Evidence-based practice is a developing concept in veterinary nursing and is considered fundamental to improving veterinary nurses’ approach to patient care (Banks, 2010). Models of nursing and care planning has steadily filtered into veterinary nursing literature and a rising number of veterinary nurses are reflecting and evaluating their current practice and publishing their findings (Lock, 2011; Wager, 2011; Brown, 2012; Heayns, 2012). Learning about and implementing holistic veterinary nursing care is no longer a new concept for veterinary nurses with articles relating to aspects of delivery of holistic nursing appearing with increasing frequency since 2000 (Welsh and Wager, 2013). Terms such as holistic nursing, nursing process and care planning are now widely recognised by veterinary nurses although Welsh and Wager (2013) also question whether practices and systems associated with care plans per se, are actually being implemented in clinical practice.
Historically, a number of authors suggest that veterinary nursing had originally followed a medical approach, which put emphasis on the physiological reasons for illness and created a disease-orientated approach to care (Jeffery, 2006; Pullen, 2006). This approach, seen as problematic in human nursing, has also received criticism from veterinary nurses (Pullen, 2006; Welsh and Orpet, 2011) with alternative approaches now being evaluated in veterinary nursing (Wager, 2011; Lock, 2011; Brown, 2012).
As a result, models of nursing used for the basis of patient care planning have steadily filtered into veterinary nursing theory. With the aid of higher education courses, a rising number of veterinary nurses are able to reflect and evaluate their current practice, enabling them to develop their nursing techniques and publish their findings (Wager, 2011; Lock, 2011; Brown, 2012). The current suggestion is that the introduction of models of nursing and holistic care concepts is enabling veterinary nurses to develop their skills and advance their professional role (Wager and Welsh, 2013). Nursing models, and more specifically, nursing care plans (NCPs), can be used as a framework to structure detailed and specific nursing care to be carried out when a patient is admitted and hospitalised (Orpet, 2011).
This article reflects on how the design and implementation of a NCP, using Orpet and Jeffery's Ability Model, affected the author, her colleagues and her patient.
Designing the NCP
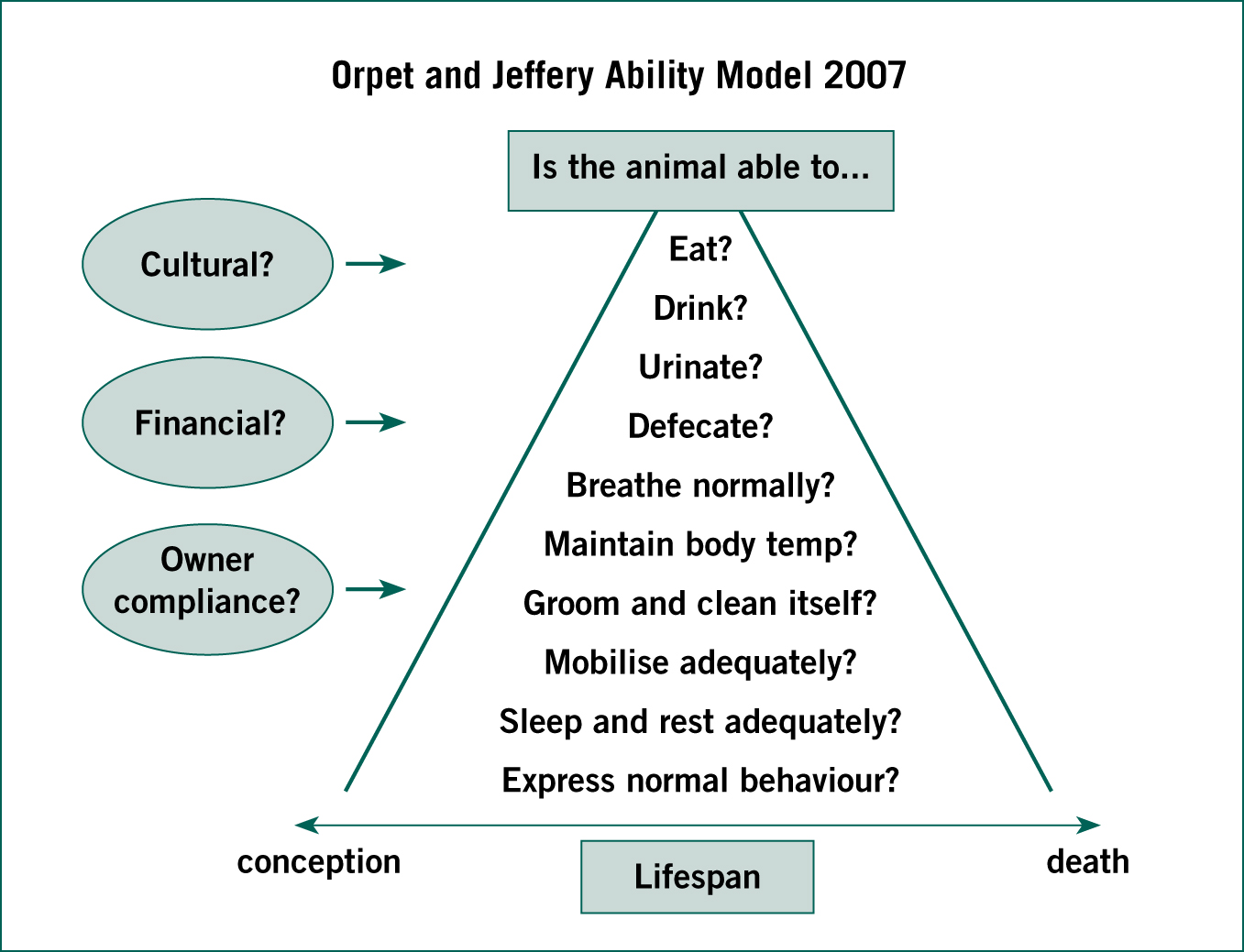
As described by Can and Erol (2012) NCPs provide an organised framework for the knowledge, thoughts and actions that nurses bring into patient care. Their structure is based on a model of nursing care that is followed (Mason, 1999). In this instance, the primary author selected and adapted the Orpet and Jeffery Ability Model (OJAM) (Orpet and Welsh, 2011)) (Figure 1) as the basis for the design of the care plan and for structure of the different stages leading to the care plan document. This model's primary goals of understanding the patient's individual needs, addressing potential problems and taking measured, appropriate action (Welsh and Wager, 2013) were aligned to the author's objectives when using an NCP. During the design process three stages were created which incorporated the OJAM: a client interview; patient assessment; and care planning. These three stages also broadly incorporated the five continuous phases associated with the human nursing process as described by Murry and Atkinson (1994): assessment; nursing diagnosis; planning; implementation and evaluation.
The NCP was created for a 3-year-old German Shepherd dog named Jess. Jess was admitted to the hospital following a period of anorexia and intermittent vomiting. The veterinary surgeon (VS) noted pain on abdominal palpation and signs of dehydration on clinical examination. Jess was admitted for stabilisation and diagnostic investigation to establish whether a gastrointestinal foreign body was present.
Client interview
The first stage of creating the NCP was to carry out an interview with the client. This initial assessment stage can be an important time to gain input from the owner which allows the veterinary nurse (VN) to understand the normal routines of the patient enabling specific care considerations to be made (Main, 2011a). Research by Lue et al (2008) and the findings of Lock (2011) suggest that communication plays a key role in creating a strong relationship between the client and the veterinary professional, which ultimately can impact positively on the care a veterinary patient receives. Further to this, Welsh and Wager (2013) suggest that an additional VN-led admission can ensure questions put to the client, which incorporate OJAM's ten abilities, generate a less disease-focused approach and can aid in strengthening the client–veterinary bond.
A paper-based client questionnaire was created by adapting the ‘Five Needs’ (RSPCA, 2014) and the OJAM to structure the underpinning questions. Orpet (2011) advises that to meet the requirements of individual patients, individual needs must be met and short- and long-term goals identified and set. To help make this possible, specific questions building on each of the patient's ‘needs’ and ‘abilities’ were asked as a way to help the VN identify key nursing and patient health goals. An example of these questions and the owner's responses are demonstrated in Table 1.
Table 1. Example of the questions and answers detailed in the client questionnaire
| Question | Owner's answer |
|---|---|
| Does your pet interact well with other animals? | Does not tolerate other dogs |
| What food does your pet eat? | Wet/tinned food, does not like Chappie |
| What type of water bowl does your pet drink from? | Raised metal bowl next to food bowl |
| Does your pet have a heat aid when sleeping or do they prefer cooler areas? | Prefers to be cool, will often sleep by the door on the bare floor |
Questions regarding the patient's current medications were also included which provided the opportunity to discover how the patient would best tolerate the administration of medications while hospitalised and to ascertain how best the client would be able to continue any medications at home.
A VN-led face-to-face admission interview with the client was incorporated into the normal admission process and a paper copy of the client questionnaire completed by the VN, via the client. The client was able to inform the author of specific behaviours that the patient displayed and even though this was a time of distress, the interview allowed the owner to relax and even be jovial when characteristics of the patient were described. Supporting the findings of Lock (2011), the author found that this process helped to strengthen the bond between the VN and the client. Evidence of this could be demonstrated by the fact that a personalised gift was received from the client to the author, thanking her for the care and support she had provided. This was in contrast to the author's previous experiences, in which client contact was minimal or totally absent.
Patient ability assessment
Information gathered during the client interview was then transferred onto the Patient Ability Assessment form. The author designed the Patient Ability Assessment form by adapting the OJAM example of a completed, patient assessment plan provided by Turner et al (2011). Adaptations included the inclusion of a ‘Lifespan’ diagram taken from the Roper Logan Tierney Model (RLTM) (Roper et al, 2000) to allow the patient's age to be plotted and easily noted. To ensure a specific plan of care could be created for the patient, visual and physical assessments were carried out by the VN. These assessments included noting the parameters of the patient's vital signs (such as temperature, pulse and respiration rate), assessing mentation and undertaking an initial pain score. This was carried out on admission so that any improvement or deterioration can be highlighted and acted on.
Care planning
When the initial information from the patient's ability assessment had been collated, clear nursing diagnoses were then made. While it is acknowledged that a VN cannot, by law, make a clinical diagnosis; the aim of the veterinary nursing diagnosis was, as suggested by Welsh and Wager (2013) to highlight problems associated with the ten abilities, and thus consider any nursing interventions which might be necessary to prevent and/or alleviate any of the identified health issues.
From the nurse diagnosis, potential and actual problems were identified and inserted into the care plan (Figure 2), goals were created and nursing interventions considered and specified. With the nursing interventions clearly highlighted the author was able to use these to review the initial clinical parameters to prevent patient deterioration and maintain the normal abilities.
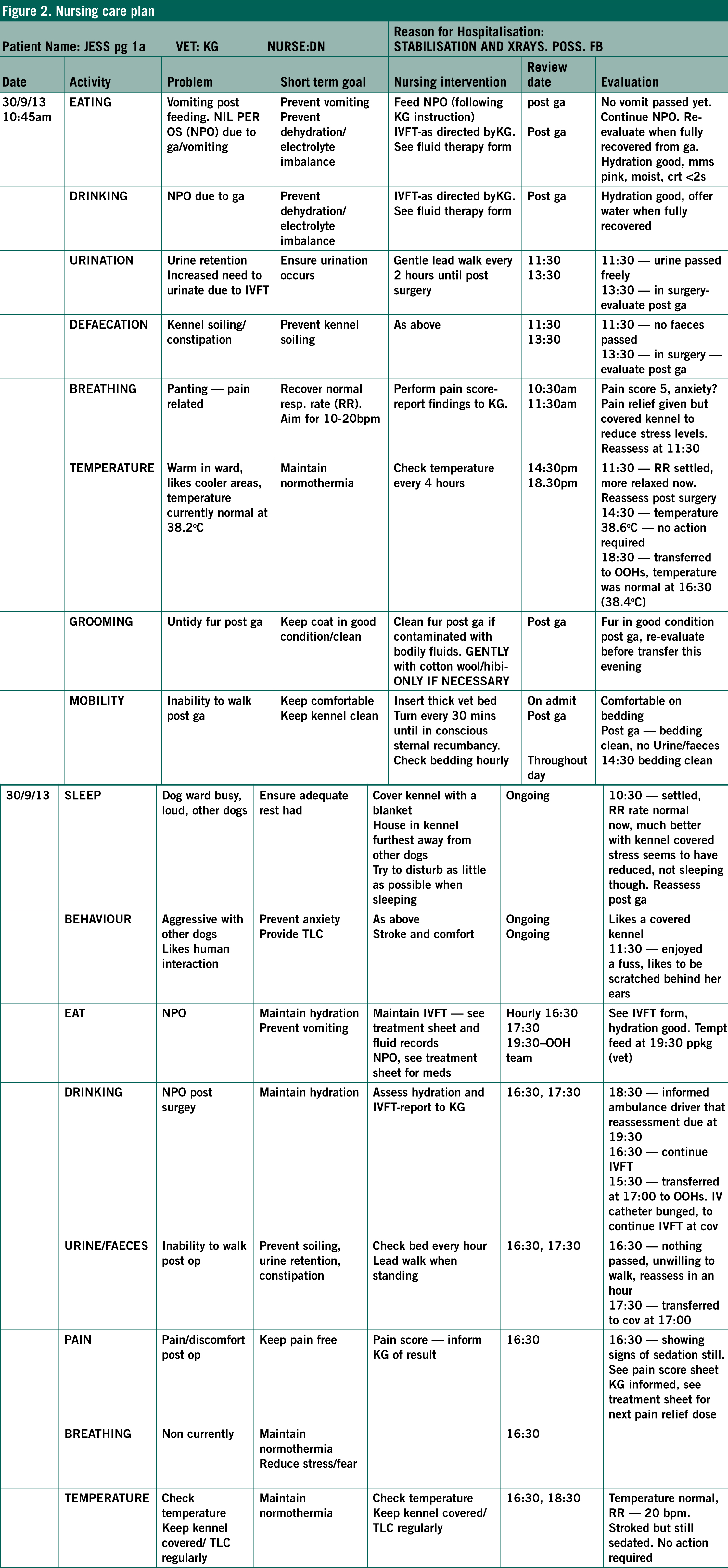
The evaluation of the care provided was the measure of how effective the interventions were and whether the goals had been met (Jeffery, 2006; Orpet, 2011). As described by Welsh and Wager (2013) using the OJAM ensures a structured and holistic approach to this evaluation and is an essential part of the process. Once this stage is complete the assessment phase can be revisited and the cycle of the nursing process continued.
Implementation of the care plan
Mason (1999) suggested that in human medicine care plans were poorly implemented in practice and some literature implies this finding may be being mirrored in veterinary nursing practice (Lock, 2011; Welsh and Wager, 2013). It was concluded by researchers Fernández-Sola et al (2011) that to accomplish the implementation of care plans, great effort is required. The first author (DN) wanted to encourage colleagues as much as possible before implementing the new documentation and convened a meeting with the veterinary team prior to the admission of Jess, with the purpose of defining the goals of the activity and to encourage team participation.
The meeting had a positive effect on the implementation of the NCP. The staff reported they had felt informed of the reasons it was being trialed and agreed to the potential benefits of the NCP. The added support from the team enabled the author to spend time with the client and the patient and allowed the NCP to be utilised and continued by other members of the team. As Cory (2007) states, the implementation of NCPs is not the responsibility of just one nurse but instead requires commitment from all members of the veterinary team.
The concept of care planning was not new to the student veterinary nurses (SVNs) in the author's (DN) practice. At the time of writing this article, the Royal College of Veterinary Surgeons (RCVS) syllabus includes human nursing models and care plans, such as the RLTM (1996) and Orem's (2001) self-care model. The introduction and incorporation of care planning into the students’ current practice caused excitement amongst the group; the students believed they would be putting their theory into practice. One SVN stated: ‘It's exciting to see the theory we're taught being used in ‘real life”. This is also supported by Lock's (2011) own clinical experience, who noted that it was junior members of her team that were more eager to participate in the use of new care plans. However, the enthusiasm towards the care plan did not necessarily equate to a full understanding of how to use them. Although the SVNs were willing to participate, their knowledge and ability of applying nursing models and completing the paperwork was limited. When later asked what difficulties the SVNs had faced when working with Jess's NCP, the response was that the concept of nursing models had not been fully understood. The students further explained that the RLTM (1996) and Orem's self-care model (Orem, 2001) had been taught during their course but, in their opinions, not in great detail. They had previously found the application of the human-based models difficult and impractical in veterinary practice and had little or no knowledge of the OJAM. These findings are supported by experiences of Wager and Welsh (2013), who also described that SVNs and qualified VNs found the application of human-based models into veterinary nursing practice challenging.
Overall the SVNs reported that they felt empowered by the process and that confidence in their abilities improved. Research in human nursing practice found that when nursing students had a legitimate place in a team, confidence and self-esteem improved (Stapleton et al, 2007; Bradbury-Jones et al, 2011; Brown, 2012). The use of the NCP had a positive effect on the nursing care provided by the SVNs in the practice, as it allowed the nursing team to form detailed discussions regarding care planning.
In contrast to the opinions of the SVNs, the qualified VN in the author's clinic expressed anxiety and apprehension in regards to using an NCP for Jess. It is not uncommon for this reaction to be noted. Wager and Welsh (2013) reported that many of the experienced VNs undertaking the RVC's Graduate Diploma in Professional and Clinical Veterinary Nursing felt anxious and stressful when implementing care plans into their clinical practices.
Although the qualified VNs had substantial post qualification experience, the concept of nursing models was new to them. Resentment towards the NCP was voiced directly to the author and when asked why they felt this way, the consensus was that they believed themselves to already be accomplished in nursing without having to rely on a written care plan. Wimpenny (2002) and Lock (2011) also discovered that experienced nurses were less inclined to adopt new concepts of nursing. If the nursing process is something that is inherently applied by experienced qualified veterinary nurses without conscious thought (Orpet, 2011), it is possible that it is the perception of these plans that needs to be altered. Main (2011b) suggests the NCP should bring nursing ideas together, especially when nursing interventions are evaluated and administration of care adjusted. With the planning of patient care being a vital part of VN practice (Wager and Welsh, 2013) the continued use of NCPs may increase familiarity and change the view of their use to a more positive one.
Further to the staff perceptions, reflecting on Jess’ care plan enabled the author to identify two further themes involved with the implementation process: the time it took to complete the NCP; and the amount of paper work created by the NCP. To understand the impact of NCPs in working practice the themes are explored further:
- The NCP took too long to complete — the process involved with completing the documentation was lengthy. Before the introduction of the NCP the normal routine was to write basic interventions, such as lead walking or feeding time, on the practice's medical-based hospital sheet. Using an NCP for Jess meant writing specific considerations and interventions which inevitably took longer. Brown (2012) had similar experiences and stated that the NCP was a long and detailed document, which added additional time to complete. Unfortunately the author found that completing the NCP did mean that direct care given to Jess was delayed, but not to an extent that it was detrimental to her wellbeing. Similarly this has been noted by Mason (1999) and Wager (2011) who discuss the conflict between the completion of documentation and providing direct care. Brown (2012) suggests that although the time it takes to complete an NCP is a significant factor to their successful adoption in practice, the unfamiliarity of the NCP process could be a cause for this and with experience, the time it takes to complete could be reduced. Based on this experience, a noted concern was that the NCP was, in itself, additional documentation which, with the additional time needed to complete, might make nursing more than one patient in this way difficult. These concerns lead on to the second theme.
- The NCP created too much paperwork — there is no question that the NCP increased the amount of paperwork to be completed by the VN team. Observations by Wager (2011) also showed that an undesirable result of implementing an NCP was that excessive documentation was created.
The primary author's and author's colleagues initial reaction to the paperwork was that the addition of the NCP created an overload of forms. In reality, the NCP (including the client questionnaire) equated to a total of three more extra pieces of paper. It seems pertinent to question why there is such widespread perception of NCPs creating an ‘overload’ of forms and excessive paperwork? It could be explained by the fact that there is already excessive documentation in the author's practice and the addition of more paperwork had made this issue more apparent. Mason (1999) stresses that by tailoring NCPs to the requirements of each specific clinical area, duplication and collation of unnecessary data can be avoided. Lock (2011) discussed how a care plan can be adjusted in several ways reducing repetition. This is further supported by Wager (2011) who concluded that insufficient adaptations of NCPs prevent integration with the hospital's existing paperwork.
With this in mind revisions to the NCP may need to be considered to further reduce the paperwork burden and as advised by Wager (2011), it is advantageous to include the VN team in these discussions until an optimal template is reached. NCPs in the author's practice could be adapted further, allowing integration with the current paperwork. In turn reassessment of the current documents could be achieved to improve practice efficiency.
The author found that the design process was difficult to complete alone. The collation of information was both time consuming and stressful. As previously stated a suggestion to improve this in the future is to design NCPs with input from the entire team. This enables the concept to be shared and creates communal responsibility. Mason (1999) found that local ownership of care plans gave a sense of duty to the nurses. They also identified strongly with their patients, compared to those who felt the care plans were ‘imposed from above’.
Evaluation and ‘reflection on action’ is an important process in professional development (Carlson et al, 2008) and so an important question to ask is: ‘Did the NCP have an effect on the care given to Jess?’ In the author's opinion the NCP did have a positive effect on her care. The VN-led admission allowed the author to understand important aspects of her behaviour and normal routine. These may have been missed in a normal VS admission (Welsh and Wager, 2013). Coakley and Mahoney (2009) and Christian et al (2006) explain that multiple stressors can impact on the experience, wellbeing and recovery of a patient. Stress can slow the rate of wound healing and can have a significant negative impact on the overall success and speed of an animal's recovery. By discovering that Jess did not like the company of other dogs and preferred to sleep in cooler areas, nursing interventions (such as applying a fan and covering her kennel) may have contributed to the improvement in her vital signs and possibly helped to reduce her stress. These subtle interventions, which under normal circumstances may not have been carried out, help to demonstrate how this NCP encouraged a holistic nursing approach to Jess's care and facilitated more than usual critical reflection. The evaluation provided an opportunity to review the nursing care and make suitable adjustments. In performing this process consciously, the author sensed a feeling of achievement and supported one of the fundamental responsibilities of the VN, which is to make animal health and welfare their first consideration (RCVS, 2012).
Since creating this NCP for Jess, the author and her colleagues continue to use and review NCPs in their day-to-day work and have made further modifications to the template with the aim of making the process of completing it more efficient. This modified NCP template has been introduced and implemented across five practices within the author's company, allowing for all staff to adopt its individual approach to care. This process has had a positively empowering effect on the VNs involved and significantly has created recognition of the evolving holistic care approach with the senior members of the company.
Future considerations
To meet the challenges of a complex profession such as veterinary nursing, education is of vital importance (Clarke, 2010). At the time of writing, it appears the OJAM has not yet been introduced into the VN syllabus (Royal College of Veterinary Surgeons, 2010; City and Guilds, 2013). Due to the model's focus on animals as patients, the integration of this into the VN course could enforce its value and aid in the application of nursing models by SVNs. Continued professional development in models of nursing for qualified VNs, could help to reduce some of the reported negative perceptions surrounding the implementation of NCPs. The integration of the OJAM into pre- and post-registration training programmes could further improve the understanding of the professional responsibilities of the VN. This would further help to ensure that an individual, patient-based approach is the focus of nursing care provision and provide veterinary nurses with the necessary documentation to support their clinical practice activities. Further research into the potential and actual clinical benefits of NCPs as a way to facilitate holistic veterinary nursing would add to the current literature surrounding NCPs and start to provide the evidence base so desperately needed to support their use in practice.
Conclusion
This article provides a reflection on the design and implementation of one NCP in clinical practice. There were problems with the implementation of this care plan, as highlighted in the article, which include an increase in time spent completing the NCP and an increase in the documentation it was perceived to create.
From the author's experience and the evidence from the available literature, it is clear that modifications to all of the existing NCP frameworks are beneficial to ensure the adoption and use of care plans into practice. With necessary adaptations made to the paperwork and the inclusion of the VN team in the decision making and implementation of new initiatives like this, the identified problems become less of a reason not to use them. The potential benefits that NCPs provide in encouraging more patient-focused, holistic nursing care to individual patients outweigh the negatives. With suitable and careful adaptations from the whole VN team, NCPs can be utilised efficiently and empower VNs in their day-to-day routine.
Key Points
- The nursing care plan (NCP) had a positive effect on the patient and encouraged a holistic approach to care.
- A veterinary nurse (VN)-led face-to-face admission interview with an owner helped to strengthen the bond between the VN and the client.
- Discussing the implementation of a NCP with the veterinary team, prior to its use, helped define its goals and encouraged team participation.
- Revisions to the NCP should include the whole VN team until an optimal template is reached.
- Reviewing the whole nursing process created an opportunity to reassess the nursing care and make suitable adjustments.


