Wound management in horses can be challenging, time consuming and expensive. Horses and ponies are presented to the veterinary surgeon and nurse with many types of traumatic wounds (Figure 1 and 2). Potential complications can occur depending on the anatomical position, degree of contamination and involvement of important structures such as joints, tendons and nerves, which can have a marked influence on the prognosis. In horses, involvement of joints and other synovial structures is extremely serious because if sepsis of these structures is not controlled with medical or surgical means, then non-weight bearing lameness can necessitate euthanasia. Careful evaluation and correct management of wounds is essential for an optimal result. Most wounds on the body of the horse heal well (Jacobs et al, 1984; Knottenbelt, 1997; Wilmink and Weeren, 2004), however, wounds involving the distal limbs can be difficult to deal with as horses often develop profuse exuberant granulation tissue in these wounds due to poor blood supply. The distal limb is also composed of mainly tendinous and ligamentous tissue, with minimal skin to create tension free closure of wounds, making it impossible to close due to excessive tension on the skin causing dehiscence.


Recent advances in understanding the processes in wound repair, provide the opportunity to actively manage wounds — dressings are applied that enhance the healing of the wound rather than just covering the wound. This has led to the production of a wide variety of dressings and bandaging materials. Correct selection of dressings is essential. This article aims to make the reader aware of some of the different dressings used in equine wound care, what properties different dressings (primary, secondary and tertiary layers) provide, and which may be most appropriate at each stage in equine patients with traumatic wounds.
What can stop or delay healing
There are 12 key factors which can inhibit healing of equine wounds. These are infection, movement, foreign bodies, necrotic tissue, continued trauma, paucity of blood supply, poor oxygen supply, poor nutritional and health status, local factors (e.g. dead space, tension, pH, desiccation or maceration), iatrogenic factors, genetic factors and cell transformation (e.g. sarcoid formation) (Knottenbelt, 2007). If any of these factors are present healing will be delayed. It is recommended that any wound that does not progress should have each of these factors assessed in turn. The dressing choice should take these factors into consideration.
Prior to choosing a dressing
Wound preparation and cleansing is one of the most important stages in effective wound management. Cleansing decreases bacterial contamination and removes necrotic debris. Always remember to wear gloves when treating a wound and, even more essentially, wash your hands with an antiseptic soap (e.g. chlorhexidine 4%) before and after treating the wound. This can protect the wound from further contamination from hands and will also help to protect hands from becoming colonized with bacteria, which may spread to another patient. Cleansing and debridement are not dealt with further in this article.
Factors affecting dressing choice
A number of factors affect dressing choice, these include anatomical location, level of contamination and infection, necrotic tissue, presence of a cavity and dead space, nature of the horse and management of the horse.
- Anatomical location — this can affect how the primary dressing will be kept in place. Areas such as the axilla and dorsum are difficult to bandage. Dressings can be attached to the horse using sutures and sticking the dressing in place with tape. Other options include Orthohorse bandages (Vet Options, ROI), which are commercial bandages designed for horses, or applying an extremely adhesive dressing over a primary dressing, e.g. Polster-Plast (Kruuse, UK).
- Level of contamination — some infected wounds will require dressings with antimicrobial activity, e.g. silver or honey dressings.
- Necrotic tissue — for example wounds where there are friction burns due to falling on tarmac, these wounds may need the dressing to aid in debridement for the initial stage, e.g wet-to-dry dressing.
- Presence of a cavity and dead space — this may lead to the application of a dressing that will conform well to the shape of the wound, or fill the dead space. The silver dressing Aquacel TM conforms well to wounds as it forms a gel. Intrasite gel (Smith and Nephew, London UK) is often used to pack wounds. If primary closure is possible, insertion of a penrose drain may be required, in which case an absorbant dressing would be ideal, e.g. Allevyn (Smith and Nephew).
Initial presentation of the equine wound
Horses and ponies are presented with many different wounds with different causes, (e.g. wire and kick wounds) ranging from a superficial graze to deep tissue damage with loss of substantial amounts of tissue.
Many wounds caused by trauma, whether they are full thickness or partial thickness, are commonly left to heal by second intention healing because primary closure has not been attempted or may not be possible. This inevitably leads to prolonged recovery time, and repeated dressing applications over several weeks.
When a wound heals by second intention healing, more scar tissue is formed which may lead to reduced function and poor cosmetic appearance, therefore primary closure (or delayed primary closure in many cases) should be attempted where possible. Debridement of the wound is used to convert a contaminated, traumatic wound into a surgical wound (Knottenbelt, 2007). The wound may need extensive debridement under general anaesthetic with sharp surgical debridement and/or hydrosurgical debridement. Dehiscence is common and may still occur, however, if some of the skin can be closed this will improve healing time (Figure 3a, b and c).

Stages of wound healing
Before choosing the optimum wound dressing it is important to understand the different stages of healing and it is also important to identify and correct any likely complications in the healing process.
Superficial wounds or partial thickness wounds rely on healing by migration of proliferating epidermal cells from the underlying epithelium and adnexal structures. Inflammatory cells are not prominently involved, in contrast to deeper or full thickness wounds.
In full thickness wounds: there are 3 key stages of wound repair.
The acute inflammatory stage:
The initial phase of healing of full thickness wounds is called the acute inflammatory stage. It begins the moment the injury occurs and is accompanied by formation of a blood clot within the wound bed. The inflammatory response is associated with redness and heat due to vasodilation, pain and swelling (oedema) of adjacent tissues. Inflammation is seen earlier in ponies and a healthy granulation tissue bed develops quicker, whereas the inflammatory response is less aggressive in horses and the granulation tissue can remain irregular and purulent for longer (Wilmink et al, 2004). In the inflammatory phase the dressing must assist debridement of the wound. There may be a large amount of exudate, therefore, the dressing will potentially need to absorb high volumes of exudates. If the wound is infected or heavily contaminated it would be helpful if the dressing can aid in controlling infection.
The cellular proliferation stage:
Cellular proliferation overlaps with the end of the inflammatory phase and can only continue if necrotic tissue and infection have been eliminated. In this stage granulation tissue is produced, angiogenesis occurs and epithelialization begins. Granulation tissue begins to develop 3–6 days after the injury has occurred, whereas epithelialization, a very slow process, begins within hours of injury (Theoret, 2005). Granulation tissue is a loose extracellular matrix containing fibroblasts and vessels which require minimal disruption by the dressing. Horses can often develop exuberant granulation tissue on the distal limbs, which may require repeated surgical debridement.
Matrix synthesis and remodelling:
The final stage of wound healing is matrix synthesis and remodelling; in an uncomplicated wound this occurs around 2 weeks after the initial injury (Theoret, 2005). The wound edges begin to contract and the granulation tissue is remodelled into mature scar tissue. At this point the dressing may be used to keep the wound clean from the environment and a minimally absorptive dressing is usually sufficient.
Primary dressings
Wet-to-dry dressings (adherent dressings)
The wet-to-dry technique uses adherent dressings to debride heavily contaminated or infected wounds aggressively. Although very cheap, due to the adherence to the wound these dressings can be painful to remove (Vermeulen at al, 2004), making their use limited. Consisting of woven gauze swabs applied directly to the wound they can be soaked in physiological saline to be used as a wet-to-dry dressing or on wetter wounds placed straight onto the wound after cleansing. In this case they are referred to as a dry-to-dry dressing. Although these dressings are frequently described in the literature, they are not used by the authors. A permeable, non-adherent dressing (e.g. MeloninTM; Smith and Nephew) should be used as a secondary dressing to prevent exudate soaking through to the absorbent cotton layer of the bandage. This allows removal of the overlying bandage without it sticking to the primary layer so that assessment prior to a controlled removal of the dressing can be achieved. The dressings need to be changed every 24 hours and removal may be painful. Once the wound has been debrided, this technique must be discontinued as further application of adherent dressings will have a direct detrimental effect on wound healing.
Foam dressings
Hydrocellular foam dressings are probably the most commonly used absorptive dressing in the management of equine wounds. Foam dressings (AllevynTM, Smith and Nephew; TielleTM, Johnson and Johnson) absorb excessive exudate while providing a protective barrier. They are available in different sizes and some have adhesive outer edges to help to keep the dressing in place. Foam dressings aid the process of moist wound healing and so encourage granulation and epithelialization. However, they are semi-permeable which means they can dry out if the wound does not produce any moisture. Foam dressings are often called passive dressings — they are not bioactive and do not debride the wound. They are therefore useful following hydrosurgical or sharp surgical debridement and in the cellular proliferation stage of healing where absorption of limited amounts of exudate is required.
Children's nappies
Children's nappies are extremely good at absorbing fluid and are useful in covering infected abdominal incisions of horses that have undergone exploratory coeliotomy. They can be useful in heavily exuding wounds where strike through of the bandage is difficult to control, but their shape is often awkward making them difficult to keep in place. Some commercial dressings, e.g. Eclypse™ (Dechra Veterinary Products Ltd.), use polyacrylate crystals (used in nappies) to provide high, nappy-like absorption in a sterile dressing. These may be easier to apply than nappies because of their more uniform shape.
Hydrogels
Hydrogels provide and maintain a moist wound environment. They donate fluid to the wound and can be used as a filler for a desiccated cavity where they can restore a physiologically sound moist wound healing environment. A wide variety of hydrogels are now available (Intrasite GelTM Amorphous Hydrogel dressing, Smith and Nephew; GranuGEL® Gel, Convatec) (Figure 4), each has its own benefits and drawbacks. Some adhere better to fresh wound surfaces than others, but not all have the same moisture donating properties. Some are also able to absorb moisture and so can be used to assist with moisture control. Most hydrogels will aid debridement of necrotic wounds (Flanagan, 1995) and may also have a bacteriostatic effect due to the presence of propylene glycol. Propylene glycol also acts as a humectant which prevents the gel drying out. This means that as an emergency measure hydrogels are useful primary wound cover since they will support the developing wound bed and appear to control the proliferation of most bacteria. However, they should not be thought of as antimicrobial dressings.

Hydrofibre
Aquacel® hydrofiber dressing (Convatec) is a soft, woven pad of carboxymethylcellulose. This dressing provides a moist wound environment as it transforms into a soft gel substance when brought in contact with the wound bed through absorbing exudate. It aids in the debridement of the wound without causing damage to viable tissues. Aquacel® is available with impregnated ionic silver which is marketed as Aquacel Ag®. With Hydrofiber® dressings a secondary dressing, e.g. a hydrocellular foam dressing, is required to keep them in place and prevent loss of fluid.
A new gelling foam dressing with a Hydrofiber® layer, called Versiva® XC® (Convatec) is the latest generation of hydrofibre dressings. It is indicated for moderate and highly exudating chronic and acute wounds. No secondary dressing is required with Versiva® XC®.
Hydrocolloids
Hydrocolloids are a suspension of gelatin, pectin and sodium carboxymethylcellulose, which are held in an adhesive polymer matrix. These dressings provide a moist environment for the wound without causing maceration and were originally designed to soften necrotic tissue to aid in natural debridement in human health care. They are said to promote angiogenesis and fibrinolysis, therefore they are useful in the proliferation stage of wound healing. As the exudate from the wound is absorbed into the dressing, it forms a gel which is held in place within the wound. GranuflexTM (Convatec) is a hydrocolloid dressing which has a thin semipermeable/breathable polyurethane film to provide a microbial barrier.
Silver dressings
Silver has an antimicrobial effect against many types of bacteria and has been used to manage infection in wounds and burns for the last 40 years (Beam, 2009). Various types of silver dressings are available. ActicoatTM (Smith and Nephew) is a nanocrystalline silver dressing which requires soaking in water (not saline) for 10 seconds before applying to the wound to activate the silver ions. ActicoatTM has been shown to have good antimicrobial effect against a variety of wound pathogens and is useful in the early phases of wound healing (Fong and Wood, 2006). However, the physical use of the dressing is limited by its non-conforming character. Aquacel AgTM is a Hydrofiber® dressing containing ionic silver, which does not need pre-soaking. It can, however, be applied dampened and then conforms well to the application site.
Antiseptic creams containing silver sulphadiazine are also available, e.g. FlamazineTM 1.0% cream (Smith and Nephew). These can be used on partial or full thickness wounds.
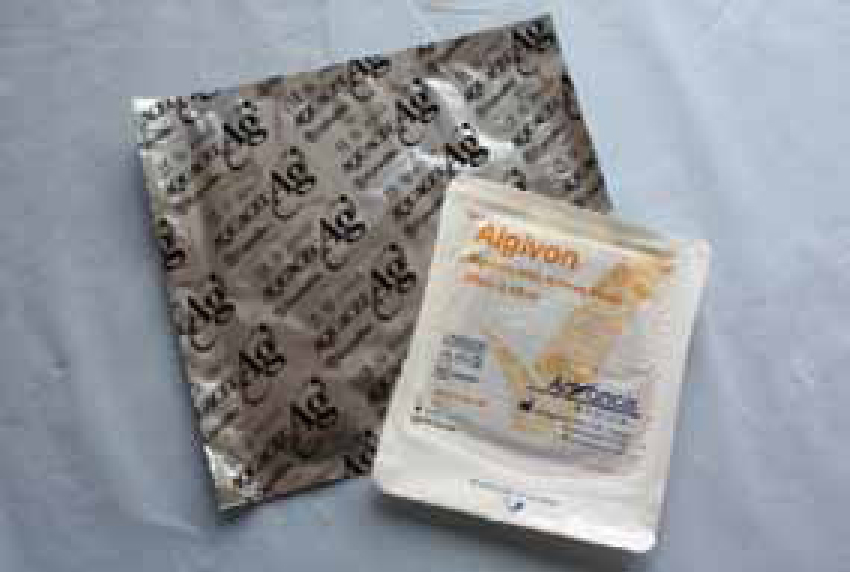
Alginates
Alginate dressings are fine, fibrous dressings that absorb exudate. Originally they were intended to provide haemostasis (Anderson, 2003). The haemostatic properties of alginate dressings vary according to how they are manufactured. Alginates form a gel as they absorb exudate, which provides a moist wound environment. However alginates should not be used on dry wounds as the fibres may irritate the wound and there is real risk of wound bed desiccation. Alginate dressings actively stimulate granulation tissue formation through the release of calcium ions, therefore caution should be used when applying these dressings to wounds on the distal limb of the horse, where excessive granulation tissue is problematic (Hollis, 2008). Available alginate dressings include Algosteril TM (Beiersdorf Medical, UK), Algisite M TM (Smith and Nephew) and KaltostatTM (Convatec). AlgivonTM (Advancis Medical, Nottinghamshire, UK) is an alginate dressing with ActivonTM (medical grade Manuka Honey). AlgivonTM is a nonadherent dressing which is effective against a broad spectrum of bacteria. New combinations include alginate and silver, which again has a broad spectrum antimicrobial effect. A secondary dressing is usually applied when using alginate dressings.
Honey dressings
The use of honey in wound management has been documented since 2000 BC (Dunford et al, 2000) and its merits are well appreciated.
Manuka honey is formulated into medical grade honey, which has prolonged antibacterial effects. It has debriding, antimicrobial and some anti-inflammatory and antioxidant properties. Normal honey is not recommended as wound exudate dilutes it quickly, and the dilution reduces the antibacterial effects (Knottenbelt, 2010) (Figure 6).

Secondary layer
In horses the secondary layer is important to keep the primary dressing in place (Soffban, Smith and Nephew, London, UK) and provide protection and absorption of exudate, as well as preventing movement of the wound.
Polyester orthopaedic padding
Common brands used are Soffban (Smith and Nephew, London, UK) or Orthoban (Millpledge, Nottinghamshire, UK). These are light, polyester bandage which are applied over the primary dressing to keep the dressing in place and provide some padding. In distal limb bandages this is always covered by cotton wool or gamgee (Figures 7 and 8).
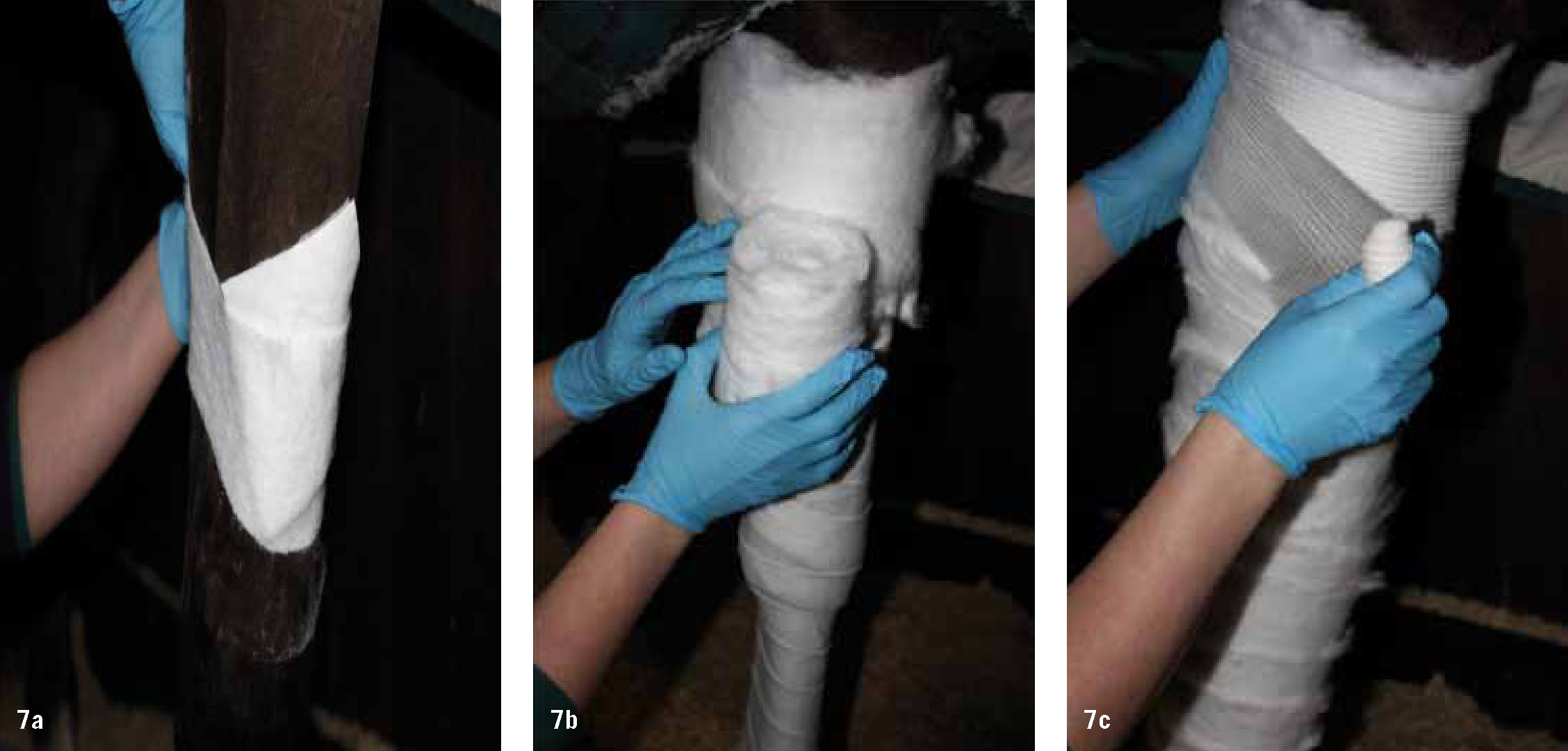

Absorbent cotton (formerly known as cotton wool) or Gamgee:
This is usually used as a protective and absorbent tertiary layer over a wound site. It provides effective cushioning and protection from external challenges. However, it is also thermally insulating. Evidence of strike-through (exudates appearing at the surface of the dressing) indicates that the wound is highly exudative. If strike through is detected on the outer most layer of the bandage then the bandage should be changed.
Tertiary layer
Absorbent cotton has no elasticity or tensional strength, therefore it is usual to apply a knitted conforming bandage (Knit-fix, Millpledge, Nottinghamshire, UK) over the cotton layers and then a flexible cohesive bandage (Co-Plus, BSN medical, East Yorkshire, UK; Vet-Flex bandage, Kruuse) over the knitted conforming bandage. Absorbent cotton is also the basis of the movement limiting Robert Jones dressing in which several layers of the material (cotton) are used with knitted conforming bandages. The horse can be splinted additionally (Figure 8d) or sometimes casting material (Dynacast P, BSN Medical, East Yorkshire, UK) is placed over 3 layers of cotton wool and knitted conforming bandage, then an outermost flexible cohesive layer to produce a bandage cast. Once set, the casting material can be bi-valved (lateral and medial divides with a cast saw) and then the bandage changed underneath to examine the wound. The cast material can be taped on over a new bandage to provide support using duct tape in circular movements from the top of the cast material to the bottom.
PolsterPlast (Kruuse) is a cross-elastic cohesive foam fixative that can be used to secure dressings where bandage is impossible to apply, e.g. the dorsum or gluteal region.
OrthohorseTM
OrthohorseTM bandages produced by Vet Options (ROI) are specially designed, adjustable Elastic wraps which can be purchased to keep primary dressings in place in difficult areas to dress, such as the axilla or abdomen (see Figure 1). These are washable and reuseable, with Velcro fastenings to ease application and removal.
Conclusion
Wound dressings should be used to actively manage the wound and chosen according to the nature of the wound and stage of healing. Many advanced dressing products are available on the market, which incorporate and combine new technology and are developed due to ongoing research into wound repair.
Key Points
- Wounds on the body of the horse heal well, however wounds in the distal limbs can be difficult to manage.
- Many dressings are available — take into account stage of wound healing, anatomical location, level of contamination and necrotic tissue, presence of a cavity or dead space, and management and nature of the horse when choosing a dressing.
- Wet-to-dry dressings are cheap and debride the wounds well, however can be painful to remove.
- Hydrocellular foam dressings are the most commonly used primary dressing in horses.
- Foam dressings are not bioactive and do not debride the wound.
- Children's nappies are extremely good at absorbing fluid, but due to their shape can be difficult to conform to the body to cover the wound effectively.
- Hydrogels provide and maintain a moist wound environment and are useful when there is a large cavity.
- A new gelling foam dressing with a Hydrofiber layer is available, which can be used in acute or chronic wounds with moderate to heavy exudates, and a secondary dressing is not required to absorb exudate, only to keep it in place.
- Manuka honey and silver dressings have antimicrobial properties.
- Alginate dressings are used when excessive granulation tissue is problematic.

