Burn injuries are infrequently seen in small animal practice and can represent a challenge to nurse and treat. Burns can be sustained from heat, cold, chemical, electrical, and radiation sources. A thermal burn is defined as skin damage through contact exposure to extremes of temperature from a liquid, solid, or gaseous heat source. This includes excessively hot and cold temperatures. In practice, thermal burns are most commonly encountered because of injury from open flames, hot liquids and inappropriate use of heat pads (Jenkins, 2018).
Direct thermal damage causes immediate cell death, evident in the central portion of the burn wound (Vaughn and Beckel, 2012). Surrounding this portion is a zone of ischaemia, which can be preserved if managed appropriately. Finally, the outermost zone is characterised by vasodilation and an increased blood supply and inflammatory response (Jeschke et al, 2020). Burns are classified according to the depth of tissue injury (Table 1, Figures 1–3).
Table 1. Classification of burns by tissue injury
| Burn classification | Skin layers involved | Clinical characteristics |
|---|---|---|
| Superficial (or epidermal) | Epidermis only | Dry, erythematous, blanches with pressure, painful |
| Superficial partial-thickness | Epidermis and superficial dermis | Exudative, erythematous, blistering, blanches with pressure, painful |
| Deep partial-thickness | Epidermis and deep dermis | Red, leathery, non-blanching, minimally painful |
| Full-thickness | Epidermis, dermis, subcutaneous tissue | Variable: white to leathery to charred black. Non-painful |



The total body surface area (TBSA) affected by thermal burns can be estimated using the ‘rule of nines’ where the head and each thoracic limb each represent 9% of TBSA, and the dorsal trunk, ventral trunk and each pelvic limb each represent 18% of TBSA (Scott et al, 2001). Burns involving less than 20% of TBSA are local burns; those involving more than 20% of TBSA are severe burns, which may lead to systemic derangements (Vaughn and Beckel, 2012).
These figures originate from human medicine and animals have greater skin elasticity than humans. Use of these figures in veterinary patients may overestimate the total area affected, and should serve as a rough guide only.
Emergency treatment and first aid
Local burns are unlikely to lead to systemic derangements and aggressive therapy is not typically required. When the injury is directly witnessed, cold water can be applied to cool the wound. This prevents further tissue damage and provides analgesia (Cuttle et al, 2008).
Cooling the wound with cold tap water at between 2°C and 15°C for 20 minutes is recommended over using iced water (Yuan et al, 2007) that causes vasoconstriction and can potentially damage tissue further. A sterile, occlusive, non-adherent dressing can be applied to prevent further trauma and limit ongoing contamination (Jenkins, 2018).
Severe burns can lead to cardiovascular dysfunction because they deplete intravascular volume, reduce cardiac output, and increase systemic vascular resistance (Keck et al, 2009). This phenomenon is also known as burn shock. Burn patients involved in household fires may also have airway dysfunction caused by smoke inhalation, which manifests in bronchospasm, acute airway obstruction, pneumonitis, pneumonia and respiratory failure (Warden, 1992). Clinically, the effects can be delayed and ongoing changes can still be encountered 3–5 days after the event (Mlcak et al, 2007).
Carbon monoxide and cyanide toxicity from fires can also be encountered in burn patients (Fitzgerald and Flood, 2006). Treatment of systemic abnormalities should be prioritised over the burn(s).
A discussion of the resuscitation of the burn patient is beyond the scope of this article; further information can be found elsewhere (Vaughn and Beckel, 2012).
Managing burn wounds
The principles of wound management are relevant in the treatment of the burn patient: infection control, managing contamination, wound debridement and preventing further damage (Williams and Moores, 2009).
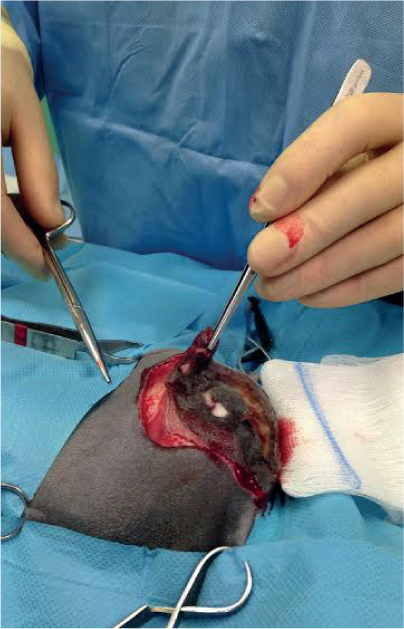
If the burn was witnessed and the patient is promptly presented to the veterinary surgeon, burn wounds should initially be cleaned with a 1:40 dilute solution of chlorhexidine or a 1:9 dilute solution of povidone iodine (Pavletic and Trout, 2006). Heavily contaminated wounds may benefit from wound lavage under general anaesthesia. Lavage under general anaesthesia is favoured over the use of heavy sedation, and allows for close examination of the wound at the same time (Williams and Moores, 2009). As lavage solutions, tap water and sterile isotonic saline have been shown to be equivalent (Huang et al, 2013). Lavage solutions containing polyhexamethylene biguanide (PHMB) have been shown to be effective against biofilms and can be considered if significant contamination is present (Davis et al, 2017). In the case of unwitnessed burns or delayed presentations, cleaning and lavage may be employed for initial surface decontamination followed by eschar removal (Figures 4 and 5).
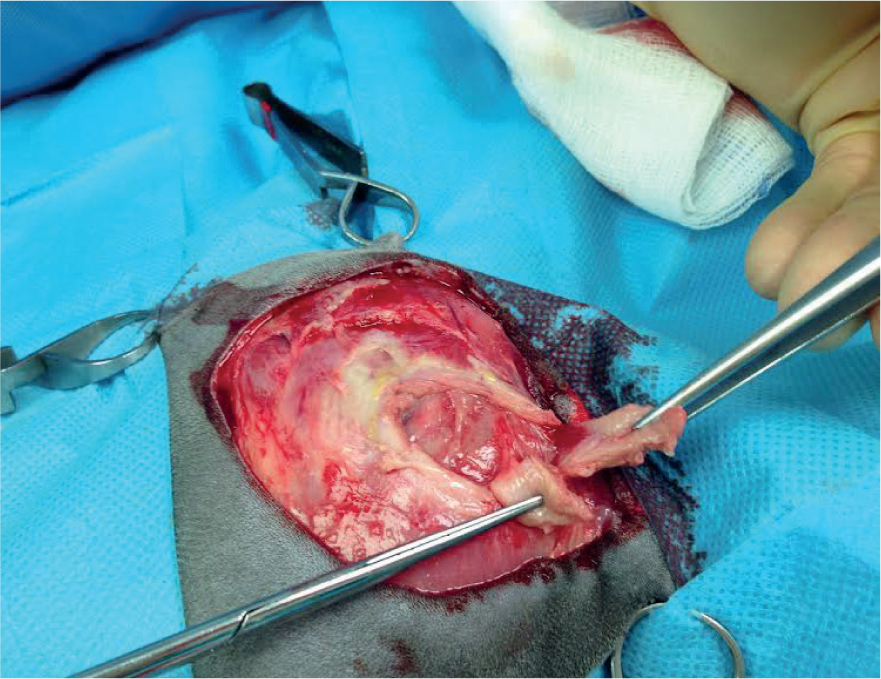
After lavage, the wound is debrided to remove necrotic and devitalised tissue. Debridement technique is dictated by the type of burn wound being treated.
Autolytic debridement, where the body engages white blood cells to remove dead tissue, can be used to conservatively manage superficial burn wounds (Campbell, 2015). A moist wound environment should be maintained to promote autolysis and wound healing. Surgical debridement may be used in superficial partial-thickness burn wounds, which are then allowed to heal by secondary intention (De-Santi, 2005). Strict aseptic technique should be adhered to as the surgeon removes all visible evidence of devitalised tissue. As much questionable tissue as possible should be removed, but anatomically important structures spared. Enough tissue must be preserved to allow further wound closure, if planned. In comparison to autolytic debridement, which is selective at the microscopic level (removing only unhealthy tissue), surgical debridement is selective only at the macroscopic level (chosen by the surgeon based on visible characteristics) (Campbell, 2015).
Mechanical debridement using wet-to-dry dressings is the least selective form of debridement and should thus be considered only if the autolytic and surgical debridement are not possible (Bell, 2018). Monofilament fibre debridement pads are relatively new products developed as a gentle alternative to traditional dressings. Efficacy has been demonstrated ex vivo and in uncontrolled trials (Schultz et al, 2018; Roes et al, 2019). Further evaluation of debridement pads for wounds in general and thermal burns in particular would be useful.
Following debridement, superficial and superficial partial-thickness burn wounds may be allowed to heal via secondary intention, which usually proceeds uneventfully in the presence of a clean, moist wound environment (Vaughn and Beckel, 2012). Provided that the surface area of the burn wound is small, wound contracture and loss of mobility are not expected complications with this technique. Deep partial-thickness and full thickness wounds, in addition to wounds with a large surface area, would benefit from surgical closure or skin grafting (primary intention wound healing).
Surgical closure should be performed as early as the patient's condition allows (Silver et al, 2007). For small wounds, tension-relieving techniques are usually sufficient to achieve primary closure (Williams and Moores, 2009). For mediumsized wounds, skin-fold advancement flaps and axial pattern flaps are applicable as long as the surgeon is familiar with their use (Remedios et al, 1991; Hunt et al, 2001).
Skin grafting should be considered in large, deep burn wounds where surgical closure is inappropriate. Care must be taken to remove all devitalised tissue, otherwise failure of the skin graft is likely. Capillary bleeding is an indicator of a viable wound bed and can be used to guide debridement (Orgill, 2009). Full-thickness skin grafts are preferred over split-thickness grafts. A detailed description of the technique can be found elsewhere (Williams and Moores, 2009).
Early excision and grafting of large burn wounds within 7 days of injury is now the standard of care in human medicine, and has consistently been shown to have better outcomes than delayed grafting 1–4 weeks after injury (Ong et al, 2006). Studies in companion animals are lacking, but it is reasonable to apply these human medical principles in small animal patients, which could lead to a reduction in duration of hospitalisation, patient morbidity and overall healthcare costs.
Infection control
Gross contamination is best controlled by lavage and debridement, as described earlier. Afterwards, ongoing infection control of the wound bed can be best achieved by the use of topical antimicrobials (Honari, 2004). Systemic antimicrobials have shown no benefit over topical therapy in preventing infection (Sheridan et al, 2001). Inappropriate use of systemic antimicrobials contributes to antimicrobial resistance; however, their use can be considered in patients with extensive burns and severe systemic compromise (Ramos et al, 2017).
Silver sulphadiazine has been recommended both prophylactically and therapeutically, in the management of burn wounds, in both veterinary and human medicine (Vaughn and Beckel, 2012). Silver sulphadiazine has multiple mechanisms of action against bacteria and thus has broad-spectrum antimicrobial activity (Dai et al, 2010). Silver sulphadiazine is widely employed in the management of burn wounds; however, recent evidence has emerged suggesting that silver sulphadiazine has a deleterious effect on wound healing, and is more suited to therapeutic treatment of an active infection instead of for prophylaxis (Khansa et al, 2019). Other topical agents such as medical-grade honey have broad-spectrum antimicrobial activity and also promote a moist environment for wound healing (Langemo et al, 2009). Maceration of periwound skin can be a complication in exudative wounds managed with honey. In patient's with larger wounds, fluid status must be monitored and losses via the wound replaced. Recently, antiseptic-impregnated dressings containing dialkylcarbamoyl chloride or PHMB have been shown to be useful in infection control (Totty et al, 2017; Worsley et al, 2019) and their use can be considered.
Complications of wound healing
In general, wound healing complications can arise through a combination of factors relating to the wound, the surgeon, and the patient (Williams and Moores, 2009). Infection, burn scar contracture, and graft failure are the most common complications encountered in thermal burns.
Animals with burns are predisposed to both local and systemic infection related to the loss of the skin barrier and the systemic inflammatory state (Vaughn and Beckel, 2012). Measures to prevent wound and systemic infections have been described earlier in the article. Wound infections can be suspected on clinical examination of the wound. However, a surface swab or tissue biopsy is necessary to confirm it microbiologically (Low and Aldridge, 2022). The most narrow-spectrum drug is recommended for the shortest duration of time possible, dictated by the animal's clinical progress (Allerton, 2018).
Burn scar contracture refers to the loss of function of an anatomical body part occurring secondarily to the wound healing process (Figure 6). This is most commonly encountered with secondary intention healing over a joint or an anatomical orifice such as the prepuce, vulva, ear or eye (Williams and Moores, 2009). Surgical resection of the contracture is required, replacing it with a skin flap or a skin graft. To prevent burn scar contracture arising, judicious planning before surgery is advised.

In deep partial-thickness or full-thickness burns, where excision and grafting have been used, the skin graft is subject to failure for various reasons. Meticulous surgical technique and familiarity with the procedure can minimise complications relating to excess fluid accumulation, graft movement, and wound bed contamination (Riggs et al, 2015). The animal's temperament, and meticulous care of the skin graft are also key to ensuring success (Pavletic, 2018).
Nutrition
The animal with a burn is in a hypermetabolic state which can be seen as soon as 3 days after injury, and can persist for months (Jeschke et al, 2006). Increased protein catabolism, gluconeogenesis, glycogenolysis, lipolysis, hepatic insulin resistance, glucose consumption, oxygen consumption and loss of lean body mass contribute to the complex dysmetabolism seen in the burn patient (Williams and Moores, 2009). Early enteral nutrition is recommended within 24–48 hours after the injury (Pavletic and Trout, 2006), once the patient is cardiovascularly stable. Enteral nutrition is more physiologic, less technically challenging and safer than parenteral nutrition. It is generally preferred over parenteral nutrition in most cases (Prittie and Barton, 2004), and specifically in the animals with burns (Chen et al, 2007). Enteral nutrition can be delivered via a variety of feeding tubes. The choice of feeding tube is based on various patient factors (Silverstein and Hopper, 2015). Previously, ‘illness factors’ were used in critical patients to account for their hypermetabolic state and increased calorific requirements. This is no longer recommended and the goal should be to deliver the animal's resting energy requirement, as soon as they will tolerate it (Chan, 2004). The reader is referred to other texts for a more in-depth discussion of nutrition in critically-ill patients (Silverstein and Hopper, 2015).
Analgesia
Thermal burn wounds cause both acute and chronic pain. Background wound pain is experienced at a low level at rest throughout the day. Acute pain is experienced, on top of background pain, during medical procedures such as dressing and bandage changes (Summer et al, 2007). Break-through pain is also evident when the patient moves, or is moved, after long periods of inactivity (Richardson and Mustard, 2009).
Multimodal analgesia is the best approach to manage pain associated with thermal burn wounds. A full μ-opioid should be administered at first presentation of an acute burn (Vaughn and Beckel, 2012). Procedural pain is expected during debridement and dressing changes, and escalating the analgesia is indicated. Multimodal analgesia can be incorporated into the sedation or anaesthetic protocol, through the use of α-2 adrenergic agonists, benzodiazepines and ketamine (Epstein et al, 2015). Topical local anaesthetics such as a lidocaine-prilocaine cream have been shown, in conjunction with an opioid, to be effective in controlling pain (Lillieborg and Aanderud, 2017), and did not have a negative effect on wound healing (Pedersen et al, 1996). In the outpatient setting, oral non-steroidal anti-inflammatory drugs (NSAIDs) with or without paracetamol may be considered (Epstein et al, 2015). The use of an NSAID in the acute, systemically compromised animal is contraindicated.
The assessment of pain can be subjective, and intra- and inter-observer variation exists. The use of objective pain scores is recommended in burns patients, to guide the analgesic plan (Holton et al, 2001).
Negative pressure wound therapy
Negative-pressure wound therapy (NPWT) is the use of an active, closed wound management system that applies sub-atmospheric pressure to the wound bed and promotes wound healing. Indications include, but are not limited to, thermal burn wounds, de-gloving in-juries, traumatic wounds, infected wounds, dehisced wounds, free skin grafts, and chronic non-healing wounds (O'Dwyer and Aldridge, 2014). NPWT is applied after appropriate debridement of the wound, and is most effective in the proliferative phase of healing (Krug, 2011). NPWT promotes wound healing through multiple mechanisms including promotion of blood supply, maintenance of a moist wound environment, encouragement of granulation tissue formation, efflux of infectious material and exudate, and direct physical protection of the wound bed (Bell, 2016). NPWT is applied to the wound for an average of 3 days in one study (Pitt and Stanley, 2014), followed by surgical closure or secondary intention healing. Proprietary human medical- and veterinary-specific devices exist for this purpose and the reader is referred elsewhere for practical details on the application of NPWT (Stanley et al, 2013).
Conclusions
Thermal burns result in both local damage and systemic effects and a multidisciplinary approach to patient management must be employed. In systemically compromised animals, management of major body system abnormalities takes priority over surgical management of the thermal burn. General principles of wound management are relevant to the burn patient. The surgical approach to the burn will vary depending on individual wound factors and patient factors. Adjunctive therapies, such as NPWT, have a role in managing thermal burns. Further research into thermal burns in veterinary species is warranted.
KEY POINTS
- In severe thermal burns, treating systemic abnormalities is prioritised over dealing with the injuries.
- Heavily contaminated wounds may benefit from wound lavage under general anaesthesia, which is favoured over the use of heavy sedation and allows for close examination of the wound at the same time.
- Debridement technique is dictated by the individual wound factors.
- Surgical closure should be performed as early as the patient's condition allows.
- Infection is controlled through lavage, debridement and choice of dressings.
- Infection, burn scar contracture and graft failiure are the most common complications of thermal burn wounds.
- Early enteral nutrition is recommended over parenteral nutrition.
- Pain can be acute and chronic and should be assessed and managed accordingly.


