Although many wounds are amenable to simple closure by apposition of wound edges, this is not always possible, either because the wound is too large, or because apposition would result in distortion of the sutured skin, leading either to poor cosmetic outcome, or to poor function. An example of the latter would be removal of a mass near the eye, where simple closure may lead to distortion of the eyelid. In other cases, direct closure of a wound may be possible only by suturing the wound edges under tension. Tension is to be avoided in any surgical repair, as it reduces the likelihood of wound healing. Pulling wound edges together under tension results in stretching and narrowing of blood vessels, thus reducing blood supply to the wound edges. Tension also reduces the migration and division of fibroblasts and epithelial cells. Judicious use of walking sutures, or other tension-relieving sutures, can reduce a certain amount of tension at wound edges, but where a large skin deficit exists (or in regions of minimal ‘spare’ skin, such as on the limbs), there may just be too little skin to stretch over a wound. Options for enabling closure of a wound include:
Types of flaps
The reason flaps heal more consistently than grafts is that they are not reliant on the recipient bed for their nutrients, carrying a blood supply with them (Aper and Smeak, 2003). The nature of that blood supply characterises the type of flap: random, axial or myocutaneous.
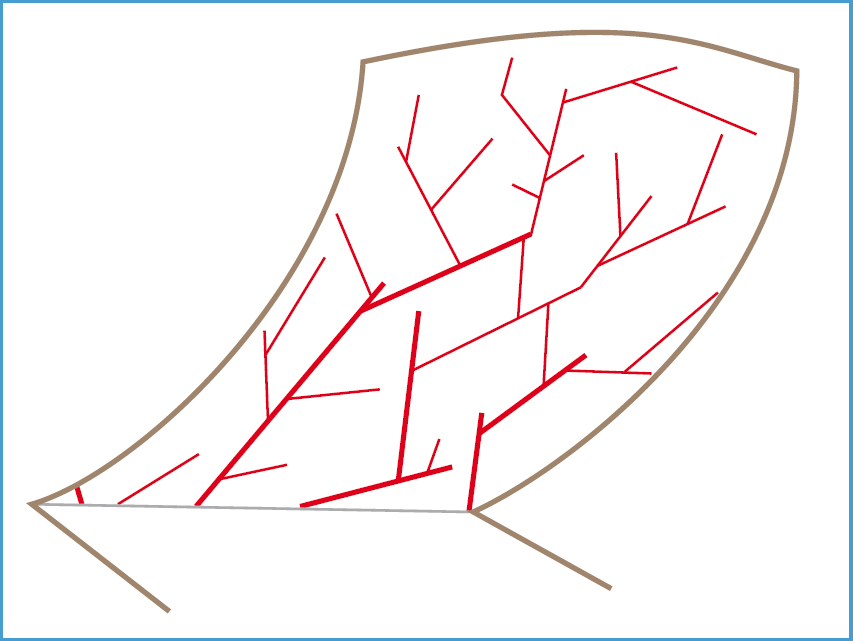
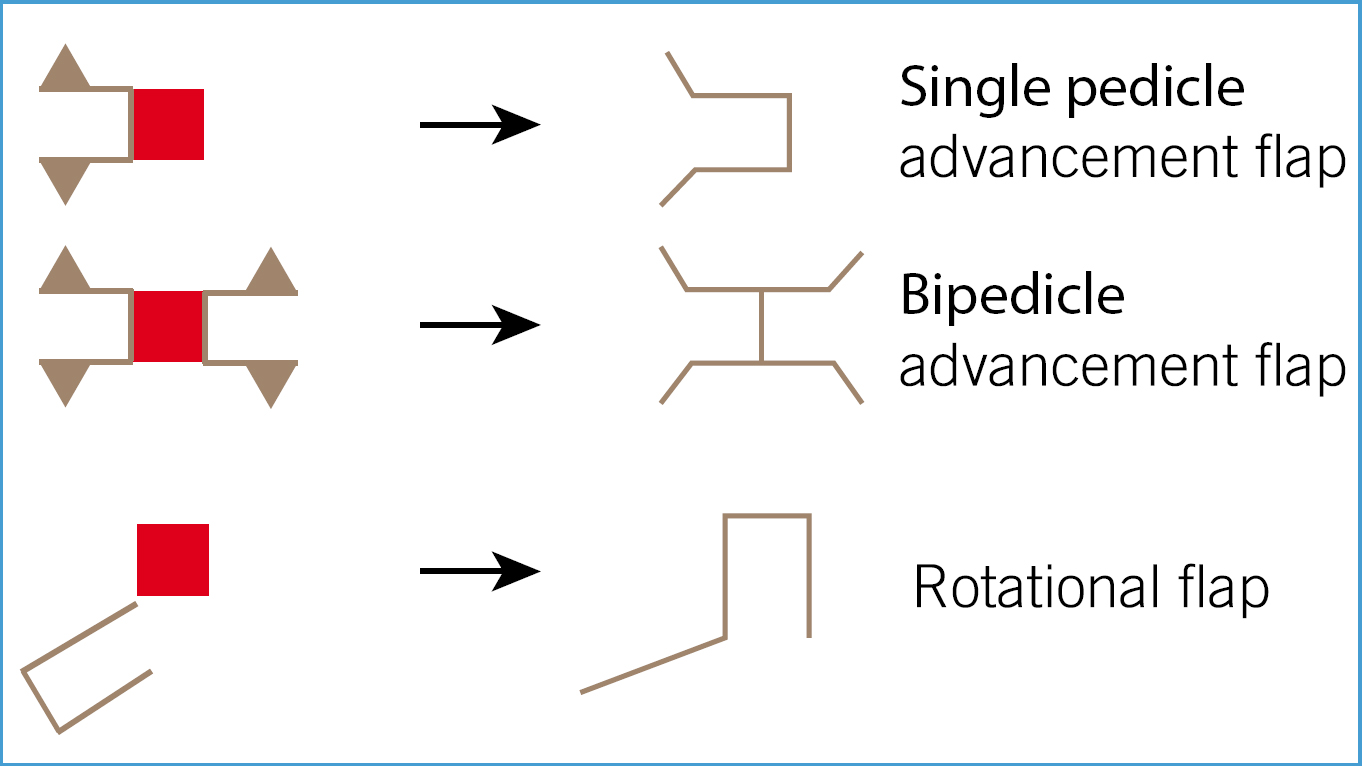
Random flaps (Figure 1), otherwise called local flaps, rely on the blood supply through the subdermal plexus to provide nourishment to the flap. The length of the flap should not exceed three times the width: this may result in poor blood supply at the tip of the flap, which could lead to wound dehiscence (Fowler, 1999). In general, the wider the flap at its base, the more likely it will be to survive. The lack of anatomical knowledge required for random flaps, and the ease of dissection and relative reliability make them extremely versatile techniques for wound closure. Random (subdermal plexus) flaps may be used in a number of orientations or confgu-rations (see Figure 2).
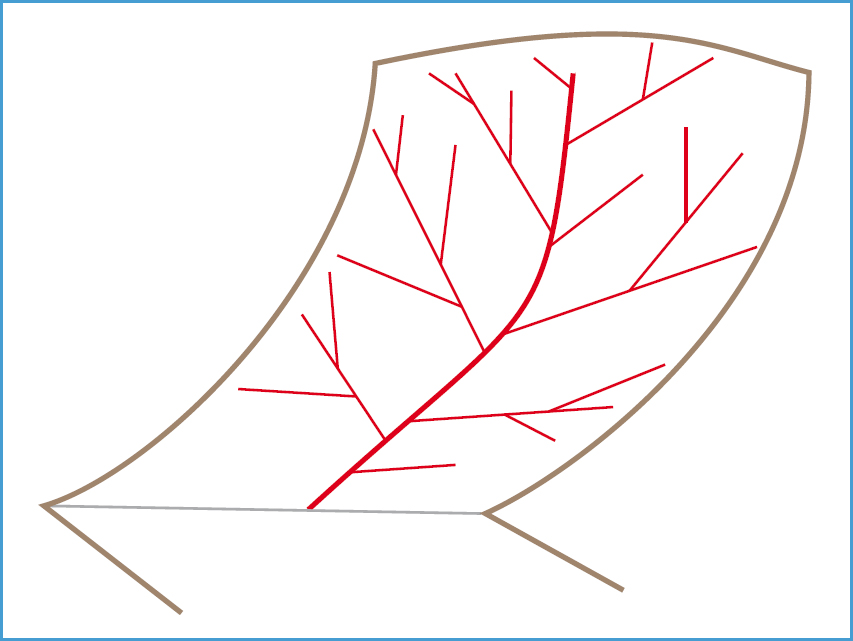
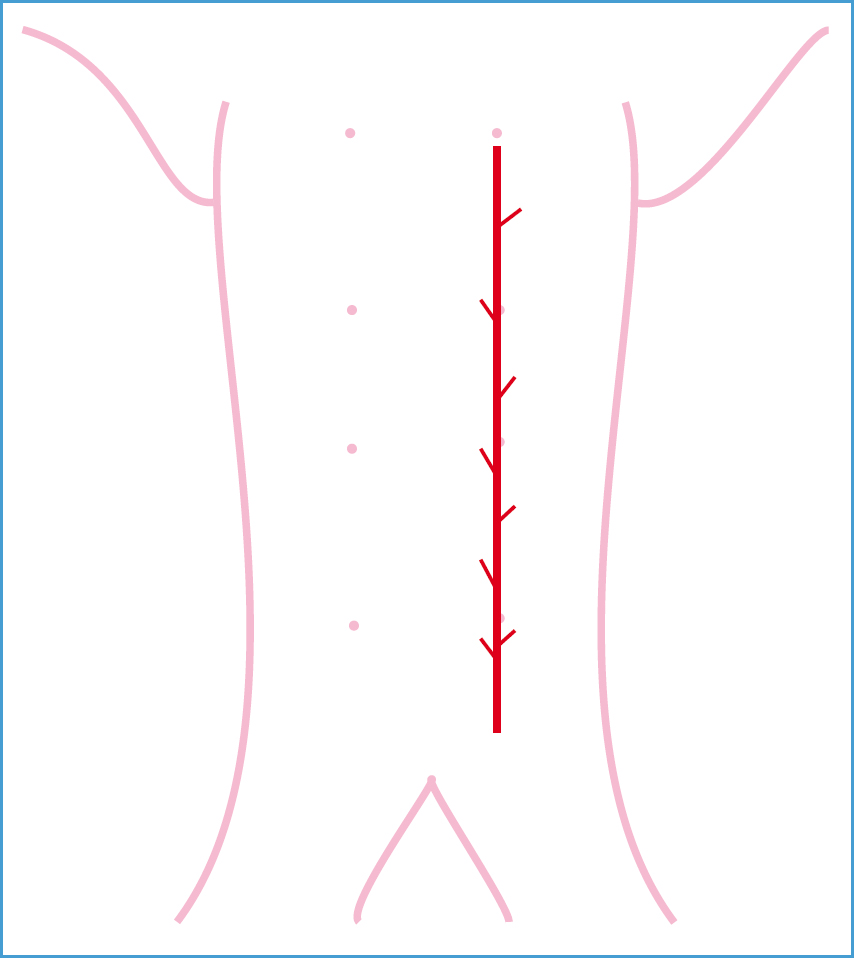
Axial pattern flaps (Figure 3), depend on the siting of the flap over a known direct cutaneous artery and vein. The base of the flap is sited at the origin of the artery, while the flap itself includes the area of skin directly fed by that artery (known as the angiosome). Over a dozen such arteries have been described (ter Haar et al, 2013); the most commonly-used ones being the caudal superficial epigastric artery and the thoracodorsal artery (Figure 4). Although some anatomical knowledge is required to locate the flaps, no specialised equipment is needed and the flaps are easy to dissect. Disadvantages to axial pattern flaps include the requirement for lengthy and extensive dissection to produce the flap: this results in a large defect at the donor site which may need undermining of a large area of skin to close. Nevertheless, axial flaps are invaluable tools for wound reconstruction and can be used to cover wounds on any part of the body, except the distal limbs beyond the carpus/tarsus.
Myocutaneous flaps involve the elevation of skin and underlying skeletal muscle. The rich vascular supply of muscles ensures a high degree of wound healing, and these types of flaps are useful in reconstructing wide and deep trunk wounds following oncological resection. However, they are technically more challenging to perform than random and axial flaps. They are not discussed any further in this article.
Planning for reconstructive surgery
General rules for patient preparation should be followed (Prisk, 2014), with a few additional cautions:

Case examples
Case 1: random flap for reconstruction of upper eyelid
‘Hopper’, a 7-year-old male neutered lurcher, incurred facial injuries running into a stone statue. On presentation, the right upper palpebra had suffered severe contusions and tissue loss (Figure 5). The dog was anaesthetised and the wound was clipped and flushed copiously with sterile saline (Figure 6); traumatised tissue was debrided. A small section of frontal bone at the dorsal aspect of the orbit had been chipped off, exposing the frontal sinus. The frontal sinus was flushed with sterile saline, having packed the nasopharynx with swabs to prevent aspiration of flushed material. The orbital periosteum was elevated and used to close the frontal sinus.

Due to the loss of some of the eyelid tissue by abrasion, and a further loss by debridement, it was decided that simple closure of the wound would lead to distortion of the upper palpebral margin, and a reduced ability to close the eye. A Random flap (single pedicle) was elevated from the adjacent forehead skin and brought forward to cover the deficit. The wound was closed with simple continuous sutures of 4/0 monocryl (Figure 7).

The dog was kept overnight for observation and analgesia. The cosmetic appearance of the wound the following morning was acceptable (Figure 8); the dog appeared comfortable and was discharged back to the owner. The patient went on to make an uncomplicated recovery.

It was important in this case to reconstruct the eyelid in such a way as to avoid any distortion of the eyelid margin, as this may well have led to inability to close the eye, or else corneal irritation due to entropion. A subdermal plexus flap is very useful for reconstructions of this nature on the head, as the skin is reasonably loose, and if necessary extensive undermining will allow skin to be ‘borrowed’ from the neck.
Case 2: lip-to-eye mucocutaneous subdermal plexus rotating flap for reconstruction of eyelid defect
‘Tom’, a 13-year-old male neutered domestic short-haired (DSH) cat, presented with a history of a 1 cm diameter erythematous mass adjacent to the medial canthus of the left eye (Figure 9). Fine needle aspiration had yielded an abundance of blood, making it difficult for the lab to positively identify the nature of the mass. However, the presence of endothelial cells showing several nuclear criteria of malignancy was strongly suggestive of cutaneous haemangiosarcoma (Tyler et al, 1999) and so resection with a reasonable margin of excision was planned.

The cat was anaesthetised and the left side of the face was shaved and prepped. The mass was resected, with approximately 1 cm margins (Figure 10). The surgical kit was changed, including drapes and gloves, to reduce the risk of contamination of the excisional site with neoplastic cells.

At this stage, suturing the eyelid margins together would have markedly reduced the size of the eyelid fissure. A local random flap could have been performed, but this would have brought haired skin to the eyelid margins, risking corneal irritation. A flap of skin was elevated from the commissure of the lips and extended to a length just exceeding that from the lip to the eyelid defect. The flap was made full-thickness at the lip, to include approximately 1 cm of mucosa. A bridging incision was made between the excision site and the flap (Figure 11).

The flap was dissected free of subcutaneous attachments and brought up to the excision site (Figure 12). Any tension in the flap was reduced by further undermining and dissection of the flap.

Finally, the flap was sutured in place with 4/0 vicryl and the donor site (the lip commissure) was closed (Figure 13). ‘Tom’ went on to make an uneventful recovery.

Incidentally, the histopathology report confrmed cutaneous haemangiosarcoma with a narrow clear margin. Tom survived for a further 2 years, dying of illness unrelated to the tumour. The ideal margin of excision for feline cutaneous haemangiosarcoma has yet to be determined. Cats do seem to fare better than dogs after incomplete resection, suggesting that metastatic disease in this species is less common (van Nimwegen and Kirpensteijn, 2012). However, this case illustrates the need for biopsy prior to surgical excision, as second surgery would have been difficult to reconstruct. Fine needle aspirate (FNA) biopsies are simple to perform, minimally invasive and usually require no general anaesthesia (Hoad, 2014).
Case 3: Use of a caudal superficial epigastric axial rotational flap to reconstruct a mast cell tumour (MCT) excision wound
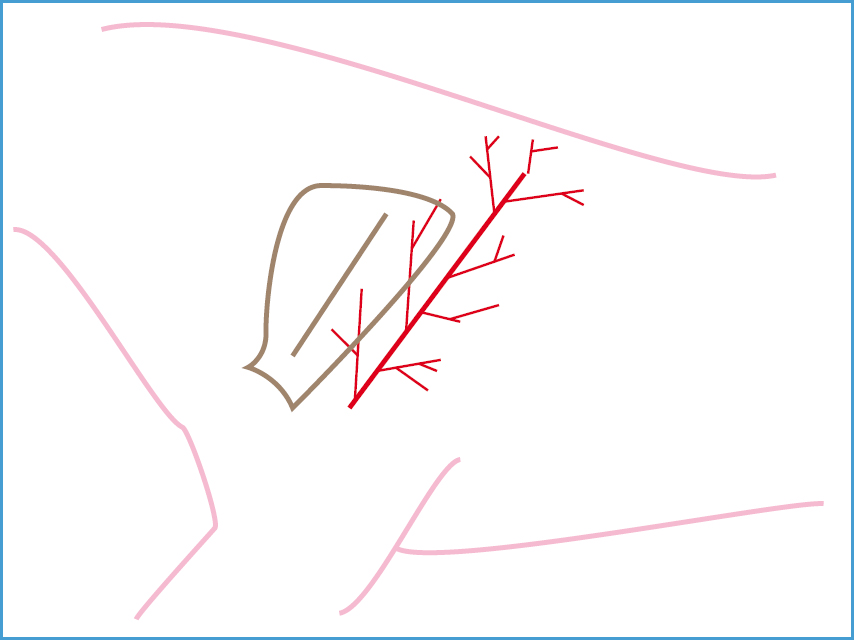
‘Indie’, an 8-year-old female neutered Boxer presented with a 2 cm diameter raised skin mass on the caudal aspect of the left thigh (Figure 14). FNA revealed a MCT of intermediate grade. Removal with 3 cm margins of excision were planned. Since the skin of the caudal thigh was not loose enough to cover the intended deficit, a caudal superficial epigastric (CSE) axial flap was decided on.

The dog was anaesthetised and a generous clip performed, to include the whole of the abdomen, groin and left hind limb to just below the stifle. The dog was placed in right lateral recumbency with the left hind limb suspended and the area was prepped for surgery. A sterile pen was used to mark the excision site and the proposed flap (Figure 15). The MCT was excised with 3 cm margins all round: since the mass directly overlay the popliteal lymph node, this was also excised (Figure 16).


The surgical kit, including drapes and gloves, were changed, to reduce the risk of seeding tumour cells from the excised mass back into the reconstruction site. A flap was created: the base of the flap was the left inguinal ring; the tip was the second mammary gland (Remedios, 1999). The flap was dissected free, being careful not to damage the artery and vein. A bridging incision was made between the base of the flap and the excision site (Figure 17). The flap was rotated laterally and sutured into position over the defect and the donor site was closed, utilising walking sutures to close dead space and reduce tension on the skin edges. Active (concertina) drains were placed prior to closure (Figure 18). The patient made an uneventful recovery — the drains were removed after 48 hours and the wounds healed without complication.


In the author's view, the CSE flap is technically the most straightforward and reliable axial pattern flap to perform; however, he has encountered one occasion where the artery stopped at the third mammary gland, with the result that the flap was of insuficient length to cover the deficit. The flap was closed and the author opted to raise an axial pattern flap incorporating the deep circumflex iliac artery instead; emphasising the need to have a ‘spare’ plan in mind.
Conclusions
Skin flaps are a valuable tool in reconstructive surgery, facilitating closure of relatively large wounds over almost all parts of the body. The survivability (heal rate) of flaps, especially axial pattern flaps, is better than that of grafts, and the cosmetic result is often far superior. There is no requirement for specialised instrumentation, and aftercare in most cases is minimal. It is important, however, to give the clients some prior warning as to the expected appearance of a large wound reconstruction, as some owners can find it disconcerting.

