Aggressive canine patients are not rarely encountered in practice, as current surveys show that 7% of UK owners' dogs demonstrate aggressive behaviour towards strangers (Casey et al, 2014), with human-directed aggression the main presentation of canine aggression reported to veterinary behaviourists (Bamberger and Houpt, 2006). Veterinary staff come into close contact with canine patients and so are more likely targets of aggression (Fatjo, 2007). However, despite the risk aggressive behaviour brings to veterinary personnel, the registered veterinary nurse must ensure the patient receives adequate care. The Animal Welfare Act 2006 ensures animal needs are met by the person responsible for their care, therefore this responsibility extends to registered veterinary nurses during their hospitalisation. Under the Royal College of Veterinary Surgeons (2017) code of professional conduct, the duty of registered veterinary nurses is to make animal health and welfare their first consideration by providing appropriate and adequate nursing care. However, the Royal College of Veterinary Surgeons code also states ‘Veterinary surgeons are not expected to tolerate threatening, aggressive, or violent behaviour or to compromise their personal safety when attending to animals’. This opens up an interesting discussion as canine human-directed aggression is a significant welfare consideration, as it can subsequently make clinical treatment of patients difficult (Odore et al, 2020). This queries if a balance between patient welfare and personal safety is possible if there is a considerable compromise to personal health and safety.
Aggression negatively influences patients' welfare and management as Mikkola et al (2021) state that aggressive dogs are more predisposed to untreated pain, rehoming and euthanasia. However, the literature investigating how aggression impacts the quality of veterinary nursing care is minimal. Moffat (2008) explored the consequences of aggressive behaviour within elements of care relating to restraint and handling. They report that staff are prone to losing patience with aggressive patients, resulting in excessive force and restraint, use of stressful tape muzzles, unsafe dog catcher poles, and undesirable techniques such as induction chambers that increase dangers to the patient through anaes-thesia-associated risks. Such methods elicit fearful interactions, leading to animals forming negative associations with the clinical environment (Moffat, 2008). Shaw and Martin (2014) discuss how aggressive patients are therefore more likely to develop hospital aversion, making them difficult to treat and, ultimately, compromising their welfare.
Patients exhibiting human-directed aggression are commonly labelled as ‘CARE’ in their clinical history to serve as a warning for other staff encountering these patients.
This study aimed to identify if the standard of nursing care differs between CARE-labelled canine patients and other canine patients and determine if there is any statistically significant difference. The hypothesis for this project was ‘canine patients labelled as aggressive receive a lower quality of nursing care compared to non-aggressive canine patients’.
Materials and methods
Procedure
This cross-sectional study used an online distributed questionnaire via JISC Online Surveys. The questionnaire was distributed via social media platforms, such as Facebook and Twitter, on veterinary nursing community pages. Open invitations were also emailed to the first author's own practice, and the Royal Veterinary College's Queen Mother Hospital for Animals.
Participants
Participants were UK-based registered veterinary nurses who had been in practice within the last 12 months.
Survey design
The questionnaire comprised four parts. Figure 1 shows the survey structure. Questions under parts 3 and 4 ask participants to score themselves on a Likert scale of 1–5, with 1 being very unlikely to 5 being extremely likely to perform the different nursing activities.
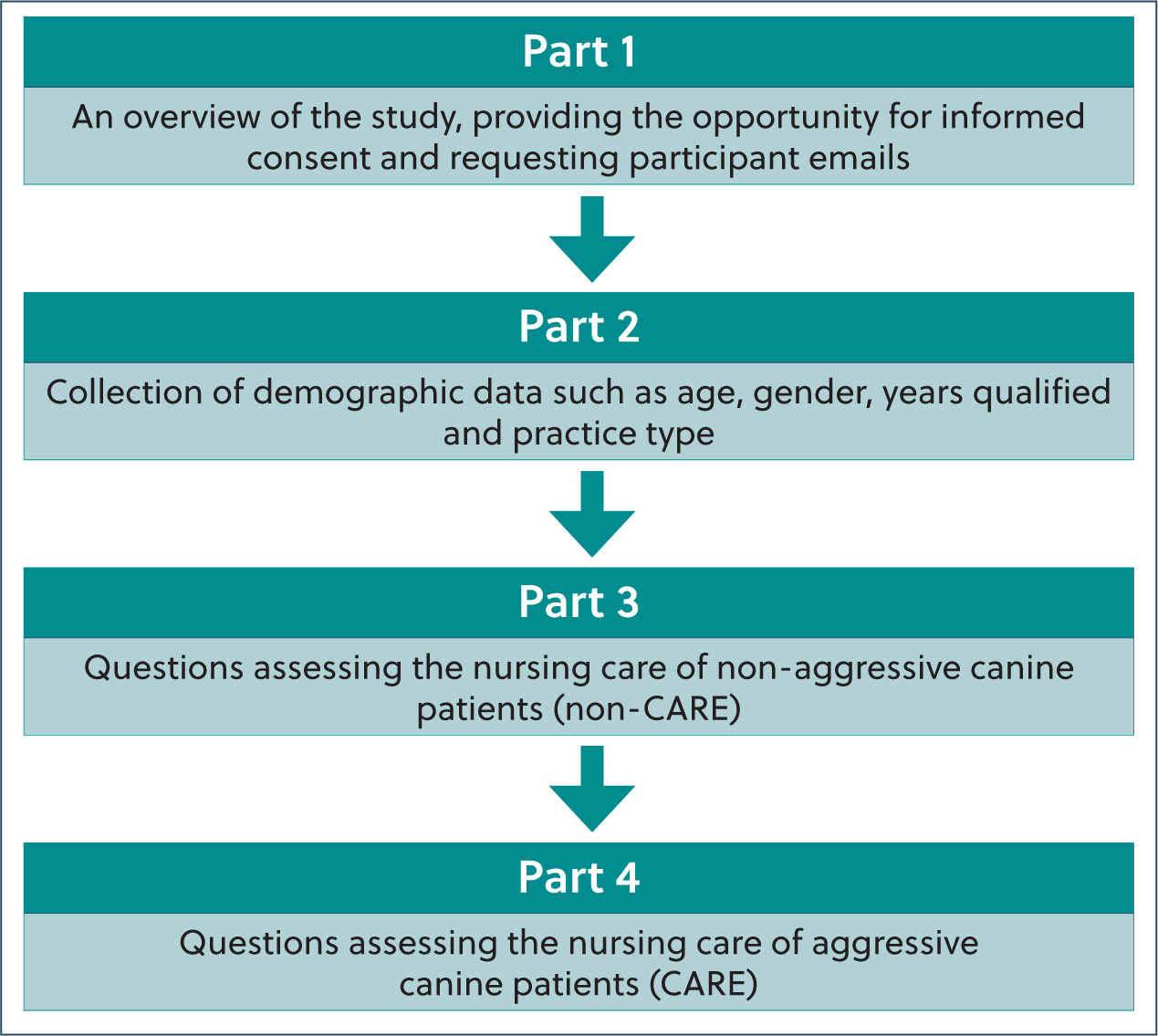
Parts 3 and 4 were based on the Orpet and Jeffery Ability Model (OJAM) on meeting the patient's needs (Orpet and Welsh, 2011), such as housing, maintaining hygiene and feeding. Nursing activities were derived from instructions in chapters of the BSAVA Textbook of Veterinary Nursing (Atkinson et al, 2018; Monsey and Devaney, 2018; Gajanayake et al, 2018; Goddard and Irving, 2018; Goddard and Phillips, 2018; Jeffery and Ford-Fennah, 2018) and literature by Moffat (2008). An open comment section was included at the end of the questionnaire which requested participant's opinions on how they thought nursing care differs between the two patient types.
Ethics
The Royal Veterinary College's Social Sciences Research Ethical Review Board (SSRERB) granted ethical approval. Responses were kept confidential under the guidelines of the General Data Protection Regulations and the Data Protection Act 2018.
Statistical tests
Survey responses were exported to Microsoft Excel to be screened and formatted. The data were then exported to IBM SPSS V26 for statistical analysis. Data were summarised by frequency and percentage groupings, while Pearson's chi-squared test was used to identify an association between the categorical variables, with a significance value set at P=0.05.
Results
A total of 390 registered veterinary nurses completed the questionnaire: 56% of respondents were in the 25–34 year age group, with 99% of the sample identifying as female. The majority of respondents were in general first opinion practices (48.5%) and first opinion hospital practices (28%). Forty-four percent of the registered veterinary nurses had qualified between 1–5 years ago, with 19% having qualified in the last 12 months.
Are patients labelled as aggressive likely to receive different nursing care?
The data indicated various differences in veterinary nursing care based on whether patients were aggressive or non-aggressive. Table 1 shows these data alongside corresponding P-values.
Table 1. Differences in nursing care for CARE and non-CARE patients
| The likelihood of various nursing activities being carried out | Likert responses | Patient type | P value | |
|---|---|---|---|---|
| Non-CARE | CARE | |||
| Check if patient has soiled bedding one to two times a day | Unlikely (1) | 67 (17.2) | 35 (9.0) | <0.001 |
| Neutral (2) | 71 (18.2) | 26 (6.7) | ||
| Likely (3) | 252 (64.6) | 329 (84.4) | ||
| Provide heat pads or cold pads if advisable | Unlikely (1) | 5 (1.3) | 16 (4.1) | <0.001 |
| Neutral (2) | 8 (2.1) | 29 (7.4) | ||
| Likely (3) | 377 (96.7) | 345 (88.5) | ||
| Select a ground floor kennel appropriate to patient size | Unlikely (1) | 1 (0.3) | 6 (1.5) | 0.011 |
| Neutral (2) | 12 (3.1) | 3 (0.8) | ||
| Likely (3) | 377 (96.7) | 381 (97.7) | ||
| Check if patient has soiled bedding hourly | Unlikely (1) | 37 (9.5) | 98 (25.1) | <0.001 |
| Neutral (2) | 57 (14.6) | 57 (14.6) | ||
| Likely (3) | 296 (75.9) | 235 (60.3) | ||
| Check if patient has soiled bedding one to two times a day | Unlikely (1) | 80 (20.5) | 56 (14.4) | 0.020 |
| Neutral (2) | 49 (12.6) | 38 (9.7) | ||
| Likely (3) | 261 (66.9) | 296 (75.9) | ||
| Remove patient's soiled bedding immediately and wash | Unlikely (1) | 1 (0.3) | 11 (2.8) | <0.001 |
| Neutral (2) | 4 (1.0) | 19 (4.9) | ||
| Likely (3) | 385 (98.7) | 360 (92.3) | ||
| Clean any abnormal discharge from patients (aural, ocular, nasal, oral or genital) | Unlikely (1) | 5 (1.3) | 110 (28.2) | <0.001 |
| Neutral (2) | 15 (3.8) | 122 (31.3) | ||
| Likely (3) | 370 (94.9) | 158 (40.5) | ||
| Bathe patient from any urine and soiling | Unlikely (1) | 3 (0.8) | 44 (11.3) | <0.001 |
| Neutral (2) | 10 (2.6) | 79 (20.3) | ||
| Likely (3) | 377 (96.7) | 267 (68.5) | ||
| Dry patient after bathing | Unlikely (1) | 5 (1.3) | 62 (15.9) | <0.001 |
| Neutral (2) | 10 (2.6) | 83 (21.3) | ||
| Likely (3) | 375 (96.2) | 245 (62.8) | ||
| Clean vomit/regurgitation or excessive salivation from mouth with damp swabs | Unlikely (1) | 6 (1.5) | 150 (38.5) | <0.001 |
| Neutral (2) | 11 (2.8) | 107 (27.4) | ||
| Likely (3) | 373 (95.6) | 133 (34.1) | ||
| Reduce stressors in environment when feeding patient | Unlikely (1) | 20 (5.1) | 14 (3.6) | <0.001 |
| Neutral (2) | 59 (15.1) | 23 (5.9) | ||
| Likely (3) | 311 (79.7) | 353 (90.5) | ||
| Ensure patient is not in pain (pain score) when feeding | Unlikely (1) | 0 (0.0) | 10 (2.6) | 0.004 |
| Neutral (2) | 14 (3.6) | 19 (4.9) | ||
| Likely (3) | 376 (96.4) | 361 (92.6) | ||
| Spend time with patient if not eating (e.g. talking, stroking, and offering food by hand) | Unlikely (1) | 3 (0.8) | 93 (23.8) | <0.001 |
| Neutral (2) | 5 (1.3) | 83 (21.3) | ||
| Likely (3) | 382 (97.9) | 214 (54.9) | ||
| Remove patient's uneaten food after short period | Unlikely (1) | 11 (2.8) | 34 (8.7) | 0.002 |
| Neutral (2) | 31 (7.9) | 33 (8.5) | ||
| Likely (3) | 348 (89.2) | 323 (82.8) | ||
| Assess patient for signs of pain against all steps of validified pain scale | Unlikely (1) | 15 (3.8) | 67 (17.2) | <0.001 |
| Neutral (2) | 16 (4.1) | 70 (17.9) | ||
| Likely (3) | 359 (92.1) | 253 (64.9) | ||
| Assess patient for signs of pain only against some steps of validified pain scale | Unlikely (1) | 204 (52.3) | 59 (15.1) | <0.001 |
| Neutral (2) | 75 (19.2) | 56 (14.4) | ||
| Likely (3) | 111 (28.5) | 275 (70.5) | ||
| Open the kennel door slowly when exercising patient | Unlikely (1) | 18 (4.6) | 3 (0.8) | <0.001) |
| Neutral (2) | 45 (11.5) | 3 (0.8) | ||
| Likely (3) | 327 (83.8) | 384 (98.5) | ||
| Take patient for out of kennel exercise once a day | Unlikely (1) | 155 (39.7) | 127 (32.6) | 0.024 |
| Neutral (2) | 38 (9.7) | 59 (15.1) | ||
| Likely (3) | 197 (50.5) | 204 (52.3) | ||
| Take patient for out of kennel exercise three times or more a day | Unlikely (1) | 55 (14.1) | 82 (21.0) | 0.002 |
| Neutral (2) | 48 (12.3) | 66 (16.9) | ||
| Likely (3) | 287 (73.6) | 242 (62.1) | ||
| Crouch to dog's level and allow it to approach you first when taking out | Unlikely (1) | 24 (6.2) | 91 (23.3) | <0.001 |
| Neutral (2) | 54 (13.8) | 67 (17.2) | ||
| Likely (3) | 312 (80.0) | 232 (59.5) | ||
| Provide ‘change of scenery’ for the non-ambulatory patient | Unlikely (1) | 67 (17.2) | 108 (27.7) | <0.001 |
| Neutral (2) | 82 (21.0) | 93 (23.8) | ||
| Likely (3) | 241 (61.8) | 189 (48.5) | ||
| Allow the dog to greet any new member of staff that you ask to assist restrain | Unlikely (1) | 9 (2.3) | 48 (12.3) | <0.001 |
| Neutral (2) | 17 (4.4) | 45 (11.5) | ||
| Likely (3) | 364 (93.3) | 297 (76.2) | ||
| Use basket muzzle when restraining the patient | Unlikely (1) | 103 (26.4) | 2 (0.5) | <0.001 |
| Neutral (2) | 153 (39.2) | 16 (4.1) | ||
| Likely (3) | 134 (34.4) | 372 (95.4) | ||
| Use tape muzzle when restraining the patient | Unlikely (1) | 373 (95.6) | 324 (83.1) | <0.001 |
| Neutral (2) | 17 (4.4) | 66 (16.9) | ||
| Likely (3) | 0 (0.0) | 0 (0.0) | ||
| Use dog catcher when restraining patient | Unlikely (1) | 373 (95.4) | 336 (86.2) | <0.001 |
| Neutral (2) | 14 (3.6) | 32 (8.2) | ||
| Likely (3) | 4 (1.0) | 22 (5.6) | ||
| Allow patient to sniff and familiarise with any equipment before use during restraint | Unlikely (1) | 12 (3.1) | 49 (12.6) | <0.001 |
| Neutral (2) | 25 (6.4) | 48 (12.3) | ||
| Likely (3) | 353 (90.5) | 293 (75.1) | ||
| Use distraction (talking in calm manner, stroke/scratch/massage/treats) when restraining patient | Unlikely (1) | 0 (0.0) | 3 (0.8) | 0.022 |
| Neutral (2) | 1 (0.3) | 7 (1.8) | ||
| Likely (3) | 389 (99.7) | 380 (97.4) | ||
| During temperature, pulse and respiration check to allow patient to sniff and familiarise self with equipment | Unlikely (1) | 11 (2.8) | 41 (10.5) | <0.001 |
| Neutral (2) | 30 (7.7) | 43 (11.0) | ||
| Likely (3) | 349 (89.5) | 306 (78.5) | ||
| Have patient suitably restrained for temperature, pulse and respiration check | Unlikely (1) | 17 (4.4) | 3 (0.8) | <0.001 |
| Neutral (2) | 47 (12.1) | 4 (1.0) | ||
| Likely (3) | 326 (83.6) | 383 (98.2) | ||
| Monitor patient's heart rate for at least 15 seconds | Unlikely (1) | 2 (0.5) | 10 (2.6) | 0.007 |
| Neutral (2) | 5 (1.3) | 14 (3.6) | ||
| Likely (3) | 383 (98.2) | 366 (93.8) | ||
| Palpate patient's pulse simultaneously to ensure no pulse deficit | Unlikely (1) | 29 (7.4) | 100 (25.6) | <0.001 |
| Neutral (2) | 66 (16.9) | 76 (19.5) | ||
| Likely (3) | 295 (75.6) | 214 (54.9) | ||
| Take patient's respiration rate from afar or outside kennel | Unlikely (1) | 10 (2.6) | 1 (0.3) | <0.001 |
| Neutral (2) | 11 (2.8) | 3 (0.8) | ||
| Likely (3) | 369 (94.6) | 386 (99.0) | ||
| Open kennel door slowly before administering intravenous medication to patient | Unlikely (1) | 15 (3.8) | 6 (1.5) | <0.001 |
| Neutral (2) | 39 (10.0) | 12 (3.1) | ||
| Likely (3) | 336 (86.2) | 372 (95.4) | ||
| Crouch to patient's level when administering intravenous medication | Unlikely (1) | 4 (1.0) | 62 (15.9) | <0.001 |
| Neutral (2) | 13 (3.3) | 62 (15.9) | ||
| Likely (3) | 373 (95.6) | 266 (68.2) | ||
| Allow patient to sniff and familiarise self with syringe/equipment when administering intravenous medication | Unlikely (1) | 46 (11.8) | 81 (20.8) | 0.002 |
| Neutral (2) | 52 (13.3) | 57 (14.6) | ||
| Likely (3) | 292 (74.9) | 252 (64.6) | ||
| Use basic commands with patients when administering intramuscular medication | Unlikely (1) | 3 (0.8) | 4 (1.0) | 0.025 |
| Neutral (2) | 21 (5.4) | 7 (1.8) | ||
| Likely (3) | 366 (93.8) | 379 (97.2) | ||
| Allow the dog to greet any new member of staff that you ask to assist with intramuscular injection | Unlikely (1) | 5 (1.3) | 37 (9.5) | <0.001 |
| Neutral (2) | 19 (4.9) | 46 (11.8) | ||
| Likely (3) | 366 (93.8) | 307 (78.7) | ||
| Use basket muzzle on patient when administering intramuscular medication | Unlikely (1) | 105 (26.9) | 4 (1.0) | <0.001 |
| Neutral (2) | 153 (39.2) | 12 (3.1) | ||
| Likely (3) | 132 (33.8) | 374 (98.9) | ||
| Use tape muzzle on patient when administering intramuscular medication | Unlikely (1) | 339 (86.9) | 276 (70.8) | <0.001 |
| Neutral (2) | 35 (9.0) | 54 (13.8) | ||
| Likely (3) | 16 (4.1) | 60 (15.4) | ||
| Use dog catcher on patient when administering intramuscular medication | Unlikely (1) | 366 (93.8) | 336 (86.2) | <0.001 |
| Neutral (2) | 19 (4.9) | 35 (9.0) | ||
| Likely (3) | 5 (1.3) | 19 (4.9) | ||
| Allow patient to sniff and familiarise self with equipment before use when administering intramuscular medication | Unlikely (1) | 39 (10.0) | 69 (17.7) | 0.002 |
| Neutral (2) | 46 (11.8) | 58 (14.9) | ||
| Likely (3) | 305 (78.2) | 263 (67.4) | ||
| Massage patient's intramuscular site post injection | Unlikely (1) | 10 (2.6) | 45 (11.5) | <0.001 |
| Neutral (2) | 10 (2.6) | 32 (8.2) | ||
| Likely (3) | 370 (94.9) | 313 (80.3) | ||
| Allow patient to greet new member of staff you ask to assist when taking bloods/inserting intravenous catheter in | Unlikely (1) | 6 (1.5) | 33 (8.5) | <0.001 |
| Neutral (2) | 11 (2.8) | 50 (12.8) | ||
| Likely (3) | 373 (95.6) | 307 (78.7) | ||
| Use basket muzzle on patient when taking bloods/inserting intravenous catheter | Unlikely (1) | 100 (25.6) | 5 (1.3) | <0.001 |
| Neutral (2) | 167 (42.8) | 10 (2.6) | ||
| Likely (3) | 123 (31.5) | 375 (96.2) | ||
| Allow patient to sniff and familiarise with equipment before use when taking bloods/inserting intravenous catheter | Unlikely (1) | 35 (9.0) | 66 (16.9) | 0.001 |
| Neutral (2) | 45 (11.5) | 55 (14.1) | ||
| Likely (3) | 310 (79.5) | 269 (69.0) | ||
| Use EMLA cream before taking bloods/inserting intravenous catheter | Unlikely (1) | 94 (24.1) | 88 (22.6) | <0.001 |
| Neutral (2) | 105 (26.9) | 54 (13.8) | ||
| Likely (3) | 191 (49.0) | 248 (63.6) | ||
Regarding patient housing, CARE patients were more likely to receive pheromone therapy (P<0.001), and be accommodated in a ground-floor kennel appropriate to their size (P=0.011), but more unlikely to receive heating or cooling devices (P<0.001).
Concerning patient hygiene, CARE patients were more likely to receive bedding checks only one to two times a day (P=0.020). Registered veterinary nurses were also more unlikely or ‘neutral’ towards removing CARE patients' soiled bedding immediately (P<0.001). CARE patients were more unlikely to have abnormal discharge cleaned (P<0.001), less likely to be bathed after soiling (P<0.001), and less likely to be dried after bathing (P<0.001) and more unlikely to have vomit, regurgitation or excessive salivation cleaned (P<0.001).
During patient feeding, CARE patients were more likely to have stressors (such as noise) in the environment reduced (P=0.001) However, registered veterinary nurses were more ‘neutral’ in ensuring a CARE patient was not experiencing pain via pain scoring during feeding (P=0.004). CARE patients were also more unlikely to have time spent with them to encourage feeding if not eating (P<0.001) and more unlikely to have uneaten foods removed after a short period of time (P=0.002).
Regarding pain assessment, registered veterinary nurses were more ‘neutral’ towards assessing a CARE patient for signs of pain against all valid pain scale steps (P<0.001); instead CARE patients were more likely to be assessed for pain against only some steps of the pain scale (P<0.001).
Concerning exercise, CARE patients were more likely to be exercised only once a day (P=0.024). Non-ambulatory CARE patients were more unlikely to receive a ‘change of scenery’ (P<0.001).
Regarding restraint, registered veterinary nurses were more likely to use a basket muzzle on CARE patients during restraint (P<0.001), during intramuscular (IM) injections (P<0.001) and during phlebotomy (P<0.001). While registered veterinary nurses were less likely to use a tape muzzle on non-CARE patients during restraint compared to CARE patients (P<0.001), they were more likely to use tape muzzles on CARE patients during IM injections (P<0.001). Registered veterinary nurses were more likely to use dog catcher poles on CARE patients during restraint (P=0.001) and during IM injections (P<0.001). Registered veterinary nurses were additionally more unlikely to use distraction techniques when restraining CARE patients (P=0.022).
During temperature, pulse and respiration (TPR) checks, registered veterinary nurses were less likely to allow the CARE patients to sniff and familiarise themselves with the equipment used (P<0.001), this was also the case during intravenous (IV) medication administration (P=0.002) and during phlebotomy procedures (P=0.001).
However, registered veterinary nurses were more likely to have a CARE patient suitably restrained for a TPR check (P<0.001). Registered veterinary nurses were also more unlikely to take a CARE patient's heart rate for at least 15 seconds (P<0.001) and palpate the CARE patient's pulse simultaneously to ensure no pulse deficit (P<0.001). Registered veterinary nurses were more likely to observe a CARE patient's respiration rate from afar (P<0.001).
Registered veterinary nurses were more likely to open the kennel door slowly before administering IV medication at the port to CARE patients (P<0.001) but less likely to crouch to CARE patients' level (P<0.001).
Registered veterinary nurses were more likely to use basic commands with CARE patients when administering IM medication (P=0.025) but more unlikely to massage an IM site post injection on a CARE patient (P<0.001).
During phlebotomy procedures, CARE patients had a greater likelihood to have EMLA cream applied beforehand (P<0.001).
Open comments
Several similar themes occurred within the open comments segment. Participants stated that the level of care depends on time, staff levels (as more staff are reportedly needed for simple tasks and restraint with aggressive patients) and facilities available. Also highlighted was that each aggressive patient behaved differently in different situations. Minimal interference was important for some patients to avoid distress; thus nursing care should be adjusted appropriately. Participants also proposed that using the same staff with an aggressive dog was important to build trust, as they believed such patients behave better for designated nurses.
Many participants explained that minimal nursing care for aggressive dogs is in place for personnel and patient safety, thus there is little room to improve as a more holistic approach cannot be adopted because of the risk of injury. Personnel safety was considered a priority among all participants. Many registered veterinary nurses stated they could not provide ‘gold standard’ care if they could not get near patients safely.
Participants also addressed staff fear around aggressive patients, stating that predisposed ideas about aggressive patients mean they are treated differently. As a result, many registered veterinary nurses recognised patient hygiene, exercise and TPRs as a personal shortcoming of aggressive patient nursing.
Discussion
The results reveal several deficiencies relating to the nursing care of aggressive canine patients. One of the main nursing categories identified was maintaining hygiene. Literature shows that maintaining patient hygiene is essential to good nursing care, preventing infection in the clinical environment but also relating to patient respect (Peate and Lane, 2015), something identified as an indicator of good nursing by Burhans and Alligood (2010). While this literature explores hygiene in relation to human patients, these values relate to veterinary patients. Canine patients are largely dependent on veterinary care to maintain cleanliness and be provided with opportunities to toilet (Joiner, 2000). This places significance on this study's findings where aggressive patients were less likely to be bathed, cleaned, checked for soiling and frequently walked. This relates to a core nursing principle of holistic care by addressing individual patient needs (Joiner, 2000) and the Animal Welfare Act 2006 stating animal needs must be met by the person responsible for their care. However, there is a gap in guidance in regards to aggressive patients in the Animal Welfare Act 2006. Current legislation only extends to ensure the responsible person meets the animal's need to ‘exhibit normal behaviour patterns’. This starts a new conversation on whether aggressive behaviour can be defined as a normal behaviour pattern in response to fear in the veterinary practice, or whether it should not be defined as such in regards to the patient's normal behaviour outside the veterinary practice, therefore more effort should be made to minimise this fear response (aggression).
Some aspects of patient feeding were inadequate. Aggressive patients were less likely to have uneaten food removed; however, this is critical to avoid food aversion in hospitalised patients (Norkus, 2018). Adequate nutrition is essential to maintain body weight and promote healing in patients (Opperman, 2004).
Aggressive patients had poorer pain assessments overall in this study, as aggressive patients were less likely to be pain scored altogether. Pain scoring is vital as animals cannot self-report pain, thus it is the responsibility of the professional carer to identify and treat pain, although this is not fully applicable if significant personal health and safety risks present during assessment. However, the detrimental effects of pain must still be considered as pain has proven to impede healing and recovery, cause metabolic and endocrine derangements, and amplify physiological stress responses (Balakrishnan and Benasutti, 2012). Pain scoring is also relevant to nutrition. Sarrau et al (2007) proved that patients that received postoperative analgesia had improved feeding behaviours; therefore, by not pain scoring a patient, registered veterinary nurses risk compromising patient nourishment.
Basket muzzles were the most likely restraint aid to be used with aggressive patients; however, tape muzzles and dog catchers were also used. These results are important regarding ethical restraint of patients. The design of basket muzzles allows them to be safely left on the patient while allowing them to pant effectively, also lessening patient stress (Moffat, 2008). However, tape muzzles keep mouths forcefully closed, inhibiting fear-related panting (Moffat, 2008), causing further distress, leading to struggling and restricted airflow. The increased use of dog catcher poles is concerning as both Moffat (2008) and Johnson et al (2018) report these as dangerous and threatening to patients. The authors suggest the use of alternative restraint aids such as the basket muzzle, air muzzle, head collar, or alternatively, chemical intervention to reduce the stress and fear associated with restraint. Medication such as gabapentin administered prior to practice visits is proven to reduce fear (Bleuer-Elsner et al, 2021) and aggression in canine patients (Gupta et al, 2000).
Data showed aggressive patients were less likely to receive frequent out-of-kennel exercise. While patients are commonly walked for toileting, the opportunity for exercise and change of scenery are equally important, as outdoor access decreases abnormal behaviours (Beerda et al, 1999; Nogueira et al, 2021). The need for exercise is also considered a basic canine biological requirement (Hubrecht, 2002), important for a pet's mental and physical health (Shaw and Martin, 2014). A study by Meers et al (2004) demonstrated increased stress in dogs after ceasing a walking programme, while Shaw and Martin (2014) additionally state that walks decrease anxiety. Aggressive non-ambulatory patients were also more unlikely to receive a change of scenery, and environmental enrichment, all of which are essential for animal welfare and reducing stress (Burn, 2017), and are proven to provide a more pleasant, stimulating environment (Opperman, 2004). An effort should be made to routinely and regularly exercise aggressive canine patients. If registered veterinary nurses fear injury, then ‘double leading’ a patient so the patient is safely restrained could alleviate this.
Differences in care were also identified regarding TPR checks, IV and IM medication administration, and phlebotomy procedures. Aggressive patients were more unlikely to have their muscle site massaged post-injection. This is significant as Kanika and Prasad (2011) concluded massaging after an IM injection effectively reduced pain perception in human patients. Registered veterinary nurses were also less likely to crouch to an aggressive patient's level when administering IV medication. Although understandable as this puts nurses‘ faces at the height of a dog's mouth, Yelland and Whelan (2011) state that crouching down sideways to the patient can reduce perceived threat, as fear and anxiety are reduced. Registered veterinary nurses are attempting to make aggressive and non-aggressive patients more comfortable, as both were very likely to have EMLA cream applied before phlebotomy procedures. This is beneficial as EMLA has been proven to significantly reduce pain-associated behaviour in patients during cephalic and jugular phlebotomy (Leask, 2021). This improves nursing care and reduces aggressive behaviour, as pain is often associated with aggression (Camps et al, 2012).
Registered veterinary nurses explained that their nursing care depends on staffing levels, time, workloads and facilities. The author recommends that these different factors should be factored into practice diaries, ultimately allowing for more time for aggressive patients. Thompson-Hughes (2019) supports these comments, contributing busy work-load and understaffing within the veterinary hospital as to why registered veterinary nurses sometimes cannot supply the best standard of care. These reasons need to be considered as additional factors when assessing the quality of care in canine patients and tackled to improve patient welfare.
Many participants suggested minimal nursing care was adopted to prioritise nurse safety. This is understandable as a survey of veterinary science and nursing students by Wake et al (2006) revealed that 38% of respondents had been bitten by a dog and 13% of bite victims had severe psychological effects. Animal behaviourist Karen Overall identifies human safety techniques (such as restraint methods and restraint aids) as causing fear and depriving patients of choice (Overall, 2020). This highlights the importance of this study's findings, showing how prioritising personnel safety can lead to compromised aggressive patient welfare. This could explain the less hands-on approach seen in the survey data and comments. This is also reinforced by Lind et al (2017), as their study revealed that dogs perceived the clinical experience as negative against three different behaviour tests. However, this does not mean staff safety should be compromised for better nursing care, instead Overall (2020) seeks to identify ways to decrease the negative emotions experienced by veterinary patients, such as dog training methods and chemical intervention. Fortunately, registered veterinary nurses might be on the right path, as pheromone therapy (proven to reduce fear and stress in dogs (Levine et al, 2007)) is more likely to be used for aggressive patients, as is removing environmental stressors such as noise when feeding, using familiar commands and opening kennels with a slow approach.
Limitations
The sample population was recruited through self-selection. This introduced self-selection bias, where subjects' interest in participating perhaps involved inherent bias and desire to voice opinions (Sharma, 2017). Thus, the sample risked not being representative of the population. This method can also lead to snowball sampling which, while useful in recruiting participants, is not considered representative of the studied population, as participants recruit each other from similar demographic populations (Sharma, 2017). Nevertheless, this was beneficial to access hidden populations (Sharma, 2017), such as participants with limited online presence, ensuring better representation in turn. As the questionnaire was deployed to practices the author had contact with, convenience sampling was employed too. This sampling method does not allow the findings to be extrapolated to target populations (Jager et al, 2017). However, this ensured a higher rate of responses as more participants took part in the study (Emerson, 2015). By distributing questionnaires to reigstered veterinary nurses nationally through online social platforms, the disadvantage of geographical, socioeconomic and ethnic bias associated with convenience sampling was minimised (Emerson, 2015).
Future research
It would be beneficial to explore the nursing elements that have been identified as being of a lower standard for aggressive canine patients further, particularly how they impact canine welfare and health in more detail and to assess if recommended approaches to alleviate such shortcomings for aggressive patients are effective in a controlled, clinical environment.
Conclusions
This study provides evidence that aggressive canine patients receive a lower standard of nursing care than non-aggressive canine patients. Significant differences in nursing care were found under many nursing categories such as patient hygiene, exercise, patient restraint and attitudes to pain scoring and feeding, suggesting concerns for patient welfare. This project serves as an indicator for practices to examine their performance towards aggressive patients to ensure that despite limitations brought about by aggressive behaviour, standards of nursing care and patient welfare should not be compromised.
KEY POINTS
- Aggressive canine patients are more likely to receive lower standards of nursing care.
- The identified areas of compromised aggressive patient welfare include patient hygiene, nutrition, exercise, patient restraint and pain scoring.
- Veterinary practices should assess their own approach to aggressive patients under these identified areas to ensure good welfare for all patients.
- Veterinary practices should aim to accommodate and maintain personnel safety in their pursuit of improved patient welfare.


