Blood is a fluid that transports nutrients, oxygen and waste products to and from cells. It is also involved in defence and wound repair. Blood contains red blood cells, various types of white blood cells and platelets suspended in plasma. The red col-our of vertebrate blood is due to haemoglobin, a protein in red blood cells, that is responsible for oxygen transport. Various poisons can affect the blood and produce a variety of biochemical changes and clinical signs. This article will discuss some substances that commonly cause adverse effects on the blood in companion animals.
Anaemia
Anaemia is a reduced number of red blood cells or haemoglobin in the blood and there are three main causes, blood loss (from trauma, for example), decreased red blood cell production or increased red blood cell breakdown. There is constant production of new, and removal of aged, red blood cells from the circulation. The normal lifespan of red blood cells is 110–120 days in dogs and 65–76 days in cats. It is also important that red blood cells are able to deform and squeeze through narrow capillaries. If they are damaged in some way and unable to deform, they will be removed from the circulation by the recticuloendothelial system (Lincoln et al, 1992).
Haemolytic anaemia
Haemolytic anaemia is a form of anaemia that occurs as a result of haemolysis, the abnormal breakdown of red blood cells. This can occur either in the blood vessels (intravascular haemolysis) or elsewhere in the body (extravascular, but usually in the spleen).
A number of substances can cause anaemia (Box 1). Zinc toxicosis in dogs results in severe intravascular haemolysis and haemolytic anaemia (Meurs et al, 1991). Zinc is available in many forms, but most cases of poisoning in domestic animals are due to ingestion of zinc-containing foreign bodies, particularly coins (£1 and £2 coin, 1 and 2 Euro coins but most cases reported involve US 1 cent coins), and nut or bolts. Many nappy rash creams contain zinc oxide but these are only likely to be a concern if there is chronic exposure (e.g. applied to the skin repeatedly and licked off).
Box 1.Some potential toxicological causes of haemolytic or Heinz body anaemia
- Allium species (onions, leeks, garlic, spring onions)
- Recluse spider (Loxosceles species)
- Copper
- Naphthalene (some mothballs)
- Propylene glycol
- Zinc
The mechanism of haemolysis in zinc toxicosis is unclear; it is not immune-mediated and may be due to inhibition of red blood cell enzymes, direct damage to the red blood cell membrane, or increased susceptibility of red blood cells to oxidative damage (Breitschwerdt et al, 1986).
Clinical signs of zinc poisoning
Zinc poisoning in dogs is characterised by gastrointestinal signs followed by a haemolytic crisis. Initial signs include vomiting, sometimes haematemesis (Mikszewski et al, 2003), diarrhoea (which can be haemorrhagic), anorexia, pyrexia and depression. Gastrointestinal ulceration, haemorrhage and melaena may also occur with zinc (Breitschwerdt et al, 1986; Mikszewski et al, 2003; Lee et al, 2016).
Haemolytic anaemia with haemoglobinuria then develops, usually within a few days of ingestion. Signs of anaemia include tachycardia with a weak or bounding pulse, heart murmur, severe weakness and dyspnoea.
In severe cases, there may be pancreatitis, disseminated intravascular coagulation (DIC), and renal and liver dysfunction (Breitschwerdt et al, 1986; Meurs et al, 1991; Mikszewski et al, 2003; Weingart and Kohn, 2009; Sharkey, 2010). Death typically results from multi-organ failure.
Proteinuria, haemoglobinuria and/or bilirubinuria are common in dogs with zinc toxicosis. Other findings are glucosuria, elevated liver enzymes, bilirubin, lipase and amylase. Azotaemia is common and coagulopathy with prolonged activated partial thromboplastin time and prothrombin time can occur (Weingart and Kohn, 2009).
Management of zinc poisoning
Treatment of zinc toxicosis is supportive and aimed at controlling the haemolytic crisis and preventing renal, hepatic and pancreatic injury. Numerous household items contain zinc, including medicines and pet items (such as some identity microchips), and it is important to question owners thoroughly about possible sources of zinc exposure in dogs presenting with haemolytic anaemia.
If zinc poisoning is suspected then radiographs should be taken to check for the presence of foreign bodies in the gastrointestinal tract, but the absence of a zinc foreign body does not rule out zinc toxicosis since the source may have been passed or vomited. Any foreign bodies should be removed (surgically or endoscopically) once the animal is stabilised.
In dogs with suspected zinc toxicosis the haematology, electrolytes, renal and liver function, clotting profile, urinalysis, packed cell volume (PCV) and pancreatitis markers should be monitored. If possible, the zinc blood concentration should be measured but results will not be available immediately.
Intravenous fluids are recommended in zinc toxicosis to maintain hydration and urine output in order to protect the kidneys from haemoglobinuric nephrosis. Antiemetics can be used for persistent vomiting. A proton pump inhibitor (e.g. omeprazole) may be given to reduce gastric acidity and reduce zinc absorption (Richardson et al, 2002; Van der Merwe and Tawde, 2009) as an initial treatment until the foreign body can be removed, as the greater the acidity of the stomach the greater the release of absorbable zinc ions. Sucralfate is indicated for management of gastric irritation and ulceration (Medici and Grigsby, 2013). Blood products (packed red cell transfusion or whole blood) are commonly required in animals with clinical signs of zinc-induced anaemia, and plasma transfusions(s) may be required for coagulopathy. Opioid analgesia may be required for pain from pancreatitis (Medici and Grigsby, 2013).
Prognosis of zinc toxicosis depends on the severity of the anaemia and the extent of liver, renal and pancreatic involvement (Richardson et al, 2002; Talcott, 2013). In mild to moderate cases improvement usually occurs 48–72 hours after removal of a zinc foreign body (Peterson, 2016). In more severe cases there may be deterioration following removal (Lee et al, 2016). Prognosis is generally good in dogs that respond to supportive therapy and surgical removal of the foreign body (where applicable), but dogs with complications of zinc toxicosis may require hospitalisation for 2–3 weeks (Mikszewski et al, 2003; Weingart and Kohn, 2009).
Heinz body anaemia
Heinz bodies are inclusions in red blood cells that are formed from damaged haemoglobin. The haemoglobin precipitates, aggregates and binds to the cell membrane and can be seen in red cells when stained for a blood smear. The presence of multiple Heinz bodies attached to the cell membrane makes the red blood cell more rigid and susceptible to fragmentation which shortens its lifespan. Small Heinz bodies are normal in the blood of many healthy cats but their presence in other species is abnormal.
A common cause of damage to haemoglobin is oxidative damage. The haemoglobin in cats is uniquely susceptible to oxidative damage as it possesses eight reactive sulphydryl groups per molecule compared with four in dogs. Oxidative haemolysis occurs when the concentration of oxidants in the red blood cells exceeds the capacity of the antioxidant metabolic pathways. This can occur with onions (Figure 1) and related plants such as garlic, spring onions and leeks. These plants (Allium species) contain a variety of organosulphur compounds and trauma to the plants (such as chewing) converts these compounds to a variety of oxidative compounds but particularly n-propyl disulphide (Fuller and McClintock, 1986; Cooper and Johnson, 1998). Oxidation of haemoglobin results in the formation of sulphaemoglobin which is less soluble than haemoglobin resulting in the formation of Heinz bodies. n-Propyl disulphide depletes the enzyme glucose-6-phosphate dehydrogenase (G6PD) within red blood cells which renders them more susceptible to oxidative damage. The formation of eccentrocytes (deformed red blood cells that occur in the presence of oxidant stress) and Heinz bodies make the cell more fragile and subject to extravascular haemolysis.

Cooking, dehydration or spoilage of Allium species does not reduce the risk of toxic effects, and so ingestion of food intended for human consumption may cause toxic effects in pets.
Clinical signs of Allium poisoning
Signs of anaemia after ingestion of Allium species may occur suddenly within 24 hours if a large quantity has been ingested but it is more common for signs to occur after several days (usually from 1–5 days). Heinz bodies can appear within 24 hours and can increase in number over the next few days before declining.
Gastrointestinal effects may occur soon after ingestion, with inappetence, vomiting, abdominal discomfort and diarrhoea, and the breath and urine may smell strongly of onions or garlic. Other clinical signs are due to anaemia with depression, lethargy, weakness, pale mucous membranes, tachycardia and tachypnoea. Haematuria and haemoglobinuria are common (and may be the presenting signs).
Haematological changes reflect oxidative damage with low packed cell volume (PCV) and haemoglobin, and erythrocytes with Heinz bodies. Blood smears may reveal eccentrocytosis (red blood cells with a ragged fringe), spherocytosis (sphere-shaped red blood cells), poikilocytosis (abnormally shaped red blood cells) and anisocytosis (unequal sized red blood cells).
Management of Allium poisoning
Any animal with clinical signs after ingestion of onion or garlic should be assessed for anaemia. Gut decontamination could be considered after ingestion of onions or garlic, etc, particularly if the quantity ingested is large; an emetic can be given if ingestion was within 1–2 hours, followed by activated charcoal (1–3 g/kg). Thereafter, most animals can probably be sent home with advice to ensure adequate hydration and, if possible, to provide a high protein diet, as this may help promote restoration of glutathione stores (an important cellular compound involved in protecting against oxidative damage) (Simmons, 2001) and to return if there is any sign suggestive of anaemia (e.g. pale mucous membranes, lethargy, weakness, dark urine) over the next few days.
Treatment of Allium-induced anaemia is supportive as there is no antidote. Antioxidants such as vitamin E, ascorbic acid and acetylcysteine are unlikely to be of benefit (Cope, 2005). A blood transfusion may be required in a critically ill animal (Kay, 1983; Simmons, 2001). The use of corticosteroids in this form of haemolysis is controversial as it will prolong the clearing of affected cells by suppression of the recticuloendothelial system, and therefore may not be beneficial (Solter and Scott, 1987). Human erythropoietin (a hormone that stimulates stem cells in the bone marrow to become red blood cells) has been used in a dog with Heinz body anaemia after ingestion of Chinese chive (Allium tuberosum) and garlic (Allium sativum) (Yamato et al, 2005) but it is unclear if it was of any benefit.
Recovery from Allium-induced anaemia usually occurs over 3–7 days but can be longer is severe cases. Death can occur but is unlikely with good supportive measures.
Methaemoglobinaemia
The iron in haemoglobin functions in the ferrous state (Fe2+) but can be oxidised by toxins to the ferric state (Fe3+). This changes haemoglobin to methaemoglobin which cannot bind oxygen and is therefore unable to perform its primary function of oxygen delivery to tissues. This change in haemoglobin is reversible. The laboratory measurement of methaemoglobin is given as a percentage of normal haemoglobin, but this test is not readily available in veterinary medicine and the presence of methaemoglobinaemia is usually made on clinical grounds. The blood in animals (and humans) with methaemoglobinaemia is characteristically chocolate brown in colour, does not change colour when oxygenated, and cyanosis and respiratory signs do not improve with oxygen therapy.
Although several substances can cause methaemoglobinaemia (Box 2), a common cause in cats is paracetamol ingestion, as they are unable to metabolise paracetamol to safe metabolites. This results in the formation of toxic metabolites which damage red blood cells and the liver. In all species paracetamol is metabolised in the liver by glucuronidation, sulphation and oxidation. Cats have a restricted ability to conjugate with glucuronic acid as they have low levels of glucuronyl transferase, the enzyme that catalyses the final step of the glucuronidation pathway. Unlike most other species, rather than glucuronidation, sulphation is the primary metabolic pathway of paracetamol metabolism and the products of the minor oxidation route become more significant (Maddison et al, 2008). Oxidising metabolites induce methaemoglobin formation, Heinz body formation and denaturation of red blood cell membranes. It is also possible that a minor metabolite of paracetamol (paraaminophenol) is responsible for the methaemoglobinaemia seen in cats and dogs with paracetamol poisoning (McConkey et al, 2009). This is usually removed as N-acetyl conjugates but cats have only one of the enzymes responsible for this reaction and dogs have none. This means that both species are less efficient than other species at removing this toxic metabolite which is known to undergo reactions with haemoglobin. Although methaemoglobinaemia occurs in dogs after paracetamol ingestion they are able to tolerate much higher doses than cats due to their ability to metabolise paracetamol more efficiently.
Box 2.Some drugs and chemicals that can cause methaemoglobinaemia
- Benzocaine
- Chlorates
- Dapsone
- Lidocaine
- Nitrates and nitrites
- Paracetamol
Clinical signs of paracetamol poisoning
Early effects (usually starting within 4 hours) of paracetamol poisoning in cats include progressive cyanosis associated with tachycardia, tachypnoea and dyspnoea as a result of methaemoglobin formation. Mucous membranes appear brown in colour, and weakness and lethargy may be observed. There may also be facial and paw oedema, depression, vomiting, anorexia and vocalisation. Haematuria, anaemia, and evidence of haemolysis may be present.
Later effects (from 24 hours) include liver damage (Kolf-Clauw and Keck, 1994), but hepatic necrosis is not the principal cause of fatality in cats as they usually die as a result of severe methaemoglobinaemia (Hjelle and Grauer, 1986). Haemoglobinuria, intravascular haemolysis, jaundice and other evidence of liver damage may be seen in cats that survive the initial stages of paracetamol poisoning.
Management of paracetamol poisoning
If a potentially toxic dose has been ingested recently, emesis can be induced and activated charcoal given. In humans there is evidence that activated charcoal appears to reduce the number of patients that achieve toxic paracetamol concentrations and thus may reduce the need for treatment and hospital stay (Buckley et al, 1999).
The aim of treatment of animals with paracetamol poisoning is to ensure adequate oxygenation and prevent further metabolism of paracetamol to toxic metabolites (with the use of antidotes) and prevent damage to the liver and red blood cells.
Monitoring for evidence of methaemoglobinaemia, liver damage, anaemia and haemolysis and renal impairment is required. The most widely used antidote in paracetamol poisoning is acetylcysteine (N-acetylcysteine) because it can significantly reduce the toxicity of the drug by a variety of mechanisms. First, it is a precursor of glutathione which is required in the metabolism of paracetamol. Second, acetylcysteine acts directly on the toxic metabolites to form an acetylcysteine conjugate which can be excreted, although this reaction is slow. Third, it is oxidised in the liver to form sulphate thereby increasing the capacity of the sulphation pathway. Administration of acetylcysteine has been shown to reduce the half-life of paracetamol by half in cats (Rumbeiha et al, 1995).
Cats with evidence of severe haemolysis, significant decrease in packed cell volume (PCV) or severe anaemia usually require whole blood transfusions. Recovery in treated cats usually occurs within 2 days (Aronson and Drobatz, 1996), depending on the severity of signs, but biochemical abnormalities may take up to 3 weeks to return to normal concentrations.
Clotting disorders
Following injury to blood vessels the escaping liquid blood must be converted into a gel (a clot) in order to plug the hole and reduce further blood loss. The plasma portion of blood contains proteins that act together in a series of enzyme activation events (a cascade), resulting in formation of a fibrin clot. If this process it disrupted, and this can happen at various stages of the cascade, the blood fails to clot and haemorrhage occurs.
The most common toxins to affect the clotting cascade are the anticoagulant rodenticides, brodifacoum, bromadiolone, chlorophacinone, coumatetralyl, difenacoum, difethialone, diphacinone, and flocoumafen. These are available in numerous forms as grain, pasta baits, ‘throw packs’ and pre-baited boxes and products are often dyed, particularly blue or green (Figure 2). The typical strength is 0.0025% for amateur products and 0.005% strength for professional products.

These long-acting compounds affect the recycling of vitamin K in the clotting cascade. Vitamin K is a cofactor in the activation of clotting factors II (prothrombin), VII, IX and X. Without vitamin K these coagulation proteins remain in a non-functional state. Anticoagulant rodenticides inhibit hepatic vitamin K1 epoxide-reductase, the enzyme responsible for conversion of vitamin K1 epoxide to vitamin K1. This inhibition results in the gradual depletion of the body stores of vitamin K1, causing a reduction in factors II (prothrombin), VII, IX and X resulting in inhibition of prothrombin synthesis in the liver. Once vitamin K1 and the clotting factors have been depleted, bleeding occurs. That is why signs only occur after a lag-time of 3 to 5 days.
Clinical signs of anticoagulant rodenticide poisoning
The first indication an owner may have that a pet has eaten some rat or mouse bait is the presence of the bait, usually bluey-green, in the faeces or the sudden onset of weakness and depression. External bleeding is not always apparent.
Clinical signs of anticoagulant rodenticide poisoning are due to coagulopathy and any type of bleeding may occur. As a result, signs are variable. Initial signs may be non-specific with lethargy, weakness, anorexia, cough, depression and pale mucous membranes. Haemorrhage into the lungs is a common site of bleeding (Schulman et al, 1986; Lewis et al, 1997), and hence cough is a common initial sign; extensive bruising of the skin may occur. In severe cases hypovolaemic shock may occur after rapid blood loss, leading to secondary organ ischaemia.
Clinical effects are typically seen within 3–5 days of exposure, but may be delayed for up to 7 days (DeClementi and Sobczak, 2012). Clotting parameters become prolonged before the onset of clinical signs.
There is increased prothrombin time (PT), activated partial thromboplastin (aPPT) and activated clotting time (ACT). The PT may become prolonged from 36–72 hours, and after 72 hours the aPPT and ACT becomes prolonged (DeClementi and Sobczak, 2012).
Management of anticoagulant rodenticide poisoning
If a potentially toxic dose has been ingested recently and there is no evidence of bleeding, emesis can be induced and activated charcoal given.
In asymptomatic animals there are two treatment options:
- Either test the PT at 48–72 hours after ingestion and then treat with vitamin K1 according to results (if the PT is normal, no treatment is required and if the PT is prolonged treat with vitamin K1 for at least 21 days and assess clotting parameters 48 hours after the last dose), or
- Treat with vitamin K1 for at least 21 days and then assess the PT 48 hours after the last dose.
The decision on which option to take should be assessed on a case by case basis depending on the history (acute or chronic exposure, dose ingested, time since ingestion, etc). If there is any delay in obtaining results of the PT vitamin K1 can be given in the interim, once the sample has been taken, and the decision to stop or continue taken once the results are known.
Although acute ingestion of a small amount of anticoagulant rodenticide is usually not a concern, it is important to discuss the possibility of multiple exposures with the owner as this would increase the risk of poisoning. There is a potential risk of unobserved exposure, for example, bait may be inaccessible to pets when put down, but it can be moved by rodents (they can move grains, throw packs or even blocks of bait). In addition, a rodent problem may not be isolated to a single household and neighbours may also be using rodenticide which could be accessible to pets. If there is any suspicion of chronic exposure treatment should be started with vitamin K1.
It is essential to advise owners to prevent any further exposure to any bait and to clear up any spills promptly. In animals not receiving vitamin K1 owners should be advised to look for any evidence of bleeding over the next few days, e.g. bleeding from gums or nose, blood in the stools, bruising, pale mucous membranes, lethargy or weakness, and advised to return for assessment immediately.
Testing the PT before 36 hours is not appropriate unless chronic ingestion is suspected. Also, if vitamin K1 has already been given the PT will be normal for the next 48 hours and signs would be expected at 5–7 days, not the usual 3–5 days (Lee, 2013). Monitoring clotting parameters while the animal is on vitamin K1 therapy is not necessary as values should be normal, unless it is to check that the PT has normalised.
Treatment is aimed at replacing inactive clotting factors and providing vitamin K1 to allow the liver to synthesise its own clotting factors.
Vitamin K1 therapy should be started immediately in any animal with bleeding. Although vitamin K1 is immediately available to the body for the synthesis of new clotting factors, the effect of vitamin K1 is not immediate as it can take 6–12 hours to synthesise new clotting factors. Therefore, in an emergency a blood transfusion will be required. Clotting factors can be rapidly restored with one or more transfusions of plasma or whole blood. Animals receiving treatment usually improve within 24 hours.
Care must also be taken when taking blood samples as the site of venepuncture may bleed excessively. The smallest possible needle should be used. Animals with severe coagulopathy require careful handling to avoid unnecessary stress and risk of haemorrhage and may require sedation when undergoing treatment.
Vitamin K1 therapy must be continued for as long as the anticoagulant is in the body and some have long half-lives. In most cases therapy is required for 3 weeks or more and owners should be advised that it is essential to complete the full course. Bleeding can recur weeks later if vitamin K1 therapy is not continued for long enough and death can occur days after ingestion (depending on the site of bleeding). Clotting parameters should be measured 48–72 hours after the last dose of vitamin K1 to check clotting parameters have returned to and remain normal. If clotting is prolonged vitamin K1 should be continued.
Bone marrow depression
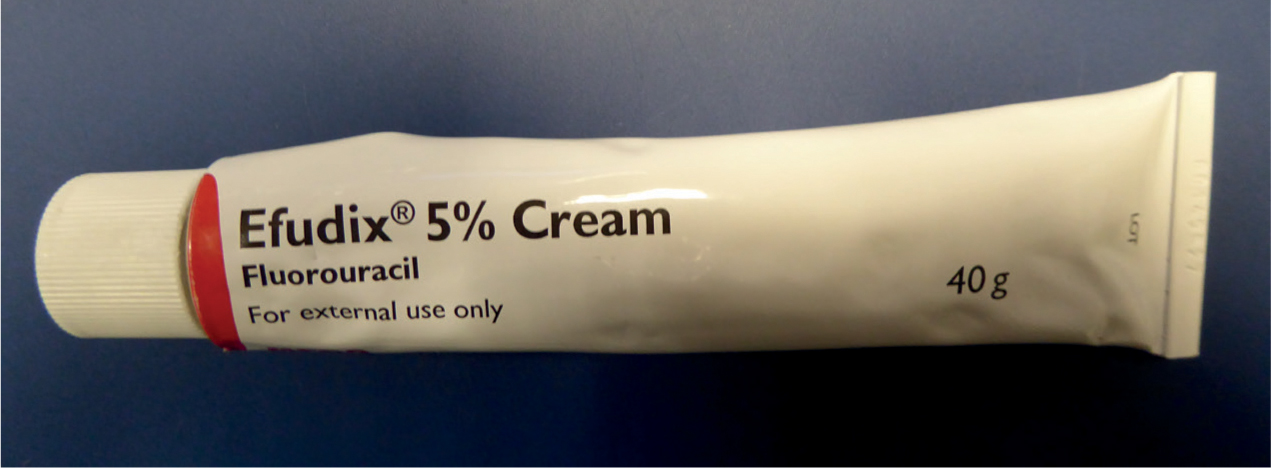
The production of blood cells (haematopoiesis) occurs in the bone marrow and some toxic substances disrupt this process. One such drug is 5-fluorouracil (5-FU) which is used in the treatment of cancer as it destroys rapidly dividing cells. In humans 5-FU is also used dermally for the treatment of pre-malignant and malignant skin lesions and most companion animals are exposed when they access and chew 5-FU cream (typically a 5% cream, Figure 3). Occasionally, toxic effects occur after owners apply the cream to their pet's skin (Dorman et al, 1990; Snavely et al, 2010).
5-FU is an analogue of uracil, a component of ribonucleic acid (RNA). It acts as an antimetabolite and interferes with deoxyribonucleic acid (DNA) and possibly RNA synthesis. As a result, 5-FU inhibits cell division and causes cell death. Tissues with rapidly dividing cells, such as the bone marrow and intestinal crypt cells, are most susceptible to its effects.
5-FU also causes neurotoxicity but this is via a different mechanism. It is thought to occur because 5-FU is metabolised to fluorocitrate which inhibits the tricarboxylic acid cycle (Koenig and Patel, 1970), blocking the gamma-aminobutyric acid (GABA) shunt resulting in low concentrations of GABA in the brain which can cause seizures.
Most cases of 5-FU poisoning occur in dogs and mortality is high. Even a relatively small quantity can cause severe poisoning and 5-FU is contraindicated in cats because of the risk of potentially fatal neurotoxicity. The lowest toxic oral dose of 5-FU in dogs is usually quoted as 8.6 mg/kg (equivalent to 0.17 g of a 5% cream/kg; Albretsen et al, 1998) and the lowest fatal dose as 20 mg/kg (equivalent to 0.40 g of cream/kg) (Dorman et al, 1990; Albretsen et al, 1998). Survival is uncommon in dogs after ingestion of >40 mg/kg (Dorman et al, 1990).
Clinical signs of 5-FU poisoning
Clinical effects after exposure to 5-FU can occur rapidly, usually within an hour but can sometimes be delayed for up to 5 hours (Albretsen, 2001; Stern, 2016). 5-FU causes gastrointestinal signs, rapidly followed by neurological effects and then, days later, bone marrow depression.
Common signs of 5-FU poisoning are vomiting, ataxia, tremors, respiratory distress or depression and convulsions. Bone marrow suppression can occur after exposure to 5-FU but is not commonly observed because most animals with severe fluorouracil poisoning do not survive the neurotoxic effects (Albretsen, 2001). Bone marrow suppression generally occurs within 4–7 days and may last up to 30 days (Stern, 2016). Leucopenia and thrombocytopenia occur from days 4–7, anaemia occurs from day 9 with the nadir for all cell types occuring on days 9–14. Signs include depression, pyrexia and the risk of secondary infection. Coagulopathy and mild elevation in liver enzymes may also occur.
Management of 5-FU poisoning
There is no specific antidote for companion animals with 5-FU poisoning. IV fluids are recommended to maintain hydration and enhance elimination (Stern, 2016) and antiemetics are recommended for severe vomiting. Metoclopramide should be used with caution because it can cause additional neurological effects (Dorman et al, 1990). Gastric protectants such as omeprazole and sucralfate can be given and an opioid may be required for pain relief (Stern, 2016).
The blood count should be monitored regularly (Stern, 2016) and the liver and renal function and coagulation (baseline and then as clinically indicated) should also be checked. Neurological status, vital signs and electrocardiogram (ECG), if possible, should be monitored.
Seizures in animals with 5-fluorourcacil poisoning can be very difficult to control and refractory to anti-epileptic drugs (Stern, 2016). Diazepam is usually ineffective to control convulsions and barbiturates, isoflurane or propofol may be needed. Levetiracetam was used successfully in a dog following a massive overdose of 5-FU (Friedenberg et al, 2013).
Any animal with evidence of bone marrow suppression should receive antibiotic cover because of the risk of infection but metronidazole should not be used as it reduces clearance of 5-FU and increases toxicity (Bardakji et al, 1986). Also, steroids are best avoided because of their immunosuppressant effects. Blood transfusions may be required in animals with excessive blood loss (Dorman et al, 1990).
Filgrastim (a human granulocyte colony stimulating factor) could be considered to stimulate bone marrow stem cell proliferation in animals where the white cell count fails to recover. It has been used in dogs with bone marrow suppression following 5-FU overdose (Albretsen et al, 1998; Fry and Forman, 2004).
Conclusions
Poisoning can disrupt the normal function of the blood through various mechanisms. The lifespan of red blood cells can be shortened through oxidative damage and toxic mechanisms resulting in anaemia. Haemoglobin is also subject to oxidative damage resulting in the formation of methaemoglobin which is non-functioning, resulting in tissue hypoxia. The clotting cascade can be disrupted by anticoagulant rodenticides resulting in delayed-onset haemorrhage and some substances can disrupt the formation of blood cells as a result of bone marrow depression. Owners need to be questioned about possible exposure to toxic substances that affect the normal function of the blood to determine the most appropriate treatment and in some cases the use of antidotes.
KEY POINTS
- A number of toxic drugs and chemicals can affect the normal functioning of the blood.
- Onions and related plants such as leeks and garlic can cause Heinz body anaemia in cats and dogs.
- Haemolytic anaemia is the main feature of zinc toxicosis in dogs.
- Haemoglobin in red blood cells can be changed by several toxins, but most commonly paracetamol metabolites, to methaemoglobin which is non-functioning as it cannot transport oxygen to tissues.
- Anticoagulant rodenticides are a common cause of haemorrhage in companion animals, as a result of their disruption of the clotting cascade.
- The process of blood cell production can also be disrupted, resulting in bone marrow depression.


