The term syringomyelia (SM) refers to the development of fluid filled cavities or holes known as a syrinx within the spinal cord of the affected patient (Rusbridge et al, 2007). These syringes are thought to contain extracellular or cerebro spinal fluid (CSF) (Klekamp, 2002). In dogs the most common cause is secondary to chiari malformation (CM). CM characterized by a mis-match in brain and skull size results in obstruction of the foramen magnum and changes in the dynamics of CSF flow. Toy dogs, in particular the Cavalier King Charles Spaniel (CKCS), are most commonly affected by chiari-like malformation and syringomyelia (CMSM) (Lamb and Pfeiffer, 2003; Rusbridge, 2005). Although identified as early as the 1960s (McGrath, 1965), incidence of the disease until the 1990s was thought to be low. However, advancements in diagnostic equipment, such as magnetic resonance imaging (MRI), has lead to an increase in diagnoses in canine patients (Bagley, 2000). With varying presentations, the most significant clinical sign of the condition is pain, thought to be multifactorial resulting from both obstructed CSF flow and spinal cord damage (Rusbridge, 2005). Stalin et al (2008), question stenosis or abnormal widening of the foramen magnum as contributory, while work by Takagi et al (2005), suggest compression of the atlanto-occipital joint as contributory. Cerda-Gonzalez et al (2006), and Meadow et al (2006), identified the condition to be a multifactorial disease with various explanations for its occurrence in the presence of skeletal abnormalities. Human sufferers of the condition report headaches, neck and back pain, and a burning or stretching sensation of the skin (Todor et al, 2000). Some canine patients present with neurological deficits, ataxia and pelvic limb weakness. Other possible clinical signs include scoliosis (Figure 1) and scratching which is typically one sided and without making skin contact (Rusbridge et al, 2000). Affected animals may have an abnormal head carriage position particularily when sleeping.

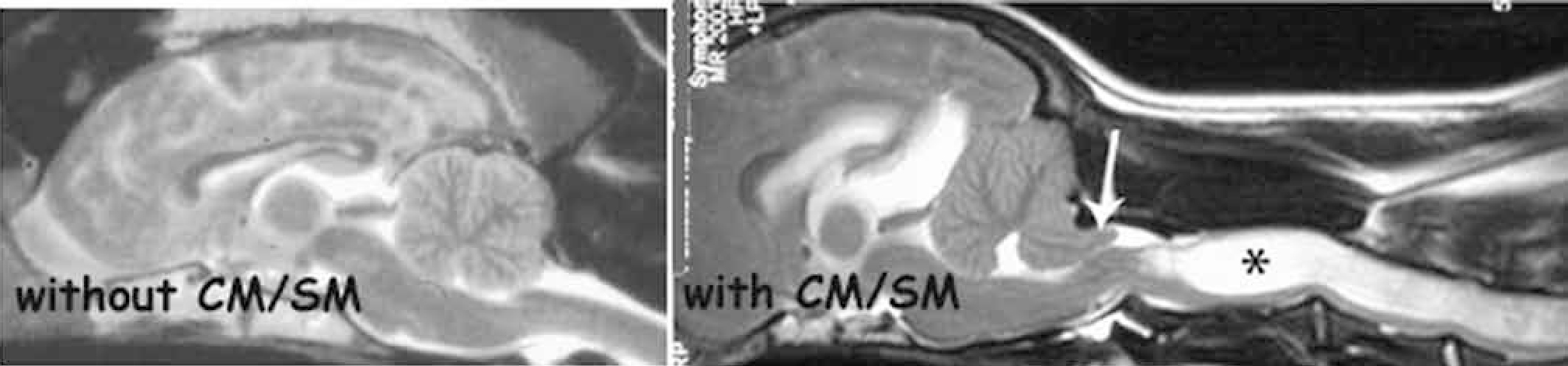
While experts agree that diagnosis of the condition relies on images produced using MRI (), opinions on the most appropriate treatment of the disease vary, with arguments being held for both medical and surgical management of the condition. With a known link to the hereditary nature of CMSM and with work underway to identify a gene responsible for both CM and SM, the influence of intensive consanguineous breeding and its negative effect cannot be under estimated (Rusbridge et al, 2005). This in itself presents another area for further research into future management and ideally prevention of this debilitating condition. Regardless of the approach, the main aim of treatment in these patients is to reduce pain and obvious clinical signs exhibited by these animals. Judging success of treatment and in particular reduction of pain can be problematic in canine patients as it relies largely on the clinician appropriately interpreting the often subtle signs and behavioural changes linked to pain response.
Current management options
Medical management of the condition uses a variety of drugs which, although similar in their aim, may vary in their mode of action, and range from common analgesics such as carprofen or meloxicam, through to neurological pain relievers such as gabapentin and alternatively steroids (Table 1). In addition to this, medication to reduce CSF formation and pressure may also prove useful (Rusbridge et al, 2006). Given that the reason and factors contributing to neuropathic pain, as experienced by these animals are multiple, attempted management of the pain often requires combined use of multiple drugs (O'Hagan, 2006). Although much of the currently published research into this subject identifies various drug groups as being useful in management of the condition, a true understanding as to why, and the laboratory evidence to support and explain these findings, may be lacking (Vela et al, 1979). The lack of long-term studies of medically managed patients is further problematic, with treatment aims and expected outcomes often being based on findings in human studies. Added to this are the problems encountered when implementing long-term therapy with some of these agents, with side effects ranging from hypergastrinemia (Berlin, 1991), abdominal pain, lethargy and weakness all having been reported (Rusbridge et al, 2006). Despite this supporters of medical management argue this to be the preferred treatment option of the condition, due to surgical outcome in these patients being unreliable. Although clinical improvement may be noted following surgery the syringomelia is generally persistent (Dewey et al, 2004; Rusbridge et al, 2006), and patients may still experience significant pain (Nakamura et al, 2004). Medical management may also be indicated in patients whose clinical signs are mild or for those cases in which surgery is not an option, or results in only limited improvement (Rusbridge and Knowler, 2002).
| Drug type | Examples of drugs used | Possible side effects and contraindications |
|---|---|---|
| NSAIDS | Carprofen, meloxicam | Can result in vomiting and diarrhoea |
| Neurogenic pain relievers | Gabapentin, pregabalin | May result in mild sedation +/− poor coordination especially at start of treatment |
| Corticosteroids | Prednisolone | Can result in vomiting/diarrhoea especially at high doses |
| CSF production/pressure reducing | Frusemide | Depleted potassium |
| Cimetidine | Liver/kidney toxicity |
|
| Omeprazole | Gastrointestinal disturbances |
Surgical management may vary in the technique used but is indicated in patients who fail to respond to analgesics or those experiencing neurological deficits (Rusbridge et al, 2006). One commonly performed surgical technique is foramen magnum decompression, aimed at reducing pressure on the cerebellum and improved flow of CSF. Indications for the use of the technique lie largely in its success in managing the human form of the condition, with patients undergoing this form of surgery experiencing a halt in progression of the disease or sustained improvement of clinical signs (Dewey et al, 2005). Another technique used involves the placing of a shunt, which is inserted into the syrinx to drain it to another part of the body. Given that shunting directly addresses two of the suspected contributing causal agents of the condition, surgical results should be favourable, but as in the human field findings are variable (Bagley, 2000), with complications including shunt occlusion and a morbidity rate as high as 42% in human patients being associated with some forms of the technique (Lee et al, 1995).
While it is not uncommon for research into either form of management of the condition to produce contrasting findings, the hurdles faced when performing research into either treatment option are often similar. Much of the current published work results from studies containing low patient numbers and often single animals. Interpretation of treatment success or failure is often taken from an owner's interpretation of improved clinical signs and not from measurement of a repeatable parameter such as heart rate or respiration. In addition, lack of long-term patient follow
Summary of current findings
While clinicians may vary in their suggested management of the condition, the need for further research into the condition, its effects and appropriate management appears to be a topic on which many agree. As stated earlier studies often contain low patient numbers who also receive only short-term follow up, which presents problems when trying to draw conclusions on a treatments success or failure. Medical management makes no claims to be curative, but simply to reduce pain experienced during whatever time these patients have left and hopefully slow progression of the disease. Work by Rusbridge and Jeffery (2008), identify the need for multicentre studies to rationalize the approach when medically managing these patients. Treatments proving successful in the management of neuropathic pain in humans would provide a logical starting point for further trials and research. Establishment of a suggested medical treatment would be beneficial especially to first opinion clinicians, to aid in selection of appropriate medications and avoid inappropriate prescribing of drugs known by others to be of little or no effect in these cases. Being able to provide owners with realistic expectations of treatment success would also prove beneficial, although this would obviously prove difficult due to the lack of consistency in patient response to treatment from one case to another.
Initial hopes for surgical management may have been to cure these patients of the disease, but recent published studies identify only reduced pain levels, decreased exhibition of clinical signs and delayed progression of the disease in some patients, which was often only in the short term (Vermeersch et al, 2004;Rusbridge, 2007). In the same way as occurs with medical management, continued research into surgical techniques uses those procedures proving successful in management of the human equivalent of the disease as a starting point for further studies. Support for surgical management of the condition would be strong, if it were to follow that the disease could be cured by correction of the underlying anatomical or functional abnormality, as attempted during surgery on these patients. Post-operative images produced by MRI, display in many patients, images similar to those first recorded pre operatively, highlighting the failure of surgery to remove the fluid filled syrinx associated with the disease. A stark contrast in post-surgical findings among authors is further problematic when trying to reach solid conclusions of treatment success, with some authors reporting no improvement (Vermeersch et al, 2004), while others note post-operative resolution of the syrinx (Dewey et al, 2005). Careful consideration to surgical technique should be given, with scar tissue formation at the surgical site becoming problematic in some cases. Work by Muraszko et al (2004), reports up to 55% of surgical patients having extensive scar tissue formation leading to further obstructions in CSF flow, which can result in the need for further surgery and continued pain. If surgical treatment were to prove successful efforts would need to be made to increase both awareness and accessibility of this as a treatment option both to veterinary surgeons and owners alike.
Recommendations for further study
It seems likely that Rusbridge et al (2005) have the answer in that successful treatment of this condition lies not in medical or surgical management, but with identification of the gene responsible for this disease and from this the establishment of an appropriate breeding programme. This is particularly important given that some animals identified as suffering from the disease exhibit no clinical signs (Couturier et al, 2008), meaning that owners can unknowingly breed from animals affected by the disease. The work by Rusbridge (2005) identifies data which suggest that occipital bone hypoplasia, known to be contributory to syringomyelia, is inherited in the CKCS (Rusbridge and Knowler 2003; 2004), and to identify the gene or genes responsible would allow development of a test to identify sub clinically affected dogs and those carrying the gene. Given that the breeding of only mildly affected animals often results in severely affected offspring (Rusbridge et al, 2005), this would prove invaluable in reducing the number of animals born who go on to suffer from this debilitating condition. However, this suggested management would fail if owners and in particular breeders were not compliant in acceptance of the condition and screening of their potential breeding stock. With this in mind a strong argument can be made for compulsory testing of all breeds predisposed to this condition. A proposal for a British Veterinary Association (BVA)/Kennel Club (KC) MRI screening scheme has been submitted to the BVA/KC Management Committee and is currently under their consideration.

Recommendations for veterinary practice
Until a clear treatment approach is decided on and while work into identification of the gene responsible continues, clinicians treating these animals must be guided by the individual animal and their response to treatment. What is clear from the work published is there is no one size fits all approach to management of the condition, with both medical and surgical treatments experiencing large variations in success dependant on the individuals concerned. If it were proven, as suggested in some studies, that swift surgical intervention following diagnosis of the condition, did in turn lead to improved prognosis in these animals, support for early surgical management would be strong. This would prove invaluable for those animals in which surgery is an option, but still leave a definite need for a structured approach to medical management for those animals for whom surgery is not possible. Following diagnosis, initiation of medical management would appear in most clinicians' opinion an appropriate first approach to treatment. Beyond this, treatment will ultimately be dictated by patients' response and owner expectation and circumstance. While it may be problematic in the context of a research paper, where reliance is on statistical evidence to prove a theory, relying on owners to identify a positive response to treatment and reduction of pain in their animals following either form of management is clearly beneficial. This is given that they are the first to identify changes in their animal, likely as a result of pain, which in turn leads to presentation in practice. An owner's interpretation of improvement in their animal likely means a reduction in clinical signs and pain-related behaviour changes that first led them to seek veterinary attention. Secondary to this is that improvement of the condition on images such as MRI are irrelevant if the owners are living with an animal who they deem as being in unacceptable pain, often leading to euthanasia. With such variation in reported treatment success and given the need for further research, it would seem appropriate to focus owners' expectations on reduction of pain, clinical signs and delayed progression of the disease, and not on a cure for their animals at this current time.
Conclusion
Both readers and researchers will struggle to draw solid conclusions from much of the currently published material on this multifactorial disease, due to the lack of consistency in reported findings regardless of treatment approach. Credible studies usually rely on the use of a control group in which some patients will receive no treatment or placebos to prove or disprove a theory. To achieve this using animals known to be suffering from the disease would clearly prove difficult as this essentially means withholding medication or surgery from some animals, which obviously brings with it ethical concerns. Despite this, and although struggling to reach a decision with regard to the most appropriate management of CMSM, an argument for the need of further research can easily be made. This research should include studies into the under lying cause and contributory factors of the disease, especially given that the current treatment available is often ineffective in managing the pain associated with syringomyelia (Baron, 2000). The hope would be that greater understanding of this debilitating condition would lead to more effective treatment. Multiple theories have been proposed but true understanding as to the exact cause of the condition still remains unclear, with many authors varying in their opinion.
