References
Zoonotic parasite protection in the practice setting
Abstract
Cats and dogs carry a wide range of parasites with zoonotic potential. While much focus is placed on protecting owners and the wider public from these infections, veterinary staff are also at risk of exposure. Veterinary nurses may be exposed to parasites through direct contact with pets, indirect surface transmission, aerosols or via vectors. The risk of zoonotic parasite transmission, however, can be minimised in the workplace with a few simple practice-wide precautions. This article considers some of the routes of parasite exposure in practice and steps to reduce them.
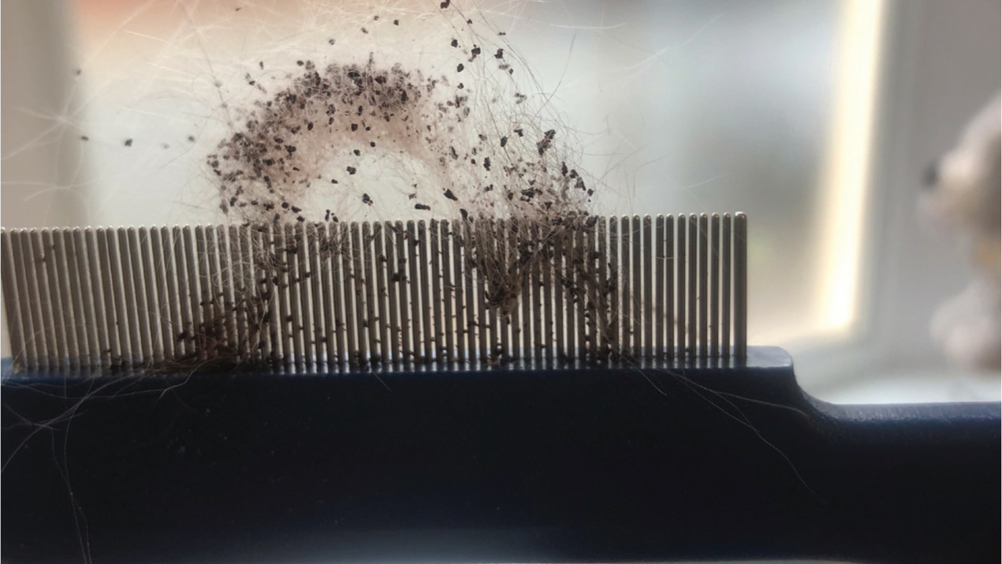
Working in veterinary practice puts both veterinary surgeons and veterinary nurses in contact with potentially zoonotic parasites. These pathogens may be transmitted through direct contact with pets, indirect surface transmission, aerosols or via vectors. Examples of pathogens transmitted through direct and indirect contact are dermatophytes (ringworm), mites (Sarcoptes, Cheyletiella), Bartonella spp. (via flea faeces) and Brucella canis. Bacteria such as Brucella spp., Bartonella spp. and Bordetella spp. may also be transmitted via the aerosol route. Fleas can easily become established in practices leading to flea-borne pathogen transmission, such as Rickettsia felis. Ticks are unlikely to become established indoors in the UK, but detached unfed Ixodes ticks can bite staff leading to potential transmission of Borrelia spp, Anaplasma phagocytophilum and tick-borne encephalitis virus.
The risk of zoonotic parasite transmission, however, can be minimised in the workplace with a few simple practice-wide precautions.
Bites and scratches leading to compromise of the skin barrier can in turn, lead to the introduction of bacteria and ringworm. Cat bites and scratches are a particular risk for Bartonella henselae (the cause of cat scratch disease) transmission via flea faeces trapped under nails or in saliva (Bouhsira et al, 2013). Planning and use of adequate restraint is vital before procedures are carried out on pets. Recording history of previous biting or scratching behaviour and history taking from owners regarding temperament are all important in the planning stage but cannot be wholly relied on. A risk assessment should be made as to whether muzzling, wrapping, sedation or anaesthesia are required. Some patients are more easily handled and less aggressive away from their owners and this may be established from the patient's history or through discussion with the owner. Safe and effective animal handling requires reading the pet's body language and a few moments should be taken to visually assess the patient before handling is initiated.
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

