X-rays are a form of ionising radiation. When x-rays interact with living tissues they produce electrically charged particles which can damage living tissues (Sherer et al, 2011). The two kinds of effects from ionising radiation are stochastic and deterministic effects, described in Table 1.
Table 1. Effects of ionising radiation
| Effect | Amount of radiation needed for effect | Effect of increased dose | Example |
|---|---|---|---|
| Stochastic | Any | Increases chances (probability) | Cancer |
| Deterministic | Above a certain level (threshold) | Affects severity | Skin damage, cataracts, infertility |
It is important to note that as there is no safe level of exposure to ionising radiation, any level exposure can cause cancer (Sherer et al, 2011). Historically, radiation protection in the veterinary context has meant protecting humans from harmful effects of radiation. Even though the topic is not properly addressed elsewhere in veterinary literature, it should be borne in mind that exposure to ionising radiation is also potentially harmful to the veterinary patient. However, when x-rays are used properly the benefits to the patient in terms of improved diagnosis greatly outweigh the risks. With respect to human staff, there is clearly no benefit whatsoever to a person being exposed to radiation as a consequence of their job. It should therefore be considered that any reduction of radiation exposure to a patient will also result in a lower exposure to staff members, should they be within the controlled area.
This article describes the various methods used to reduce radiation exposure to personnel and patients when performing radiography, with the emphasis being on methods available to the veterinary nurse.
What are the rules and regulations?
The main set of rules governing the use of x-rays are the Ionising Radiations Regulations (IRR 99). As these make heavy reading, the British Veterinary Association has published guidelines to help veterinary professionals work safely with radiation (British Veterinary Association, 2002). While these are designed for use in Great Britain, other countries such as Ireland and Canada have also published documents which help veterinary professionals to comply with the law in their countries. It is a good idea to have a copy of these guidelines in the x-ray room for training and reference purposes. The main points are detailed below.
The Radiation Protection Advisor and Radiation Protection Supervisor
The Radiation Protection Advisor (RPA) is a professional with detailed knowledge of radiation physics and the practical application of this to working practice. The RPA is first consulted at the planning stage of constructing a workplace with x-ray facilities, and provides advice on how to comply with the relevant regulations. The RPA also helps to draft local rules which detail how radiation should be properly used in each particular instance. In the individual workplace a Radiation Protection Supervisor (RPS) should also be appointed. This person's role is to ensure that the local rules are properly adhered to, and that any radiation-related incidents are reported to the RPA for investigation (British Veterinary Association, 2002).
Justification
One of the most important principles of radiation protection is justification. This means that under no circumstances should radiography be performed without proper justification of the procedure. All requests for radiography should come from a qualified professional who, with consideration of the clinical history, judges it necessary for diagnosis. If the procedure cannot be properly justified then it does not need to be performed, and this reduces the risk from ionising radiation to zero. In practical terms, any requests for radiography that do not make sense from a clinical perspective should be questioned before proceeding.
Working within controlled areas
A controlled area can be defined as an area within which it is necessary to take special precautions to limit exposure to ionising radiation. In buildings it is usually designated by the RPA, taking into account the individual circumstances of each workplace. Controlled areas may be temporary, such as when performing mobile radiography, in which case the area should be properly marked out to prevent entry. Entry to the controlled area should be strictly controlled. To help with this, warning signs must be placed at the entrance, and wherever possible the door should be locked to prevent the accidental entrance of staff when an exposure is being taken. A simple shout of ‘x-ray!’ is also useful to make sure no one is present in the controlled area just before making an exposure.
There are some instances where it is not possible for staff to exit the controlled area for radiographic procedures. These may include fluoroscopy, equine extremity radiography, taking manually inflated thoracic radiographs and performing retrograde cystourethrograms. Sometimes this could possibly include manual restraint of a patient. An important consideration at this point is to make sure that only the bare minimum number of essential staff should be present. Others should exit the controlled area until it is safe to return. Any people present in the controlled area during radiography should be wearing protective clothing (i.e. a lead gown and thyroid shield) and a monitoring badge. Ideally a protective screen should also be used as this reduces exposure by a large factor, and staff should stand as far away from the patient and x-ray beam as possible. A log of people present in the controlled area should be kept in case of any incident or incident involving radiation occurs. The monitoring badges of these people can then be checked to calculate potential dose received.
The BVA guidance (2002) states that manual restraint of animals during radiography should be avoided wherever possible. This means that patients should not be held unless there is a clinical reason why they cannot be restrained by other means (e.g. chemical sedation or physical immobilisation with sandbags). Staff holding a patient should be properly trained to perform this task, and should be wearing lead gloves in addition to the measures mentioned above. Under no circumstances should any human body part be included within the primary beam (Figure 1). In the 1950s it was common to see American veterinary surgeons with radiation damage to their hands from x-ray use, largely due to ignorance regarding radiation hazards (Schnelle, 1968). Interestingly, by the late 1960s it was rare to see human hands on radiographs, probably due to a proactive awareness campaign regarding radiation safety (Schnelle, 1968). Unfortunately, in some countries outside of Great Britain it is clear that manual restraint is still commonplace for small animal radiography, and consideration of safety aspects is sometimes lacking. Reasons for this may include increased cost, time and risk associated with sedation.

As low as reasonably practicable (ALARP)
The ALARP principle should govern all use of radiation. In short, exposures should be kept as low as reasonably practicable to get the diagnostic information required, and the minimum number of radiographs should be taken. This principle is designed to help keep exposures to staff and patients to a minimum. In practical terms this means that individual exposure factors (i.e. mAs and kVp) should not be too high for each particular procedure. Plain film radiography has a built-in protective measure to stop the user from regularly using exposures which are too high — this comes in the form of an overexposed undiagnostic film. Although there are a great number of advantages to digital radiography, one problem is that up to a certain point unnecessarily high exposures do not result in poor quality images (Baker, 2012). With this is mind it can be seen that using higher exposures than needed will result in increased patient dose, increased scatter, and increased staff doses. The standard method for checking exposures in digital radiography is the Exposure Index, which is a numerical value indicating the suitability of the exposure used (Baker, 2012). Keeping a log of exposures and using an exposure chart are valuable ways of keeping a check that exposures are not gradually increasing over time, a phenomenon called exposure creep (Gibson and Davidson, 2012).
Complying with the ALARP principle also means that care should be taken to avoid repeating radiographic procedures due to poor technique. It is therefore crucial that proper training is given in radiography in order to ensure the best working practice. As well as proper positioning, care should be taken to ensure proper sedation and/or immobilisation of the patient. Images must also be processed with the best technique available as this will avoid the need for repeats due to poor quality images. In other words, becoming good at radiography means that fewer exposures will be needed!
The term ‘collimation’ refers to restriction of the x-ray beam so that only the area of interest is exposed. This is achieved by dials on the x-ray unit which shutter off the main beam. Some units may instead use screw-on cylinders, sometimes called ‘cones’, which limit the beam to a fixed circular area. Good collimation is essential because it reduces the amount of radiation the patient is exposed to, thereby increasing patient safety. In addition, it reduces the amount of scattered radiation produced, which constitutes the main source of radiation exposure for staff (Brateman, 1999).
Although use of a grid greatly reduces scattered radiation reaching the film or imaging plate, it does not prevent it from reaching staff members or indeed other parts of the patient itself. Importantly, when a grid is used the exposure must be significantly increased in order to achieve a good quality image. This in turn increases patient exposure and where applicable, staff exposure too. It is therefore essential to only use a grid when absolutely necessary — usually where a body part exceeds 10 cm in depth.
Key Points
- Exposures should be kept as low as reasonably practicable (ALARP).
- There is no safe level of exposure to ionising radiation.
Protective clothing, shields and equipment
Scattered radiation is produced when the primary beam interacts with matter — usually the patient or equipment next to the patient. Protective clothing is designed to protect against scattered radiation only as it is easier to attenuate or stop than the primary beam (Brateman, 1999). Historically, protective clothing has come in the form of lead-lined gowns, thyroid shields and gloves. The effectiveness of protective clothing and equipment is graded according to its equivalent thickness of lead, with 0.25 mm, 0.35 mm or 0.5 mm options being the most commonly available. Body parts that are not covered in this way may receive up to 20 times the dose of covered areas (Hricak et al, 2011). Although a thicker layer of lead gives better protection, it is also heavier. There are different ways of dealing with this, usually by wearing a special belt which transfers some of the weight to the hips, or by a tunic and skirt combination. Lead-free protective gowns and clothing are now gaining in popularity due to their lighter weight and safety concerns regarding lead. Some gowns have a cross-over design which gives more protection at the front. It is important to hang protective clothing properly when not in use as this reduces the risk of it developing cracks. Indeed, this kind of equipment should be tested regularly to ensure that the protective layer has not become damaged, making it less effective (Ionising Radiations Regulations, 1999).
Leaded glasses are useful to protect the eyes and face, and arm, leg and head protectors are also available. Gloves and thyroid shields should have a minimum lead equivalent of 0.5 mm. There are a range of sterile surgical-style gloves which provide a lesser degree of shielding against x-rays. While these are designed for surgeons where scattered radiation dose to the hands may present a problem, they are not designed to be placed within the primary beam. Simple actions such as standing behind a lead-lined screen can greatly reduce radiation exposure. There is a large range of protective screens available, either wall-mounted or on wheels. Some of these are completely transparent, allowing better participation and observation.
Distance
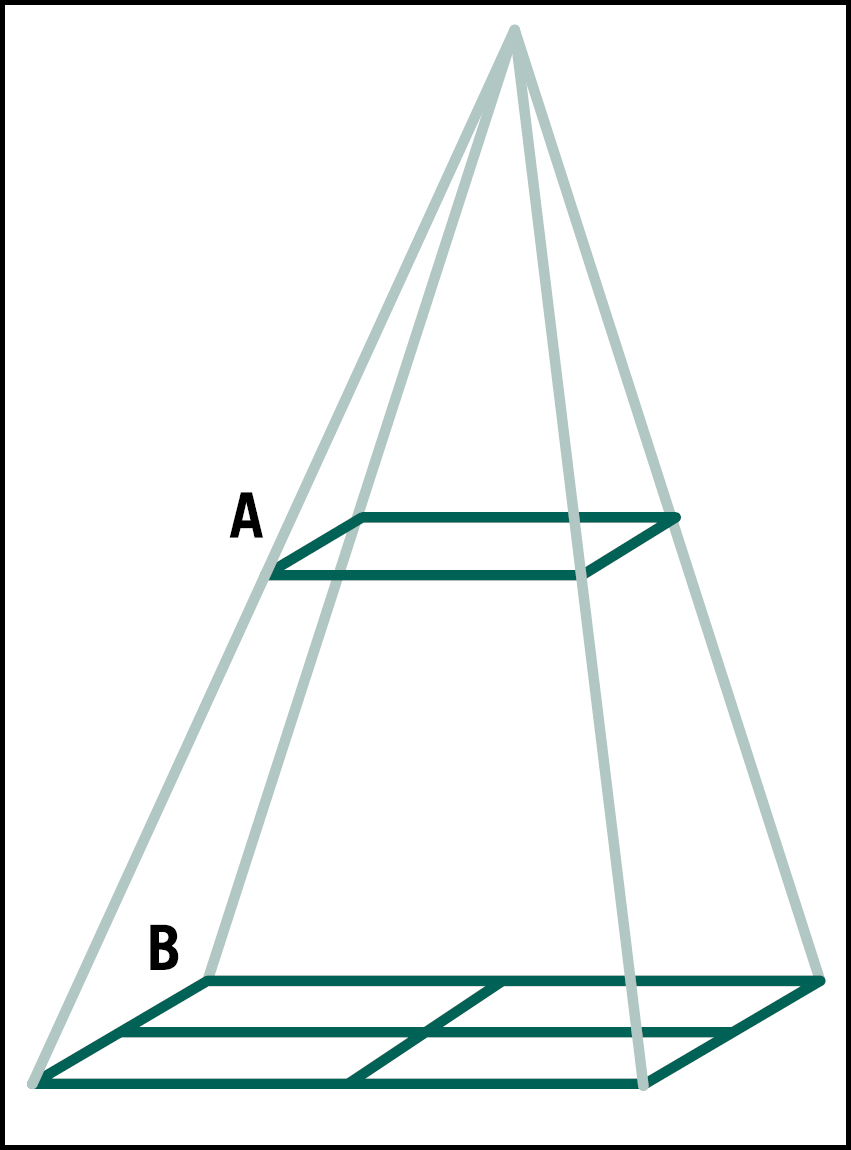
The relationship between distance and exposure is governed by the inverse square law. Simply put, doubling the distance from a radiation source will reduce the intensity or exposure to ¼ of its previous value (Figure 2). If a veterinary professional is required to be present in the controlled area during a radiographic procedure, the further away from the radiation source they can be the better it will be for their safety. For equine extremity radiography the use of a pole with a cassette holder at the end will allow the practitioner to keep as far away as possible from the primary beam in many cases.
Monitoring badges
Monitoring badges are a good way of checking that veterinary personnel are working safely with radiation, and help demonstrate that the annual dose levels for staff are not being exceeded. These badges range from film badges to thermoluminescent dosimeters (TLDs), to electronic personal dosimeters (EPDs). The first two are normally renewed every 2 months or so, and the recorded dose is used to give an indication of how much radiation and what kind of radiation exposure occurred. Although more expensive, electronic dosemeters can give an immediate reading and so may be more useful. Monitoring badges should be worn on the trunk when performing radiography, and should be positioned under the lead gown if it is used. Additional badges may be worn on the wrist or finger, and these are usually used for theatre procedures or for fluoroscopy. It is important that each badge is looked after so that it can give an accurate reading. For example, some are heat sensitive and should not be left in the sun, on a radiator or put in a tumble dryer. It also goes without saying that they should not be left in the x-ray room! In workplaces where the employer can demonstrate that the dose to personnel does not exceed a given level per year, it may not be necessary to use radiation monitoring badges.
Pregnancy
It is well documented that ionising radiation presents a particular risk to the fetus. If a veterinary professional is pregnant or thinks they may be pregnant, it is their duty to inform their employer. In order to comply with the Health and Safety Act (1974) the employer must have carried out a risk assessment to take into consideration safety of pregnant staff in the work place with respect to radiation safety and pregnancy. The Ionising Radiations Regulations (1999) state that once the employer has been informed of pregnancy it is their duty to ensure that the dose to the fetus does not exceed 1 mSv for the remainder of the pregnancy. A possible outcome could be that the employer allocates pregnant veterinary personnel different duties for the remainder of their pregnancy.
Conclusion
There are many techniques which can be employed to reduce the risk from ionising radiation to staff and patients. Becoming proficient at radiography is also imperative as it reduces the number of exposures required and often the amount of radiation used per examination. Proper training and awareness of the potential risks are therefore essential for the veterinary nurse in order to work safely with x-ray equipment.

