Advances in the veterinary field are driving changes taking place within the nursing curriculum. As a result the role of the registered veterinary nurse (RVN) has changed to meet the needs of this advancing profession. There are now an abundance of specialised areas in which the veterinary nurse can study. A nurse's job involves anything from advocating for their patients, counselling the owners, data analysis, anaesthesia, radiography to most importantly caring for their patients in a systemic and holistic manner (Barrett et al, 2009). The role of a specialised surgical nurse involves caring for their patient before, during and after surgical procedures. This is a huge responsibility and all aspects of the patient's care should be taken into consideration when planning the treatment. It is part of the nurse's role to evolve the care given, as the patient's needs change throughout the procedure (Carpenito-Moyet, 2009). This also emphasises the importance of the surgical nurse's knowledge in a wide range of surgical procedures.
To provide this key aspect of nursing it is important that the nurse chooses a suitable model of nursing and follows the nursing process (Barrett et al, 2009). This is significant as it aids the nurse in collecting accurate information and highlights any problems that need to be dealt with. The nursing process involves four fundamental parts which are assessment, planning, implementation and evaluation. The model of nursing provides the framework through which the nursing process may be applied. Once this phase is completed a nursing care plan (NCP) can be drawn up. Carpenito-Moyet (2009) states that as the nurse intervenes and continues to assess the patient, additional goals and interventions can be added to the plan. This enables the care plan to evolve with the patient.
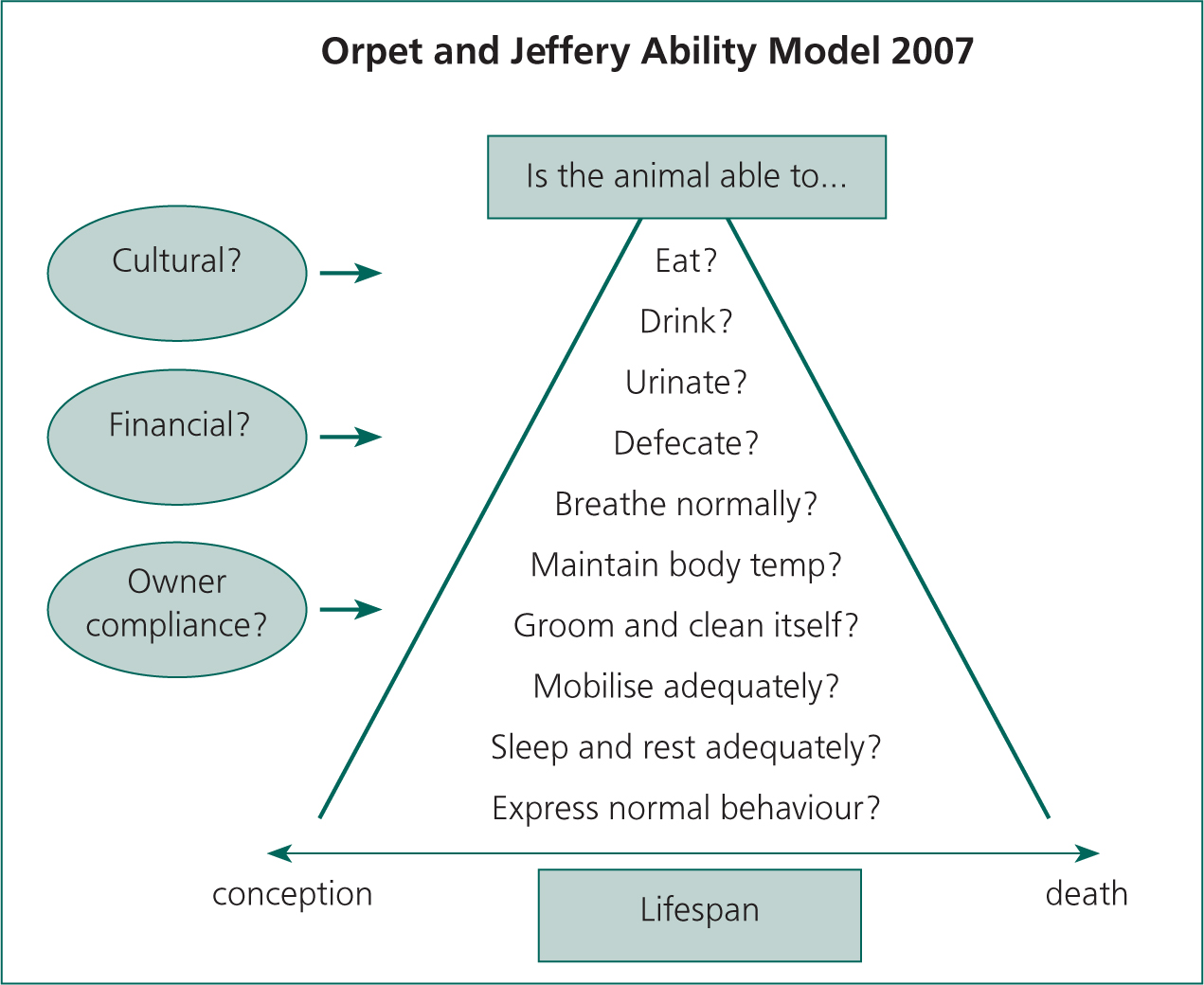
The Ability Model is the chosen model for the following case study that follows (Orpet and Jeffery, 2007). This is an adaption of the human model by Roper, Logan and Tierney (RLT) (1996). The Ability Model was constructed in 2007 by Hilary Orpet and Andrea Jeffery, both qualified veterinary nurses. This model was chosen for its holistic nursing approach as it focuses on assessing ten aspects of the patient's life. It helps improve nursing skills and involves a high standard of care to the patient as it is systematic and logical to follow. It was also chosen because it can be adapted for each patient and enable several nurses to use it as the patient care progresses from surgical to postoperative.
Relevant history and clinical presentation with diagnosis
The patient was a 12-year-old, male neutered, 5.3 kg domestic short-haired cat. A clinical examination revealed weight loss of 0.2 kg, polyphagia, and a palpable goitre. He was tachycardic, with a heart rate of over 200 beats per minute (bpm) (normal heart rate for cats 110–180), but no arrhythmia. He was diagnosed with hyperthyroidism. Differential diagnoses for the above are diabetes mellitus, renal disease, bowel disease, cardiomyopathy and primary liver disease (Neiger and Liebig, 2005). There was no previous relevant history.
The patient was booked in for a bilateral thyroidectomy after stabilisation of his condition on antithyroid medication carbimazole (Vidalta, Intervet). His clinical examination revealed tachycardia, poor body condition, and polyuria. His pre-operative bloods revealed no abnormalities. His total T4 was within normal range. A full body condition score (BCS) and muscle condition score (MCS) were not carried out at the time of examination, but this would have been beneficial.
Pathophysiology and nursing assessment
Hyperthyroidism is a multisystemic disorder resulting in excessive production of the thyroid hormones tri-iodothyronine (T3) and thyroxine (T4). The primary cause of the condition is benign hyperplasia of the thyroid gland. Peterson (2000) stated that around 70% of cases involve bilateral enlargement of the thyroid lobes and only 3–5% have a malignant thyroid tumour. Caney (2004) outlined that the excessive circulating hormones have a catabolic effect, resulting in increased metabolic rate, gastrointestinal motility, cardiac output, central nervous system activity and heart rate, a decrease in sleeping pattern and a reduction in bodyweight.
Clinical signs are weight loss, muscular weakness, tremors, heat intolerance and intermittent fever, central nervous system abnormalities such as hyperactivity, nervousness and aggressiveness. This is supported by Garnett (2008) who outlined further clinical signs such as an unkempt coat, polyphagia, and cardiovascular features such as tachycardia, vomiting, diarrhoea, goitre and tachypnoea.
The Ability Model was used for the assessment. The Ability Model involves ten aspects of the patient's life to be assessed (Figure 1). This model highlights the patient's individual needs and how these can change throughout a procedure. Nursing interventions can then be placed on the care plan to prevent potential problems (PPs) from occurring. Having the NCP in place increased the understanding and knowledge of the patient's condition and stage of disease, and using the nursing process and nursing models, utilises the VN's knowledge and skills. An actual problem (AP) highlighted pre-operatively was low bodyweight which could result in the PP of hypothermia during surgery (Martinez, 2008). The short-term goal for this was to reduce heat loss. The long-term goal was to return the patient to their original body condition. The nursing interventions (NIs) put into action were regular temperature checks, twice daily pre-operatively, with the cattery being kept at an ambient temperature, which in a ward is 18–21°C. The thyroid's effect on the thermoregulatory system also increases the risk of hypothermia (Martinez, 2008). This was addressed by using bubble wrap and a foil blanket to reduce heat loss during the surgical procedure, as well as heat pads placed underneath the patient. The NIs of temperature checks were increased to every 10 minutes during surgery and immediately postoperatively.
Another AP that was highlighted was polyuria. The PP of this would be dehydration. The specific gravity was assessed as this measures the urine's concentration. The patient's specific gravity was 1.008, which was low, indicating polyuria, compared with the normal value for cats which is 1.035–1.060. Polyuria may have occurred because of concurrent primary renal dysfunction, decreased renal medullary solute concentration, electrolyte imbalance or may be in compensation for polydipsia, which occurs as a result of hypothalamic disturbance associated with thyroid hormones (Mooney and Peterson, 2004). Renal parameters must be checked as hyperthyroidism increases the glomerular filtration rate (GFR), which may mask mild pre-existing renal failure in some patients (Caney, 2004). Following control of hyperthyroidism, the GFR may fall precipitating a significant deterioration in renal function (Scherk, 2009). This is one indication why stabilisation of a patient prior to surgery is pertinent.
Polyuria is likely to lead to polydipsia so it was important not to withdraw fluids too early preoperatively; 2 hours was adequate for this patient. The NIs were to measure water amounts and urine output four times daily, skin turgor and a pre-operative blood sample to check packed cell volume, renal and T4 levels. The calcium level was also checked pre-operatively as there could be accidental damage to the parathyroid during surgery. The short-term goal was to prevent dehydration, which was maintained by administering intravenous fluids at a rate of 2 ml/kg/hour pre-operatively and 3 ml/kg/hour peri-operatively. The long-term goal was to determine the cause of the polyuria. Results from all blood analyses were within normal parameters.
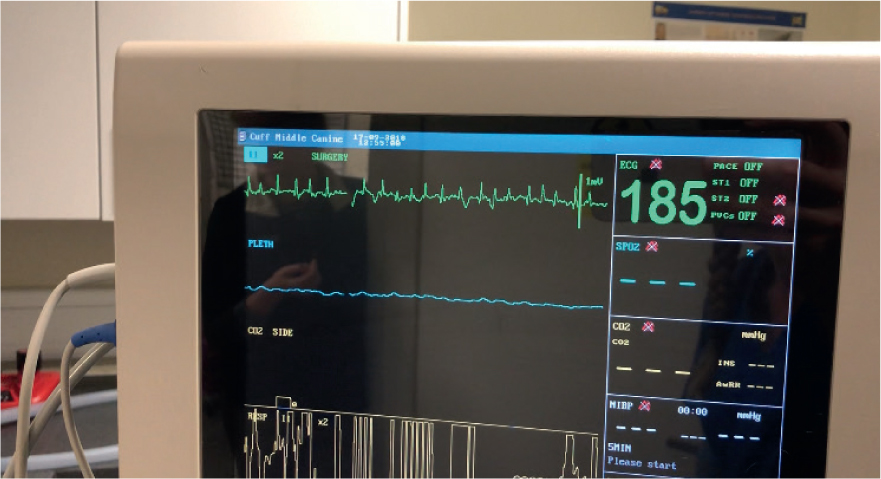
Another highlighted AP was tachycardia. The PP of this would be anxiety and stress leading to an increase in circulating catecholamines, which have a detrimental effect on cardiac function. The PP of this would be a further increase in tachycardia and potential arrhythmias. Hyperthyroidism causes cardiac abnormalities which affect the sympathetic nervous system, and may result in a hypertrophic cardiomyopathy, increasing myocardial oxygen demand (Martinez, 2008). If the demand is not met the likelihood of arrhythmias increases and fatalities can occur (Mooney and Peterson, 2004). The patient's stabilised euthyroid state helped to reduce the anaesthetic risk. The NIs put in place were hourly monitoring of heart rate (HR) and rhythm, respiratory rate (RR), capillary refill time and mucous membrane colour and minimal handling pre-operatively. This was increased to every 5 minutes peri-operatively and in the immediate postoperative period, returning to hourly once the patient was out of the recovery area. This was further reduced to every 4 hours the next day for the duration of the hospitalisation. No arrhythmias occurred during the surgical procedure but the patient did remain tachycardic.
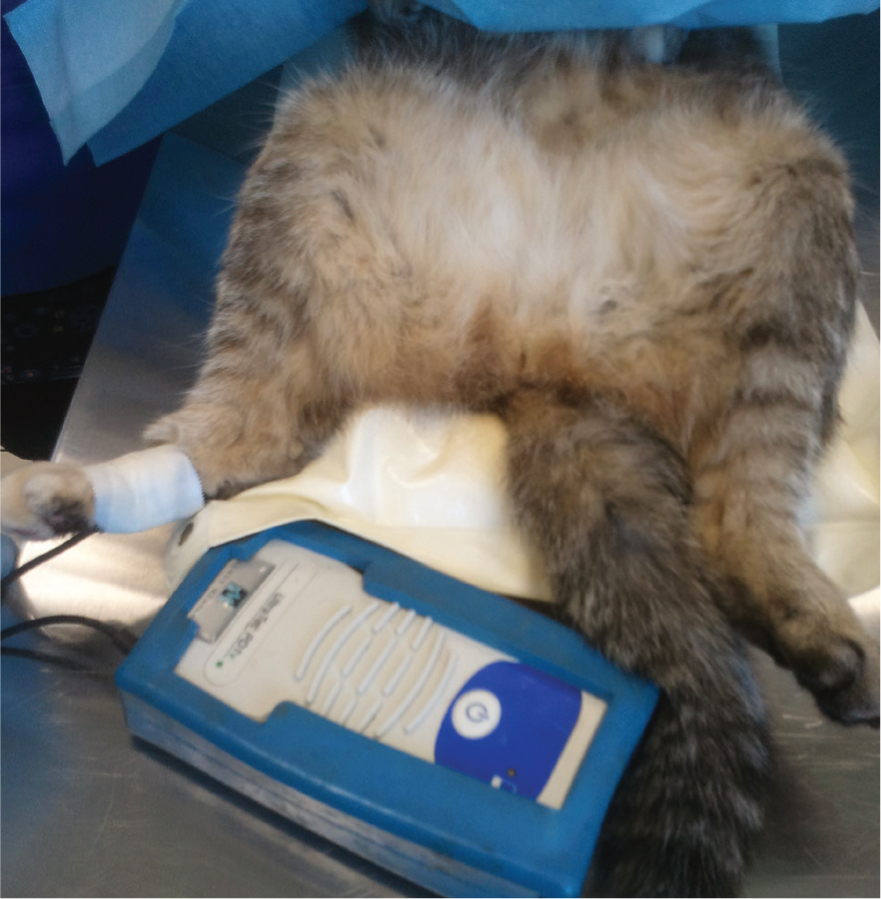
Electrocardiogram (ECG) (Figure 2) can be used to monitor for cardiac problems throughout the procedure. This measures the electrical impulses of the heart and provides readout of the heart's activity. If an abnormality is observed, the ECG can be readily recorded for further analysis. Blood pressure was also monitored. Blood pressure is the pressure exerted by blood on the wall of a blood vessel and is made up of a systolic and diastolic component. This is measured using an inflatable cuff on the leg that automatically cycles through taking readings so that any changes in the pressure can be tracked during surgery. If an abnormality is observed, measures can be taken to correct it. This is connected onto the multi monitor and takes readings throughout the procedure. If a multi monitor is not available a Doppler (Figure 3) can be used by clipping the plantar area, then gel can be applied. The Doppler should be taped to the plantar area then turned on to ensure the pulse is audial. The normal blood pressure for anaesthesia is 60–100 mmHg. The patient was slightly above this throughout the procedure.
Intra-capsular bilateral thyroidectomy
The surgery performed was an intra-capsular bilateral thyroidectomy. This removes the abnormal tissue without compromising the parathyroid glands (Caney, 2004). Special equipment used was small iris scissors and Bishop Harmon thumb forceps; these are used for their precise nature and facilitate removal of the thyroid glands (Fossum, 2007). The surgical nurse's roles within this procedure involved preparing the patient, moving through to theatre, preparing the equipment, comprehensive monitoring, anaesthesia, fluid management, blood monitoring of electrolytes, acid–base balance, administering pain relief and antibiotics (Tracy, 2000). A surgical scrubbed nurse would assist in instrumentation management for the veterinary surgeon and help with positioning of instruments in the sterile area (Tracy, 2000). The surgical procedure went well with no serious problems arising.
Hughes (2008) stated that the heart is less able to compensate for adverse cardiovascular events, hence why it is imperative that the drug selection is mainly based on the minimisation of cardiac depression. Drugs avoided were those that stimulate adrenergenic activity, inducing tachycardia and arrhythmias. These include atropine and alpha 2 agonists such as medetomidine which sensitise the heart muscle to adrenaline. The premedication selected was a neuroleptanalgesic combination of acepromazine (ACP 2 mg/ml, Novartis Animal Health) and buprenorphine (Vetergesic 0.3mg/ml, Alstoe Animal Health). Hyperthyroid patients are very anxious because of increased catecholamines within the body; the premedication utilised the drug synergism and created an anxiolysis effect.
Medetomidine was avoided because it causes depression of the cardiovascular system despite the benefits of easy handling and reversibility (Stein, 2004). Ketamine was not used as it is contraindicated in hyperthyroid patients because of increased sympathetic tone and myocardial oxygen consumption leading to an increased risk of arrhythmias and hypertension (Veterinary Anaesthesia Support Group (VASG), 2004).
The patient's blood pressure remained hypertensive at 120 mmHg throughout the procedure. A good supply of oxygen was administered throughout the anaesthetic and also preinduction by mask. This was monitored with a pulse oximeter (Figure 4), which measures the oxygen carrying capacity of the blood. The instrument uses an infrared light to measure the transparency of the blood cells and reports the oxygen content as a percentage. It also measures the heart rate.

This, as stated by Martinez (2008), helps prevent episodes of hypoxia and associated arrhythmias during anaesthesia. Profound analgesia was met with the administration of buprenorphine, which is shorter acting than morphine, aiding a quicker recovery alongside the non-steroidal anti-inflammatory drug meloxicam (Metacam 5 mg/ml, Boehringer Ingelheim Vetmedica). Isoflurane (Isoflo, Abbott Laboratories) was used because of its beneficial antiarrythmogenic properties compared with other inhalation agents (Stein, 2004).
Postoperative problems
The most common complications that may occur from the surgery are:
- Hypocalcaemia as a result of damage of the parathyroid glands
- Hypothyroidism
- Recurrence of hyperthyroidism
- Worsening of renal disease
- Horner's syndrome
- Laryngeal paralysis
- Wound infection.
An AP postoperatively was hypothermia. The PP of this would be a slower recovery. Hyperthyroid patients are quite small and they have a larger surface area to bodyweight ratio, poor body condition and less subcutaneous fat. This increases the susceptibility to hypothermia during anaesthesia. This was well planned for in this patient's case by the use of heat pads pre-operatively. The NIs added to the care plan, were 10 minute temperature checks, and extra thermoregulatory treatment was administered with hot hands as well as heat pads, bubble wrap and blankets. The patient was marginally hypothermic at 36.6°C. Hypothermia can slow recovery in patients (Martinez, 2008) but the patient's temperature returned to normal 1 hour into recovery.
Another postoperative AP was seeping of blood from the wound. The PP of this was swelling that could lead to upper airway obstruction (Martinez, 2008) and could also put pressure on the parathyroid glands thus affecting their function and resulting in hypocalcaemia. The other PP of this would be haemorrhage. The NI was observation every 10 minutes of the wound area and monitoring of the patient's respiratory effort and rate (normal rate is 20–30 breaths per minute), mucous membrane colour and capillary refill time. This was reduced to 4 hourly checks of the wound. The short-term goal was to prevent haemorrhage. The long-term goal was to achieve suitable wound management and prevention of infection or swelling. The wound management worked well in this case and no complications occurred.
A complication of bilateral thyroidectomy is hypocalcaemia. Clinical signs are usually noted 24 to 96 hours postoperatively (Fossum, 2007). Taking this into consideration the NIs added to the care plan were monitoring for signs of calcium deficiency. These include panting, nervousness, facial rubbing, muscle twitching, ataxia and eventually seizures (Mooney and Peterson, 2004). Another NI was blood analyses to check calcium levels 24 hours and 48 hours post operatively. NIs that were continuous throughout the stay were feeding three times daily and once daily kennel cleaning.
Post-discharge evaluation
On discharge the owner was given a home care plan (HCP) to observe for signs of calcium deficiency and also renal disease. A home care plan helps in the continuation of the patient's care and enables the owner to facilitate in their pet's recovery in their home environment. This allowed the veterinary team to continue stabilising the patient without the stress of the practice environment. The NCPs and HCPs ensured a continuity of care following discharge, and enabled the owners to help in their pet's recovery from disease in a structured way. The early signs that the owner was told to look for were lethargy, anorexia, panting and facial rubbing (Fossum, 2007), along with increased thirst and urination. The owner was also responsible for wound management; if there were any signs of heavy weeping or discharge they were instructed to return to the surgery. It is extremely important that the owners have a bond with the veterinary team to ensure that they phone when instructed and feel comfortable speaking to staff if they need to. It is also important to remember that not all owners would be able to cope with the responsibility of care for their pets, so it is part of the veterinary nurse's job to evaluate this. Sometimes it is in the patient's best interests to stay hospitalised a little longer (Carpenito-Moyet, 2009). A care plan at home helps the owner feel as if they are facilitating in their pet's recuperation.
The nursing care plan
The use of a NCP is important as the needs of the patient change constantly when involved with any surgical procedure. The NCP helps highlight PPs that might occur and changes to the patient's condition. If followed correctly, NCPs work well in practice ensuring the patient is closely monitored with appropriate treatment and changes promptly noted. Without reassessment and alterations to the NIs the patient care may be compromised. Care plans in practice and at home allow all members of staff and owners to monitor progress and potential risks to the patient, and they are essential in the patient's progression. The care plan worked well in the above case because of the constant reassessment of the patient and the accurate information collected in the first assessment. Davis' (2006) case study noted a similar outcome as a result of an in-depth patient assessment guided by a model of care. This shows the importance of holistic nursing care rather than a disease-oriented approach. Davis (2007) outlined that the collaboration of important information allows the veterinary nurse to highlight the AP and PP unique to that patient before formulating a NCP, suggesting that this care plan will only be as good as the information and assessment performed.
The weakness of this case was the time constraints imposed on the nurses to complete the paper work and administer care. The practice was short staffed and the Ability Model was found to be extremely time consuming. This disadvantage has often been highlighted in the past for other types of models of nursing. Timmins and Horan (2007) supported this by stating that the RLT Activities of Living Model for Nursing is a paper exercise and is criticised for its excessive documentation.
The NCP has highlighted that it does influence the after care and home care, but it is difficult to say whether it works in a surgical procedure. The time observing and caring for the patient that is required with surgical procedures, makes it difficult to find time to fill out all of the ten abilities. This procedure went well and no complications arose yet further NIs could have been added to improve the care throughout this case. Bair huggers are a warming blanket system that improve patient care by continually warming the patient throughout a procedure. This would have been a benefit in this case as well as undertaking a full BCS and MCS pre-operatively. Another added pre and postoperative check that would have benefited the patient would through checking his hydration status by regular weight checks to track fluid loss or gains.
Conclusion
This case reflects, not only the importance of NCPs in practice, which highlights problems before they deteriorate, but it also reflects the importance of HCPs. The case above suggests that the NCP may work better in some surgical procedures than others. It was felt by the author that their place in routine operations would not work because of the time constraints that are linked to the NCP but would benefit more complicated and higher risk surgical procedures as these present a multitude of risks. This would enable staff to ensure that the right care is given with the changing needs of the patient from admission through to discharge. NCPs play an important part in helping the surgical nurse facilitate a more systemic, holistic approach to patients. Specialising in surgical or medical areas improves the nurse's knowledge in procedures, which results in a higher standard of care.
KEY POINTS
- Nursing care plans (NCPs) should evolve with the patient so that veterinary nurses continually evaluate and implement different care throughout.
- A care plan at home helps the owner feel as if they are facilitating in their pet's recuperation.
- Complications that may occur from the thyroidectomy surgery include hypocalcaemia, hypothyroidism, and recurrence of hyperthyroidism, worsening of renal disease, Horner's syndrome and laryngeal paralysis, and wound infection.
- NCPs in practice highlight problems before they deteriorate; and also reflect the importance of the home care plans.
- NCPs play an important role in surgical nursing, facilitating a more holistic approach to patients.


