
According to randomised controlled studies in humans, using locoregional anaesthesia in conjunction with a general anaesthetic, helps decrease postoperative recovery times, reduce the length of hospital stays, and provides superior pain relief in patients when compared with the use of systemic opioids (Singelyn et al, 1998; Capdevila et al, 1999). Campoy (2008) mentioned that the key features of regional anaesthesia combined with less invasive surgical techniques can encourage early appetite and increased mobility, decreasing severity of complications, and hence decreasing the length of hospital stays, overall making the patient more comfortable. Therefore, locoregional anaesthesia techniques should be considered in the anaesthetic planning for veterinary patients undergoing surgery.
There are different techniques that can be used for locoregional blocks. The success of the block will depend on the technique used, the drug dose administered, and experience of the person performing the block. Complications that may arise from using specific techniques and different blocks should also be considered when choosing the correct block for any given patient.
Locoregional anaesthesia can be administered using three different techniques. These include: blind (without the use of electrostimulation or ultrasound), ultrasound guided, or electrostimulation (with the use of a nerve stimulator). Studies have been conducted on the success of different techniques and both the ultrasound guided (Campoy et al, 2010) and electrostimulation (Campoy et al, 2008) have demonstrated improved accuracy and success in providing adequate distribution of local anaesthetic for brachial plexus, femoral and sciatic nerve blocks.
Ultrasound-guided techniques for locoregional blocks are becoming increasingly popular in humans (Marhofer and Chan, 2007). These techniques use sonographic visualisation of the injecting needle and its proximity to anatomical landmarks, including the nerves themselves rather than seeing the functional end point to stimulation (muscular twitches after electrical impulse), which is used with electrostimulation technique.
The use of electrostimulation or ultra-sound guided techniques allows for more accurate needle location without eliciting paraesthesia than can been seen when local anaesthetic epidurals are administered (Greenblatt, 1962). Directing the anaesthetic agent closer to the nerve (without being in the nerve) allows the dose and volume of the drug to be reduced, therefore reducing side effects of the drugs, without affecting the quality of anaesthesia provided.
Complications related to locoregional anaesthesia include: trauma to the nerve, tissues or blood vessels associated with the nerve; injection directly into the nerve (including neuronal ischaemia); incorrect drug or drug calculations and infection, but with appropriate training and experience, the likelihood of these complications occurring is reduced. Hence it is imperative that the correct training and guidance is provided for practitioners before performing them on patients.
This article describes the use of a nerve stimulator for femoral, sciatic, brachial plexus, and radial, ulnar, median and musculocutaneous (RUMM) blocks.
Drugs and drug doses
Table 1 shows the different local anaesthetic drugs and the doses that can be used in locoregional blocks. A combination of these local anaesthetics and an opioid, can be used to form part of a multimodal approach to the patients' pain management plan.
Table 1. Local anaesthetic drug doses used in different locoregional blocks
| Local anaesthetic | Onset time | Duration | Common clinical dose | Maximum dose |
|---|---|---|---|---|
| Lidocaine | 5–15 minutes | 1–2 hours | 4 mg/kg | Dogs: 10 mg/kgCats: 5 mg/kg |
| Bupivacaine | 15–30 minutes | 4–6 hours | 1 mg/kg | Dogs: 3 mg/kgCats: 2 mg/kg |
| Mepivacaine | 5–15 minutes | 1.5–3 hours | 4 mg/kg | Dogs: 10 mg/kgCats: 5 mg/kg |
Electrostimulation technique
The first demonstration of electrical nerve stimulation was performed as early as 1780 in frogs, however it was Greenblatt (1962) who introduced use of nerve stimulation for improving regional blocks into clinical practice in humans. It is now widely used in many general and speciality veterinary practices.
After clipping and aseptically preparing the proposed insertion sites, the technique of electrostimulation uses a 30° bevel stimulating insulated needle, which connects to a nerve stimulator (Figure 1). Starting with an output of 1 mA, a frequency of 2 Hz and pulse duration of 0.15 ms (Campoy, 2008), the needle is inserted at the desired location, looking for a nerve response (muscular twitch of the effector muscles distal to the stimulated nerve) — once the desired nerve response is noted, the stimulation amplitude is incrementally reduced down to 0.4 mA. If a nerve response is still seen at this low amplitude, it indicates the needle tip is close to the nerve. If a decrease of the amplitude to 0.2 mA results in persistent muscle twitch, this might indicate the needle is within the nerve (Hadzic and Vloka 2004). If this occurs, withdraw the needle slightly until no stimulation is seen. Draw back to ensure there is no blood aspirated, inject quarter to half of the calculated dose of local anaesthetic solution and increase the nerve stimulator to 0.4 mA — no response should be seen (Raj Test)(Campoy, 2008). Following this, continue to inject the remainder of the local anaesthetic solution; no resistance should be felt during the injection at any point.

This technique is used for all the locoregional blocks described below, remembering all the key points:
- Clip and aseptically prepare the skin of the proposed needle insertion site
- Wait for the response of the correct nerve before injecting any solution
- If a response is still seen at 0.2 mA, remove the needle slightly as the needle is probably in the nerve
- Do not inject if resistance is felt, and
- Draw back before injecting any solution to ensure blood is not aspirated.
Femoral and sciatic blocks are generally used in conjunction with each other to provide anaesthesia unilaterally to the pelvic limb of interest. These local blocks can be used instead of administering an epidural, which also blocks the contralateral limb unnecessarily and potentially has more side effects than using the femoral/sciatic blocks (Campoy, 2012) yet has not been shown to provide any different analgesia than the use of epidurals (McCally et al, 2015).
Femoral block
The femoral nerve is supplied by the L4–L6 nerve roots. Anaesthesia of this nerve will block the femur, femoro-tibial joint, medial femoro-tibial joint capsule, femoro-tibial intra-articular structures, skin of the dorsomedial tarsus and the first digit.
Procedure
The patient is positioned in lateral recumbency with the affected leg uppermost. The pelvic limb is abducted approximately 90° and extended caudally. Palpate the femoral artery and picture a triangle made up of the pectineus muscle (caudally), sartorius muscle (cranially) and rectus femoris (medially) and iliopsoas muscle (proximally). Insert the needle between the femoral artery and the sartorius muscle. Advance the needle on a 20–30° angle proximally towards the iliopsoas muscle. The femoral nerve is located immediately medially of the sartorius and approximately 1 cm deep in medium size dogs (Figure 2).
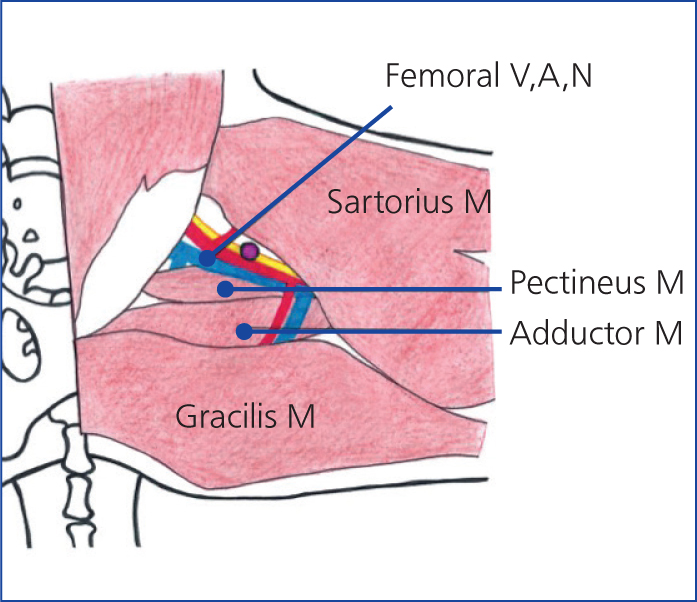
A twitch of the quadriceps and movement of the stifle is seen when the femoral nerve is stimulated. As this nerve is close to the femoral artery, inadvertently the vessel can be punctured causing haemorrhage. If this does occur, remove the needle, and apply digital pressure for up to 5 minutes to stop the bleeding.
Sciatic block
The sciatic nerve stems from the L6–S2 vertebrae blocking areas of the caudolateral joint capsule and lateral meniscus and the majority of the limb distal to this. Using this block in conjunction with the femoral nerve block, will desensitise the entire unilateral limb.
Procedure
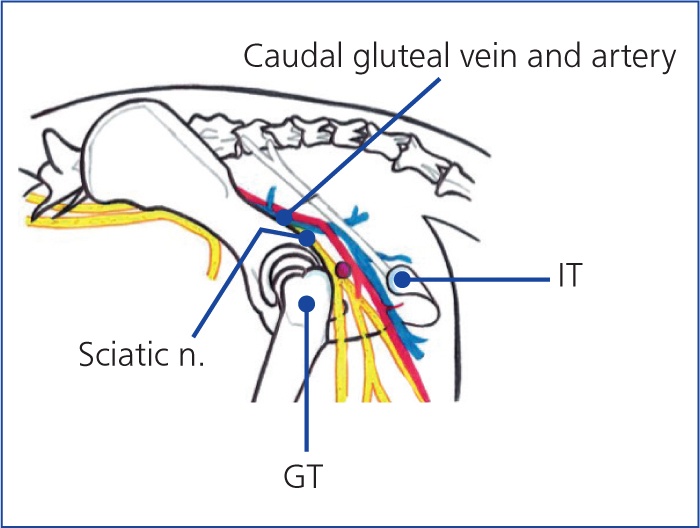
Position the patient in lateral recumbency with the leg to be blocked upmost. Palpate the greater trochanter of the femur and ischiatic tuberosity and about one third of the distance from the greater trochanter (to the tuberosity), insert the needle at a 90° angle to the skin (Figure 3). Visualisation of dorsal or plantar flexion of the hock (either is acceptable) suggests correct location for the stimulation needle electrode and sciatic nerve block can be performed.
Brachial plexus block
The brachial plexus is formed by the ventral branches of the caudal cervical and first thoracic nerves (C6–T2). Performing this locoregional block successfully will desensitise the limb unilaterally, from the elbow and further distally. The specific nerves that are blocked include pectoral, suprascapular, subscapular, axillary, musculocutaneous, radial, median and ulnar nerves. If you wish to target more proximally than the elbow a paravertebral brachial plexus block would need to be performed (this article does not explain this block, because of the potential risks associated with this more difficult technique (Monticelli et al, 2018)).
Procedure
The patient is placed in lateral recumbency with the limb to be blocked uppermost. Palpate the acromion — the needle is inserted cranial to the acromion and medial to the subscapularis muscle in a caudal direction. The needle is directed towards the first rib with a slight dorsal deviation relative to the body axis (Figure 4). When advancing the needle be careful not to penetrate through the jugular vein, axillary artery, axillary vein or subscapular vein which are also in this location. If you do advance the needle through one of these, a haematoma will form, remove the needle and apply steady pressure for up to 5 minutes.
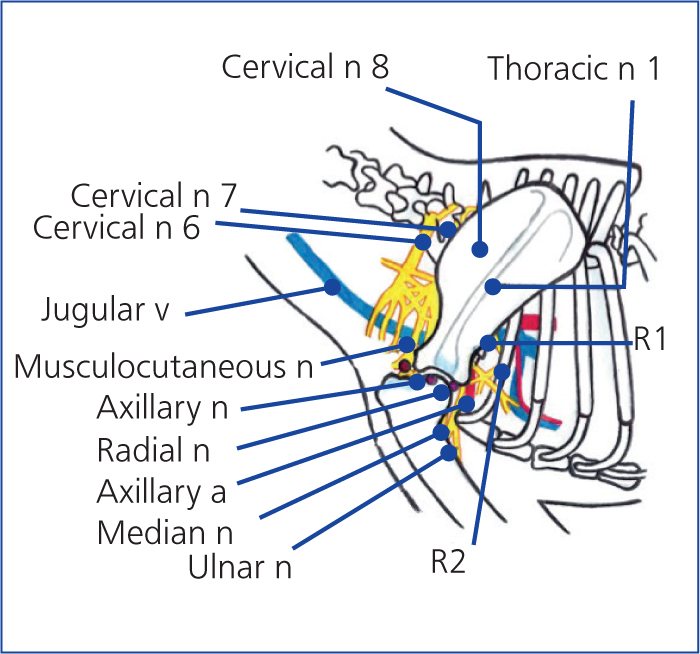
The suprascapular nerve is reached when there is flexion and extension of the shoulder; the subscapular nerve is reached when the shoulder extends and adducts; the musculocutaneous nerve is reached when contractions of the biceps brachii muscle and flexion of the elbow is seen; extension of the elbow is seen when the radial nerve is reached, carpal flexion is seen with the ulnar nerve and the median nerve is reached when the carpus flexes.
Radial, ulnar, median and musculocutaneous block
The RUMM block is used for providing anaesthesia for procedures involving the antebrachium, carpus and manus (paw of the thoracic limb).
Procedure
Position the patient in lateral recumbency with the affected limb uppermost. To block the radial nerve, advance the needle from the lateral aspect of the limb, between the long head of the triceps and the brachialis muscle, proximal to the lateral epicondyle of the humerus (the nerve is very superficial) (Figure 5a). When using the electrostimulation, you will note a response of extension of the carpus.
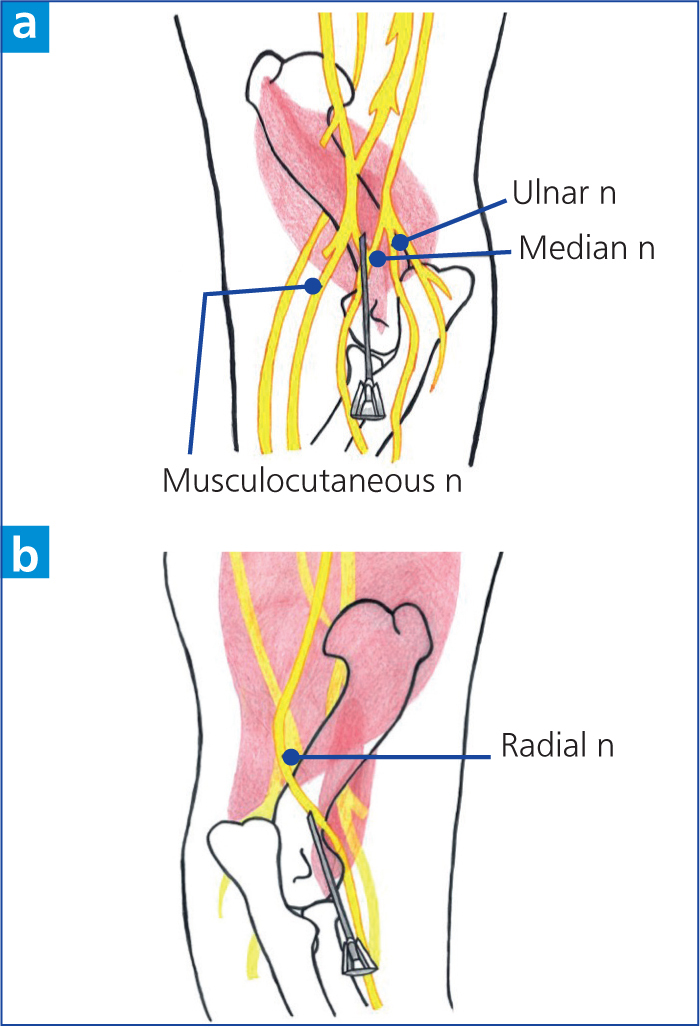
To block the median and ulnar nerves, on the medial aspect of the limb, feel for the brachial artery, insert the needle caudal to the artery proximal to the elbow joint between the biceps and the medial head of the triceps (Figure 5b). When using electrostimulation, you will note flexion and pronation of the antebrachium for the median nerve, and/or flexion of the forepaw may be seen which is stimulation of the ulnar nerve. Local anaesthetic deposited here will block both the median and ulnar nerves.
Conclusion
There are many locoregional blocks that can be performed on small animals (this article only addresses a few of them) and it is the technique, the confidence/experience of the person performing the block and the equipment required that will determine how often locoregional blocks will be used in practice. However, it is important to recognise that any local block that is used successfully in patients, as part of a multimodal analgesia/anaesthesia approach, should benefit the patient in the peri-operative and postoperative periods. VN
KEY POINTS
- Multimodal analgesia techniques should be used in any surgical patient.
- Successful local anaesthetic blocks will block any sensation of nociception when that nerve is blocked.
- Locoregional blocks decrease postoperative recovery times, reduce length of hospital stays and provides


