Burn injuries have a reputation for being extremely traumatic, and in human medicine often result in high morbidity and mortality rates (Sheridan, 2018). The definition of a burn is generally described as damage to the two main skin layers which has been caused by extremes in temperature or by contact of caustic substances, electricity or radiation (Pope, 2009). When tissue is burned it involves direct coagulation and microvascular reactions which can cause the injury to spread into the surrounding dermal layers.
This is known as the iceberg effect, where on initial presentation the wound may only appear to cover a small surface area, however if left untreated these microvascular thermal reactions continue and cause further devitalisation of the surrounding tissue (Sheridan, 2018). The severity of these injuries can depend on the aetiology and extent of the burn - larger burn injuries where there is a significant loss of the skin barrier and release of wound mediators are associated with a systemic response that can lead to sub-sequent infections (Sheridan, 2018). These factors along with the patient's age, body condition or any other pre-existing medical conditions can significantly alter the management plan and overall outcome for the patient. Severe burn cases require a systematic wound management plan that maps initial stabilisation and long-term care (Vigani and Culler, 2017). The initial aims when managing a burn patient should include minimising the thermal damage by cooling the area and/or removing any chemical substances, ensuring adequate analgesia, preventing contamination and infection, removal of devitalised tissue and reconstruction options (Niles, 2009). This article aims to look at the common types of burns typically seen in practice and the treatment methods available. It will cover stabilisation of the emergency burn patient, and the wound management options available for burn wounds.
Classification, causation and evaluation
Before creating a wound management plan, it is important to establish what caused the burn - for instance the initial stabilisation and treatment of a thermal burn may differ to that of an electrical burn. When exposure to electricity occurs the current will take the path of least resistance which can cause damage to major internal structures, generally this can lead to moderate to severe pulmonary oedema, ventricular fibrillations and in cases of high voltage electricity exposure cardiopulmonary arrest, so care would need to be taken to ensure a thorough examination before initiating fluid and drug therapies to rule out major cardiac and respiratory system involvement (Pavletic, 2018). Following this, the extent of the burn needs to be evaluated, by establishing the total body surface area affected as well as the burn depth. Once the aetiology and extent has been determined the overall wound management plan should be considered. This should involve not just how the wound will be managed, but also supportive treatment (Vigani and Culler, 2017). Severe burn patients may require intensive care that involves advanced nutritional management, aggressive fluid therapy, monitoring electrolyte imbalances, managing anaemia and maintaining organ function. It may also be necessary in patients exposed to house fires to treat life-threatening injuries, such as smoke inhalation or carbon monoxide poisoning before initiating wound management (Tello, 2013).
Classification
The traditional human medical classification system of burns divide these injuries into first, second- and third-degree terms, however the veterinary profession has adopted another system, determined by the layers of skin affected by a burn injury (Tello, 2013). These classifications are discussed in Table 1.
Table 1. Burn classification (Vaughan et al, 2012)
| Burn thickness | Burn depth and characteristics | Healing |
|---|---|---|
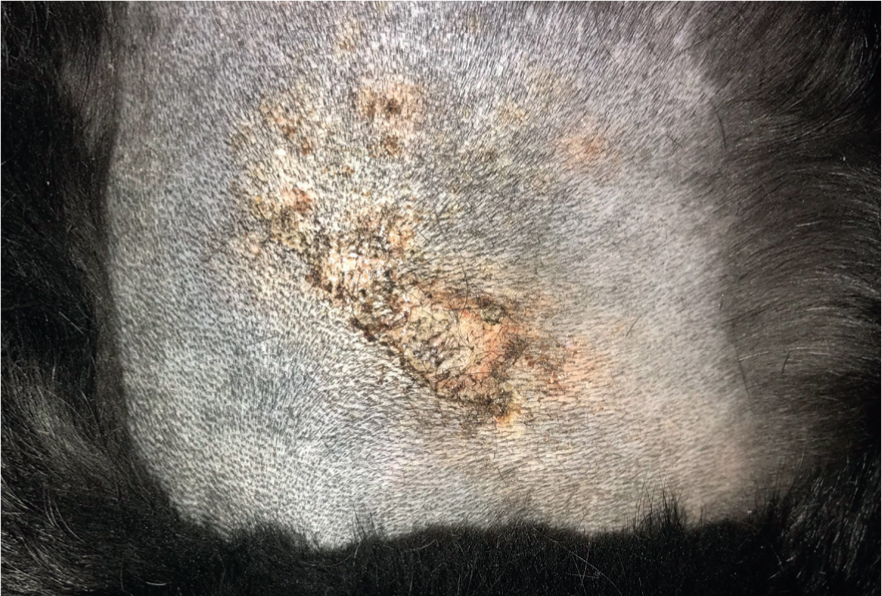
| Superficial | Only affects the epidermis.Signs:
|
Heal by re-epithelialisation within 3–5 days with minimal to no scarring (Figure 1) |
| Superficial partial thickness | Involves the epidermis and superficial layer (1/3) of the dermis or papillary layer Signs:
|
Should heal within 1–2 weeks with some scar formation |
| Deep partial thickness | Epidermis and all layers of the dermis Signs:
|
Should heal in 2–3 weeks, may require surgical intervention to aid in healing and prevent poor scar tissue formation |
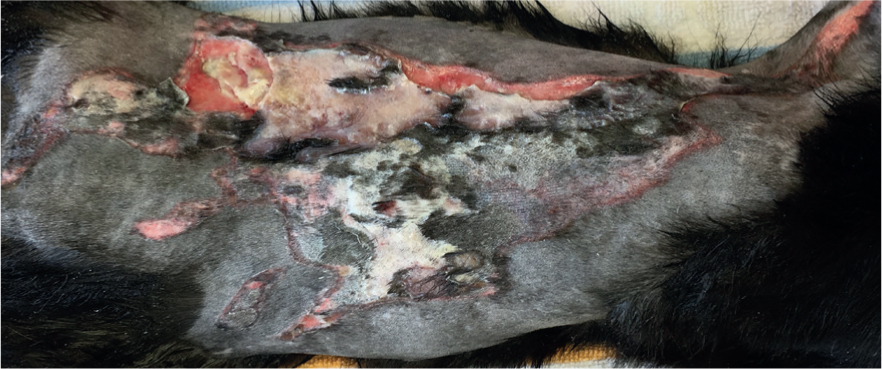
| Full thickness | Involves the epidermis, dermis and into subcutaneous tissue Signs:
|
Do not generally heal by second intention, require surgical intervention to minimise scarring and impaired function (Figure 2) |
Thermal
Thermal injuries are classified as either dry or wet burns. Dry burns are caused when the patient is unaware or unable to move away from a heat source; such as a recumbent or anaesthetised patient in contact with a heat pad or cats found sleeping inside car engines (Figure 3) (Pope, 2009). Wet burns are caused by contact with hot liquids or ignited flammable solutions. Typically, patients with a dorsal pattern have had a liquid dropped onto them or thrown over them in passing (Figure 4) (Pope, 2009). Ventral burns are associated with the patient being lowered or jumping into hot liquid (Figure 5). Deliberate ignition with application of a flammable liquid has been described in cruelty cases but is not common place in general practice, most burn wounds are more accidental in nature (Pope, 2009).



The severity of a thermal burn is dependent on the temperature of the heat source and contact time. There are a few other factors to consider, including where the heating aid has been applied; skin with less fur or wet fur can facilitate heat transfer to the skin surface, and weight-bearing areas where perfusion may be compromised preventing heat from being removed from the area (Veterinary Practitioner's Board (VPB), 2016). For example, when looking at contact time and temperature it has been reported that 45°C warming can lead to a burn after 90 minues whereas 50°C warming can lead to burn after just 10 minutes of contact time (VPB, 2016).
Chemical
Chemical burns can be caused by acidic or alkaline solutions, and these may present as skin wounds or as damage to the oropharynx and oesophagus if ingested (Figure 6) (Pope, 2009). Acidic solutions will generally cause pain on ingestion or application leading to decreased exposure time and quicker presentation to the practice (Pope, 2009). In contrast, alkaline solutions will not usually cause pain, and so exposure times may be prolonged due to the slower onset of symptoms and this ensuing delay in presentation can lead to a more severe burn wound (Pope, 2009).

Electrical
Electrical burns are generally caused by the chewing of electrical wires or by exposure to bare wiring, and this is more commonly noted in paediatric patients (Pope, 2009). Burns from extremely high voltage sources, such as exposure to railway lines or lightening, are rare.
Radiation
Generally, the least common presentation, however as an increasing number of practices now offer oncological treatments there may be increased numbers of patients as a result. Radiation burns are typically a result of exposure to doses 40 gy and above (Pope, 2009). The severity of the injury is dependent on the area affected as different tissues have differing tolerance levels to radiation injury (Pope, 2009).
Evaluation
Full evaluation of a burn wound is crucial, and it is important to establish both the aetiology and the extent of the injury. This is important as it can help to build a good management plan and may help to manage client expectations of a successful outcome, and inform the client of the potential financial costs. The extent of a burn wound is expressed as the percentage of the total body surface area (TBSA) affected. The available models are taken from human medicine and have proven difficult to adapt to veterinary medicine (Vigani and Culler, 2017). The ‘Lund-Browder Chart’ (http://www.vicburns.org.au/burn-assessment-overview/burn-tbsa/lund-browder) is a popular model which involves drawing the burn onto a figure and using an age-specific table to calculate the percentage of the patient's body affected. This model can be applied to veterinary medicine (Vigani and Culler, 2017), however it faces limitations when applied to animals. ‘The rule of nines’ is an alternative method used for human adult burn patients which involves separating the body into sections that represent 9% of the body's surface area (Table 2) (Sheridan, 2018). This model has proven to be inaccurate in veterinary patients due to the variation in size and weight between animals, and due to most animals having an excess of elastic redundant skin which tends to lead to an over estimation of the affected area (Langley-Hobbs and Pead, 2018). Despite these limitations, until a veterinary specific model is established using human guidelines as a rough estimate can prove helpful.
Table 2. ‘Rule of nines’
| Section of body | Percentage of body surface area |
|---|---|
| Head and neck | 9% |
| Each forelimb | 9% |
| Each hindlimb | 18% |
| Thorax | 18% |
| Abdomen | 18% |
(ISFM, https://icatcare.org/vets/practice-resources/considerations-burns-patients)
Emergency stabilisation and considerations
It is important that stabilisation occurs before or alongside any wound management when treating any emergency patient. If the presenting patient is stable, then treatment of the wound can commence immediately. Arguably, the only wound treatment that may be deemed appropriate at the initial stages of presentation of the burn patient would be lavage (Vigani and Culler, 2017). One of the main aims when treating a burn wound is to try and prevent further micro-vascular damage by attempting to remove the thermal aspect of the burn (Niles, 2009). Lavage at the early stages could potentially reduce further spread of the coagulation zone, help to reduce oedema locally, improve pain control and remove potentially caustic materials (Vigani and Culler, 2017). Thorough wound lavage technique will be discussed in more depth in the next section, but for emergency situations the currently recommended guidelines are to cool the area with running tap water at approximately 12°C or room temperature saline for 15–30 minutes (Vigani and Culler, 2017). It is important not to use cold water or ice as there is a potential for vasoconstriction, hypothermia and exacerbation of injury (Vigani and Culler, 2017). The goal with initial lavage is to cool the burn and not the patient so temperature should be carefully monitored.
If the burn injuries are a result of a house fire, then the patient should be assessed for smoke inhalation injuries as these could be more life threatening than most burn wounds. The airway should be checked for any localised oedema and maintained if needed (Pope, 2009). Intubation may be warranted but in certain cases emergency tracheostomy tube placement may be more appropriate. At a minimum, supplemental oxygen should be provided, this can be done using nasal prongs or nasal catheters (Pope, 2009). Patients should be continually monitored for signs of inhalation injury; respiratory rate, repeated chest auscultation, pulse oximetry and blood gas analysis could prove beneficial in early detection of any complications (Pope, 2009).
Appropriate analgesia should be administered, and continually adjusted as needed based on regular pain scores and patient demeanour (International Cat Care (ICC), 2019). It has been reported that human burn patients experience varying degrees of pain throughout the duration of treatment, with descriptions of pain worsening over time despite aggressive analgesic techniques (Vigani and culler, 2017). Full mu opioids, such as methadone or fentanyl, can be used if available either via constant rate infusions or bolus doses, although most literature recommends the use of constant rate infusions to maintain a near-constant plasma level and efficient control of background pain (Vigani and Culler, 2017). Non opioid analgesics, such as NDMA receptor antagonists and alpha 2 agonists have been shown to offer effective analgesia and sedative effects for burn patients (Vigani and Culler, 2017). Ketamine, an NDMA receptor antagonist, has over recent years has been utilised in human burn patients as a low dose constant rate infusion to control ‘wind-up’ pain and as part of procedural sedation protocols for dressing changes (McGuiness, 2011). The use of corticosteroids likely do not aid patient recovery, and non-steroidal anti-inflammatories should be avoided until the patient is deemed haemodynamically stable, as these can lead to renal impairment (Vigani and Culler, 2017).
Fluid therapy is an integral part of managing the severe burn patient. In moderate to severe burns increased capillary permeability and myocardial depression causes a mass fluid shift and secondary depletion of intravascular volume, which can lead to burn shock during the initial 24–48 hours after presentation (Vigani and Culler, 2017). The increased capillary permeability also causes mild to severe oedema and depending on the extent of the oedema it can be either localised or generalised, this factor is based on the percentage of TBSA affected (Pope, 2009). The maximum leakage occurs within the first 8 hours following injury and should gradually decrease over 48–72 hours until the patient's body creates enough fluid to compensate. In some patients, aggressive fluid therapy may be required, and balanced isotonic solutions should be chosen over isotonic saline solutions in order to reduce the incidence of hyperchloraemic acidosis. The efficacy of hypertonic saline and colloids are disputed and were found to have no improvement on survival rates. Incremental fluid boluses can be used initially until blood pressure, heart rate, and pulse quality is normalised, and signs of hypovolaemic shock are corrected. Care should be taken not to cause hypervolaemia in these patients; they may require large volumes of fluid during the initial stages, but overload can lead to worsening of oedema, intra-abdominal hypertension and compartment syndrome (Vigani and Culler, 2017). To ensure fluid therapy is tailored appropriately to the patient they should be weighed regularly, urine output and specific gravity monitored, with urine output kept at a minimum of 1–2 ml/kg/hour, along with continual monitoring of all the vital parameters (Vigani and Culler, 2017).
It is important to rule out any other underlying issues that may affect wound healing and the management of the patient. Packed cell volume (PCV) and total solids should be checked and monitored. Burn patients can present with mild to moderate anaemia - this is due to several mechanisms, one of which is the thermal destruction of red blood cells followed by physiological lysis of cells several hours later (Pope, 2009). Where appropriate, haematocrit levels should be maintained using whole blood or packed red blood cell transfusions and supplemental oxygen therapy until the patient is able to maintain a steady haematocrit level of 25% and above (Pope, 2009). Electrolyte imbalances are common, serum potassium should be monitored and maintained using supplementation as necessary (Vigani and Culler, 2017). In the long term these patients will require intensive nursing care which should include a nutrition plan, mobilisation and/or physiotherapy, and monitoring for any gastrointestinal complications (ICC, 2019).
Wound examination and considerations
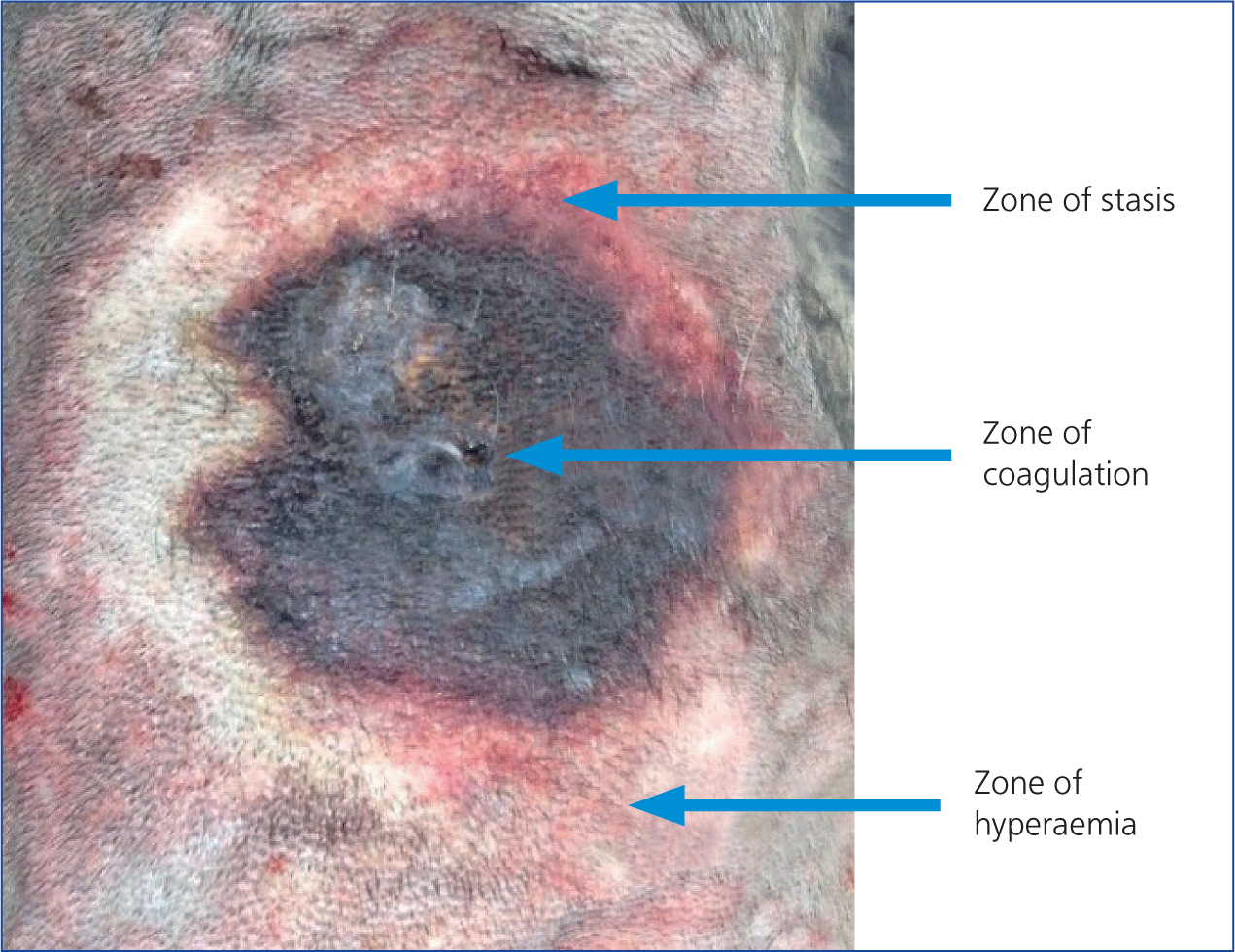
The severity of the burn wound will dictate how invasive the wound management plan needs to be. When considering the wound management plan it can be useful to refer to the ‘Jackson burn wound model’ (Figure 7) (Douglas and Wood, 2017). The inner part of the burn wound is referred to as the zone of coagulation, this inner zone is considered non-vital and no treatment will change this (Douglas and Wood, 2017). The outer zone is referred to as the zone of hyperaemia, this area of reactive tissue is a result of the body's inflammatory response, this response will usually settle with minimal treatment over a few days (Douglas and Wood, 2017). The middle zone is the zone of stasis, where the use of dressings will help to prevent further deterioration of tissue status, and if left untreated it risks becoming part of the coagulation zone and will no longer be viable tissue (Douglas and Wood, 2017). With most small partial-thickness burns and superficial burns often second intention moist wound management will be enough (Jenkins, 2018). Some small full thickness burns could also be managed via second intention healing, but scar formation and contracture could potentially cause issues (Jenkins, 2018). Most full thickness burns, especially those with a high TBSA percentage, will require surgical intervention to ensure minimal scarring and a return of normal function (Jenkins, 2018).
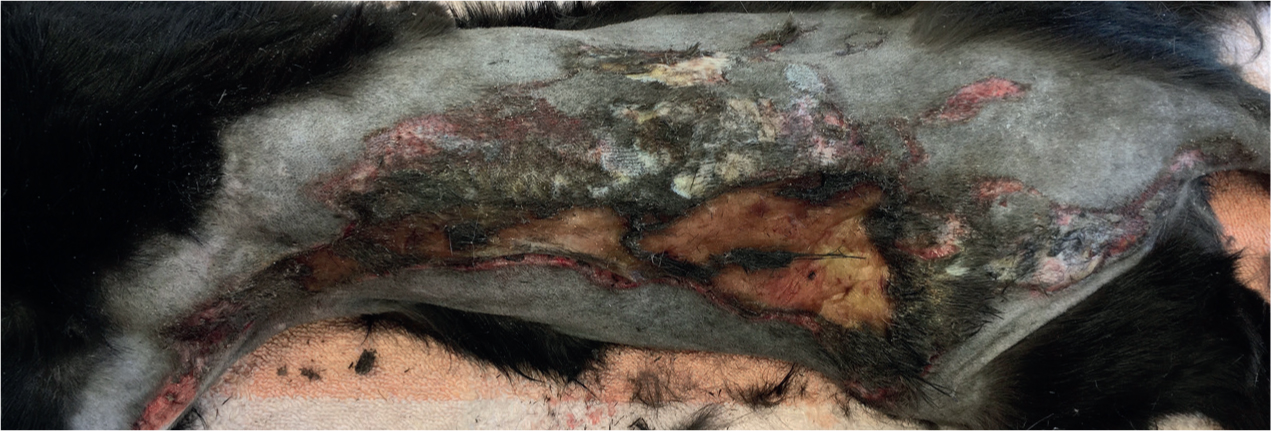
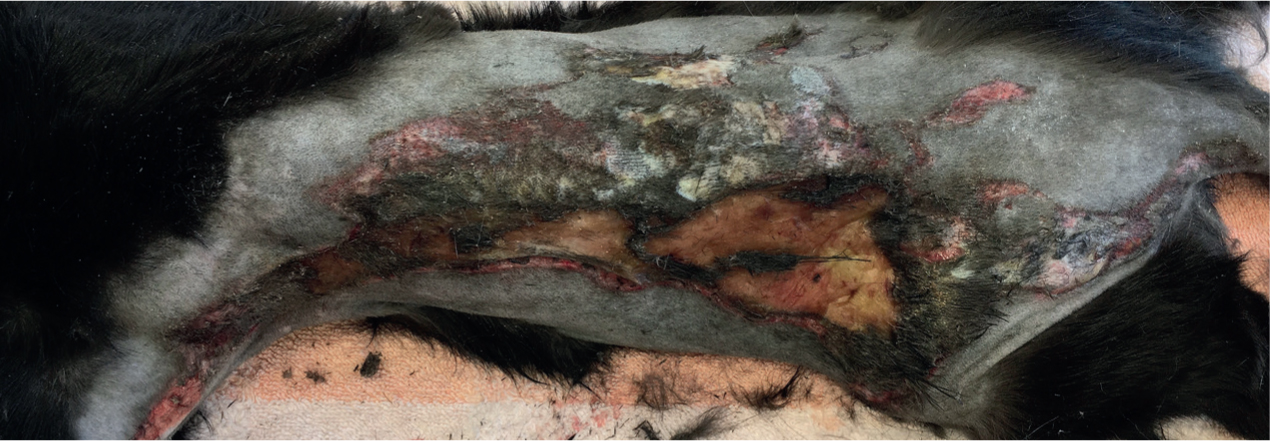
A wide area should be carefully clipped to allow for full visualisation of the wound and surrounding tissue. In full thickness burns the hair will pluck out easily so when clipping care must be taken not to cause further damage to already delicate tissue (Langley-Hobbs and Pead, 2018). Burn injuries can change appearance over 48-72 hours, initially areas of red or inflamed skin may be noted so having good visualisation of the surrounding tissue can help to monitor wound progression and eventually help assess the full extent of the injury (Figures 8 and 9) (Langley-Hobbs and Pead, 2018).

Lavage is an important aspect of burn wound management, it can provide a form of debridement by helping to remove debris and help prevent burn progression (Roosje, 2018). Recommended equipment for lavage includes a 1 litre bag of warm isotonic solution, attached to a giving set or extension set then connected to a three-way-tap, 35 ml syringe and 18 g needle (O'Dwyer, 2012). This should provide the correct pressure of approximately 4–15 psi, to ensure debris is removed and that bacteria are not driven deeper into the tissue (Swezey, 2014). Lavage should be continued until all debris is removed, and it is recommended to use a rule of 100 ml per 1 cm of wound (Hollis, 2018). The efficacy of antiseptic solutions is disputed, and in heavily contaminated wounds chlorhexidine or iodine can be used if appropriately diluted but have been reported to cause damage to fibroblasts and to inhibit wound healing, and so care should be taken not to over use these solutions (O'Dwyer, 2012).
Aseptic technique is vital when handling burn patients, and good hand hygiene, use of personal protective equipment and sterile gloves and equipment should be used when directly handling the tissue to prevent contamination (O'Dwyer, 2012). Burn patients are at high risk of developing sepsis, but the use of prophylactic antibiotics is disputed, and ideally the patient should be monitored closely for early signs of a systemic inflammatory response and if infection is suspected this should be confirmed using culture and sensitivity before utilising systemic antibiotics (Pope, 2009). Topical antimicrobials for initial wound dressings may also be used to help prevent a systemic response developing from the wound bed (Figure 10) (Hollis, 2018).

For partial to full thickness wounds more invasive debridement is usually required. It is typical to see eschar (thick, leathery, necrotic tissue) formation in most burn wounds (Figure 11) (Jenkins, 2018). These eschars can lead to potential complications if not removed; when formed over the thorax they can restrict breathing and could lead to vascular compromise and reperfusion injuries if covering a limb circumferentially (Pope, 2009). Sharp surgical debridement may be the most appropriate method, and the technique used is usually dependant on whether there is muscle/bone involvement. With deep burns that do not involve muscle or bone, tangential debridement is used to slice off the affected tissue in thin layers until viable tissue is reached (Jenkins, 2018). With deep burns that extend into muscle and/or bone layered debridement would be more appropriate, a method which involves starting at the perimeter of the wound where the tissue damage is more superficial and carefully removing devitalised tissue, progressing inward to debride the deeper layers and taking care not to damage any vital tissue (Jenkins, 2018).
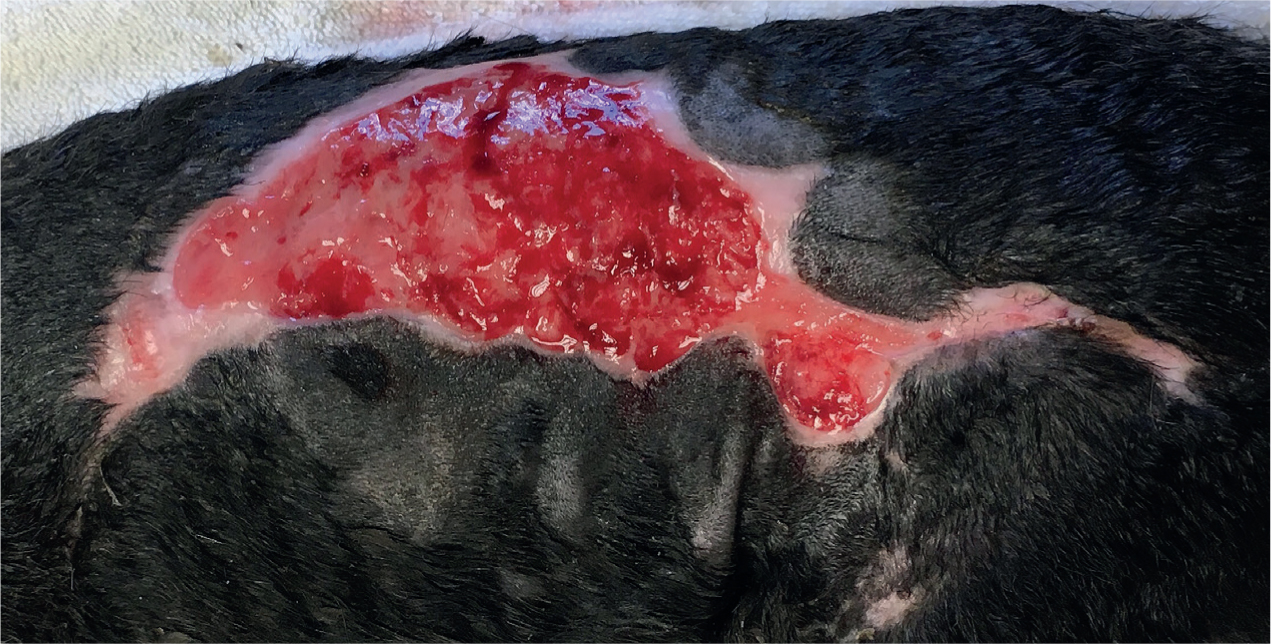
Care should be taken when deciding how much tissue to debride. As previously mentioned the full extent of the injury may take a few days to present and as such it is advisable to carry out staged debridement to ensure viable tissue is not removed (Figure 12). For that reason, the application of topical treatments and wound dressings that assist with autolytic debridement might be a more appropriate option (Jenkins, 2018). A summary of the available dressings, including their advantages and disadvantages are outlined in Table 3. Another option to consider for larger wounds that involve a deep tissue deficit would be negative pressure wound therapy, the aim of which is to remove exudate, decrease interstitial oedema, promote circulation and help to stimulate cells involved in modulating the body's inflammatory and proliferation response (Stanley, 2017). There is limited evidence as to whether negative pressure wound therapy when used with integrated dressings on large partial-thickness to full thickness burn wounds has any benefit on revascularisation or not (Kantak, 2016), and further research is needed into the effect this therapy has on burn healing (Dumville et al, 2014).
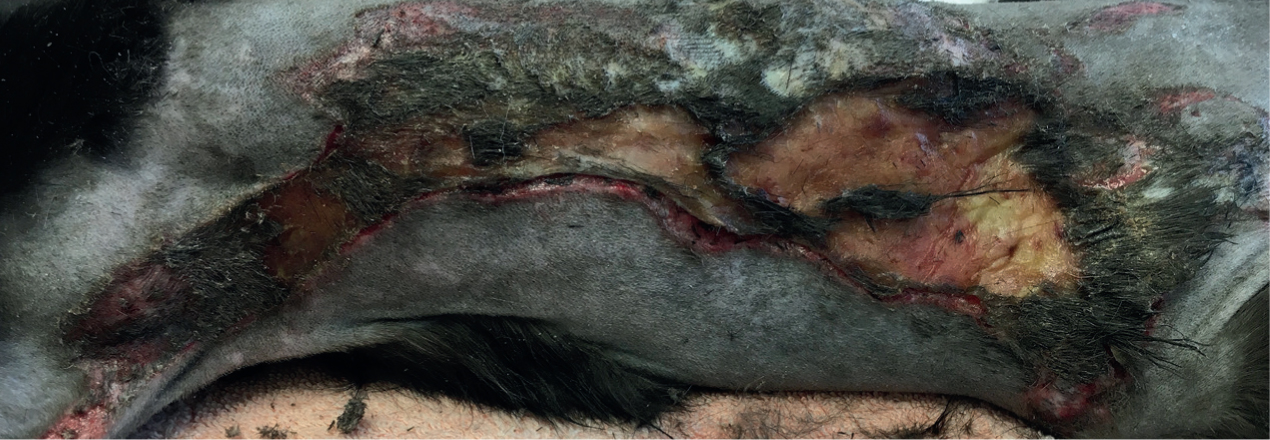
Table 3. Products available for burn wounds
| Product | Advantages | Disadvantages |
|---|---|---|
| Medical grade manuka honey - sterilised honey availablefor topical application or as an impregnated dressing |
|
|
| Silver sulfadiazine - available as topical application or as a combined impregnated dressing |
|
|
| Hydrogels - complex hydrophilic organic cross-linked polymer, 80–90% water based. Can be free flowing or impregnated dressing |
|
|
| Hydrocolloids - self-adhesive, gel-forming dressings composed of hydrophilic colloid particles |
|
|
| Negative pressure wound therapy - specialised equipment is used to apply sub atmospheric pressure to the wound bed via a dressing or sponge |
|
|
(MRSA, meticillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant enterococci)
Once a healthy granulation bed has been established, reconstruction surgery can be considered or in areas where contracture and scar formation are not an issue continual moist wound management via second intention healing could be a viable option (Figure 13).
Conclusion
When presented with a severe burn wound there are a wider variety of factors to consider than just the wound itself. Burn injuries pose an assortment of challenges for all the veterinary team, but for nurses these patients require utilisation of a variety of skills and knowledge. Having a comprehensive understanding of how the burns patient may differ to that of a traumatic wound injury can help us to appreciate how these cases are so much more complex than typical wounds and will hopefully help in improving outcomes for these patients.
KEY POINTS
- Burn injuries can be extremely traumatic and can present a variety of challenges that require use of various nursing skills, such as wound management, nutritional support, monitoring of vital body systems and infection control.
- Burn patients are at high risk of developing sepsis, and when handling these patients aseptic techniques should be adhered to and the patient should be monitored for signs of any systemic inflammatory response.
- Deep or large burn wounds generally need to be managed by delayed primary closure, these wounds can develop over a few days, so topical antimicrobials may be useful in the early stages to help with debridement and formation of granulation tissue ready for reconstruction.
- Fluid therapy is one of the most important aspects of managing the burn patient. Aggressive fluid therapy may be required to help prevent burn shock, but care needs to be taken to not fluid overload these patients.
- Adequate multimodal analgesia should be used in burn patients, pain levels can vary throughout the course of treatment so approved pain scoring systems should be used to monitor pain levels.


