Fleas (Siphonaptera: Pulicidae) are the most important ectoparasites on domestic dogs and cats worldwide (Blagburn and Dryden, 2009), except in northern Scandinavia where the louse is predominant. Figure 1 shows a cat flea (Ctenocephalides felis), the dominant flea species in the UK, which causes flea infestations of dogs and cats. In Ireland the dominant species on dogs is the so-called dog flea Ctenocephalides canis. Besides causing discomfort to pets and their owners through biting, fleas cause flea allergy dermatitis (FAD) and act as vectors for a range of human and animal pathogens, such as Bartonella and Rickettsia species (Barrs et al, 2010).

FAD is described as a common cause of skin disease in dogs and cats (Scott et al, 2001). Most FAD cases occur in the late summer, corresponding to the peak of flea populations, although in warm climates flea infestations may persist throughout the year. Utilizing the diagnostic, treatment, and preventive recommendations outlined in this paper should allow for improved outcomes for a common and serious medical complication seen in dogs and cats infested with fleas.
Pathophysiology of FAD
When feeding, fleas inject their saliva, which contains a variety of histamine-like compounds, enzymes, polypeptides, and various amino acids. These immunogenic (allergenic) molecules exhibit unusual immunologic properties and have the ability to induce distinct skin test reactions in the sensitized animal. When first exposed to flea bites (flea saliva) the animal will not react. However, with repeated exposure a proportion of animals will develop a hypersensitivity response. A dog’s hypersensitive immune reactions to the antigens present in flea’s saliva bear the hallmarks of Type I (immediate), Type IV (delayed), and cutaneous basophil hypersensitivity reactions. Type I hypersensitivity is a humoral response that occurs in a few minutes. It is triggered by immunoglobulin E binding to mast cells, leading to the release of inflammatory mediators, such as histamine. Type IV reactions are cell-mediated and involve interactions of T lymphocytes. Release of numerous lymphokines results in the release of pruritogenic inflammatory mediators. Basophil hypersensitivity is a transient delayed-type reaction in which basophils comprise the principal cell population. This sequence of reactions occurs constantly in the flea-allergic dog while it is exposed to flea bites, and can be used as a diagnostic aid in skin tests.
Pruritus represents one of the most prominent signs in FAD and numerous dermatological and systemic disorders. The pathophysiology of pruritus is diverse and involves a complex interaction of cutaneous and neuronal cells, and specialized skin nerve fibres (Metz et al, 2011). Apart from histamine, several allergy mediators and receptors, and inflammatory cytokines have been identified as playing a role in the pathophysiology of pruritus. In the skin, tissue resident cells and tissue inflammatory cells have been found to interact with neuronal cells using effector molecules and regulatory pathways for the modulation of pruritus.
The pathophysiology of FAD in cats has been the subject of less research; however, similar mechanisms may exist (Lewis et al, 1999). More understanding of the pathogenesis of FAD is needed before vaccination or immunotherapeutic intervention is likely to be successful.
Risk factors
The initial development of FAD as an allergic response and subsequent manifestation of clinical signs depends on exposure to flea bites. Once developed there is a threshold level of exposure for an individual animal, hence an owner is unlikely to see clinical signs of FAD until the cumulative number of bites (number of fleas x time) exceeds the threshold, by which time the flea infestation is likely to have established in the home.
Importantly, FAD is more frequently observed in dogs that are intermittently exposed to flea bites than dogs that are continuously exposed to fleas. This immunologic tolerance (i.e. a state of systemic hypo-responsive ness to an antigen) in chronically infected dogs is due to low level of circulating IgE and IgG anti-flea antibodies, and these animals generally do not develop skin reactions or develop them later and to a considerably lesser degree (Halliwell, 1984; Halliwell and Longino, 1985). Hence, circumstances which permit intermittent flea challenge (e.g. interrupted or irregular flea treatment) and increased level of these antibodies are more likely to result in the development of FAD.
The clinical spectrum of FAD is variable and is determined by the frequency of flea exposure, which in turn determines the amount of saliva entering the body. Additional contributing risk factors include the duration of disease, presence of secondary or other concurrent skin diseases, and degree of hypersensitivity. Hence, non-allergic animals may exhibit few clinical signs other than occasional scratching due to irritation caused by flea bites. In contrast, allergic animals will have a dermatitis that is characterized by pruritus, which can be intense and may manifest over the entire body.
Clinical signs
In dogs: clinical signs are papulo-crustous lesions distributed on the lower back (Figure 2), tail-head, and posterior and inner thighs. Affected dogs are restless and uncomfortable, spending much time scratching, licking, rubbing, chewing, and nibbling at the skin. As clinical disease progresses the affected areas become alopecic, lichenified, and hyper-pigmented, and the dog develops secondary bacterial and yeast infections. In extremely hypersensitive dogs, extensive areas of alopecia, erythema, and self trauma are evident.

In cats: the most classic flea lesion associated with allergy has been miliary dermatitis — focal, small 1–5 mm, papules which become crusted. The lesions are typically found on the back, neck, and face. These lesions are not specific for flea allergy as they are also seen with atopic dermatitis, food allergy, folliculitis, Cheyletiella infestation and dermatophytosis. Cats with FAD can show pruritus, alopecia, facial dermatitis, and exfoliative dermatitis.
Diagnosis of FAD
In general, diagnosis of FAD is dependent on various variables including suggestive history, clinical signs, presence of fleas or their excrement on the pet, allergy testing (skin tests and serum tests), ruling out other causes of dermatologic disease (i.e. differential diagnoses) and response to appropriate anti-flea therapy.
History and clinical signs
Discussed above.
Visual observation of fleas or flea excrement on the infested pet
In some cases it is difficult to find evidence of fleas, such as in hypersensitive animals, which self-groom excessively. In these situations, the use of a fine-toothed flea comb facilitates finding of fleas and their excrement. Examination of the pet’s bedding for eggs, larvae, and excrement is also useful. Flea excrement can be detected by using a damp paper test in which flea excrement is placed on a damp paper towel and crushed, the excrement dissolves, producing a reddish brown colour. Alternatively, the dog’s coat can be brushed over the paper and small amounts of flea faeces (like small black dots) will fall onto the damp paper and show a reddish halo.
Allergy testing
Intradermal testing (IDT) using flea antigen extracts or pure flea saliva can be used to support a clinical diagnosis of FAD. Positive immediate reactions are characterized by a wheal ~3–5 mm larger in diameter compared with the negative control. Observations for an immediate reaction (15–20 minutes) and, if negative, a 24–48 hour delayed reaction are recommended. The delayed reaction may occur as a diffuse erythematous reaction. A positive reaction does not decisively indicate that the clinical condition is FAD—it indicates only that the animal is allergic to the flea antigen, either from current or prior exposure. Hence, results should be interpreted in the light of the case history and clinical signs. Type I and to some extent Type IV reactions are the reaction basics sought in IDT for flea allergy. Serological allergy testing using ELISA for IgE antibody to flea saliva antigen (FSA) has been reported (Stedman et al, 2001). However, the development of FAD is not necessarily associated with the presence of anti-flea saliva IgE antibody. Some dogs with positive IDT response have negative results on flea antigen-specific IgE antibody and vice versa.
Differential diagnosis
FAD in dogs must be differentiated from other causes of dermatologic disease including food and atopic allergy dermatitis. Other causes of dermatoses include: pediculosis; cheyletiellosis; scabies; trombiculosis; Malassezia dermatitis; dermatophytosis; demodicosis; and superficial pyoderma. In cats, other conditions that can result in miliary dermatitis including external parasites (cheyletiellosis, trombiculosis, notoedric mange, and pediculosis), dermatophytosis, drug hypersensitivity, food allergy, atopy, bacterial folliculitis, and idiopathic miliary dermatitis, must be ruled out. The situation may be complicated by dogs being both flea-allergic and atopic as flea allergic dogs are more likely to be atopic than non-flea allergic dogs (Laffort-Dassot et al, 2004).
Treatment and control
Control of fleas
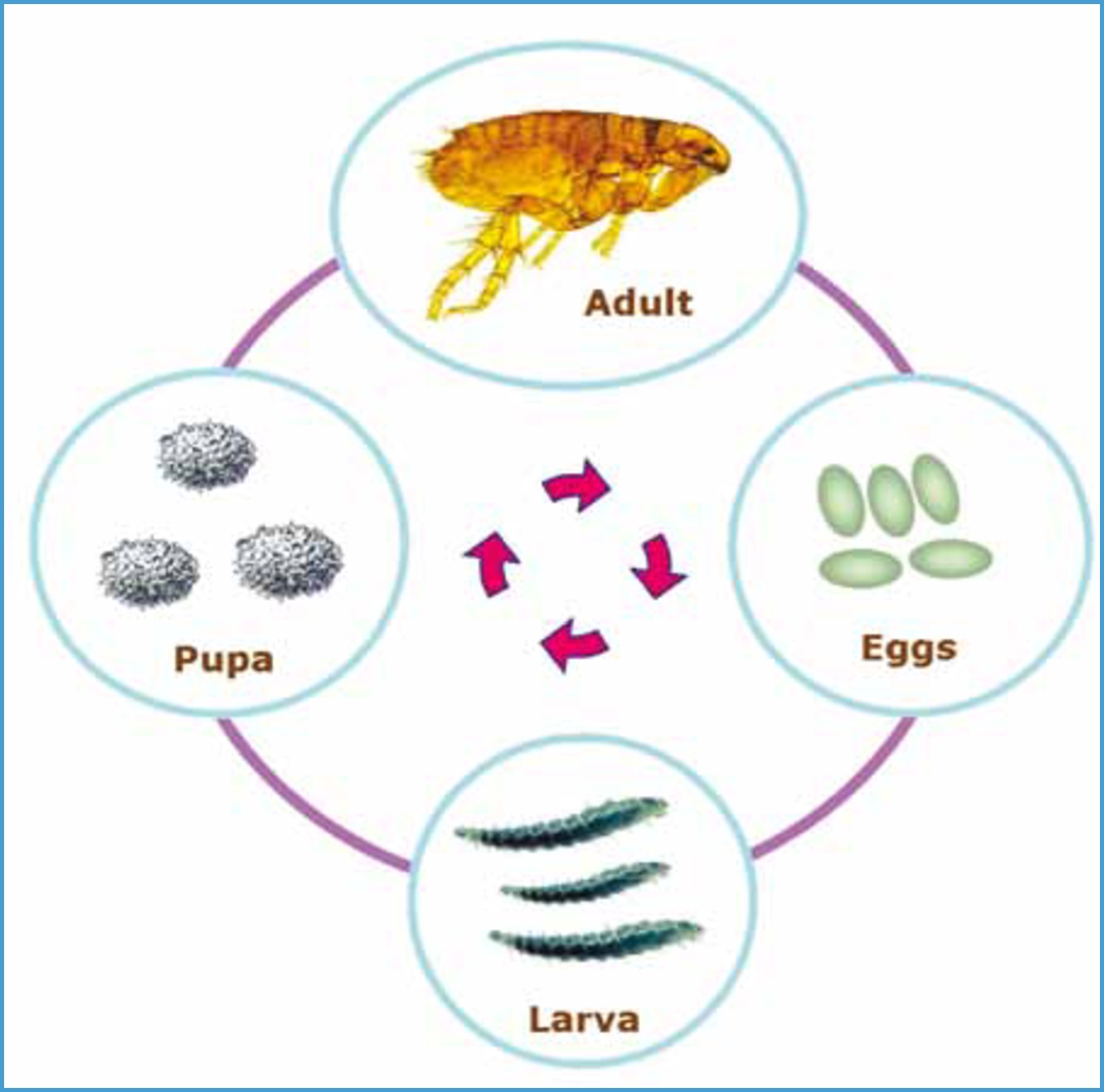
An important goal for treatment of FAD is to effectively control flea populations and prevent exposure to adult fleas. Success may be easy in situations for example where a cat is confined indoors and/or all cats and dogs in the house are treated with products that both kill fleas and prevent completion of the flea life cycle (Figure 3).
Integrated flea control
While fleas are found on animals, a large proportion of the developmental immature stages can be found in the environment. Hence flea control is a challenging task and a continuing flea infestation can be expected for weeks after treatment has begun. This is mainly because immature flea life stages continue to develop, and adult fleas are likely to emerge from the household environment. Since immature fleas tend to move away from light it is no easy job to remove them. However, regular hoovering and washing pet bed covers, focussing cleaning efforts particularly
where the pets lie, will help to reduce the environmental flea burden. In summer, when the environment is neither too wet nor overly exposed to sun, the flea life cycle may complete outdoors and this should be considered in any control regimen.
Further information about approaches to flea control can be found in, for example, Elsheikha (2012), ESCCAP (www.esccap.org) and ESCCAP UK (http://www.esccapuk.org.uk/), specially designed to be utilized by pet owners, and professionals.
Chemotherapy
The goals of a sound flea control strategy are to: eliminate fleas on pets; eliminate existing environmental infestation either by using sprays with insecticidal or insect growth regulating activity or by relying on newly emerged fleas being killed once they have located a suitable treated host; and prevent subsequent reinfestation. In cases where environmental infection is substantial then professional pest control may be necessary.
Numerous safe and effective host-targeted flea-control agents are available. These include topical (imidacloprid, fipronil, metaflumizone, indoxacarb, selamectin) and oral (nitenpyram, spinosad) adulticides. Some flea-control formulations also combine adulticides with insect growth regulators (e.g. methoprene, pyriproxyfen) or insect development inhibitors (e.g. lufenuron). These exert an affect on stages in the environment as treated dander, which will have insecticide on them, will fall into the animal’s environment and be consumed by the flea larvae, which will then die. Care should be taken to ensure that treatments for dogs are not used on cats, this is particularly important as cats are intolerant of many pyrethroid products available for dogs.
Some of the flea control agents will control fleas alone; others will treat a range of other parasites. It is therefore important to integrate flea control into overall parasite control for that animal. Principles to apply when choosing appropriate chemotherapeutic agents against fleas include: knowledge of the speed of action; duration and spectrum of activity; route of administration, and systemic versus topical action of the product; and knowledge of likelihood of owner compliance. Obtaining owner buy-in hence compliance is critical for a successful outcome.
Adjunct therapeutic options
Adjunct therapy should never be used as a substitute for flea control.
Corticosteroids
Systemic corticosteroids have proved beneficial as a supportive treatment to control inflammation and associated pruritus. Corticosteroids allow a marked, but temporary remission. As soon as flea control is accomplished, the glucocorticoid should be discontinued due to side effects associated with long-term therapy with the corticosteroids.
Antibiotics
Systemic antibiotics are commonly used to control the pyoderma associated with secondary bacterial infection in FAD. Selection of an appropriate antibiotic should be based on bacterial cultures and results of antibiotic sensitivity tests.
Immunotherapy
Hyposensitization — administering of allergens to a hypersensitive animal on a regular basis in an attempt to obtain a state of clinical non-reactivity (tolerance) to flea bites has been reported, but the effectiveness of whole flea extracts is controversial.
Jin et al (2010) reported that simultaneous co-immunization with FSA1 DNA vaccine and its cognate-recombined protein antigen improved clinical signs and alleviated the allergic responses in cat with established FAD. The improved therapeutic outcomes of treated cats demonstrate the potential of this strategy for a practical application. This study opened the door to studies aimed at defining protective immune responses which govern hypersensitivity and identification of putative targets for new therapies. Identifying the pertinent molecular target for immunotherapy poses a major challenge. However, recent technologic advances have the potential to identify novel flea saliva antigens with a dual role in infection protection and allergy. Such antigens could provide novel targets for therapy of infestation and associated allergy.
Prevention
Prevention of dogs and cats developing FAD depends on the owner being made aware of the potential for the development of FAD, hence the importance of ongoing vigilance for fleas together with appropriate preventative strategies.
Once an animal is hypersensitive then prevention is reliant on eliminating as far as is possible future exposure to flea bites, or at least keeping them below the exposure threshold for that animal. Owner vigilance, perhaps including regular checking of the animals in the household with a flea comb, will assist in catching any flea problem in the early stages.
Conclusion
FAD is a painful and recurrent condition that can be prevented by robust flea control and can be managed subsequent to its development by effective flea control, although the sensitivity of individual animals will vary. The mechanisms that lead to the development of FAD are complex and involve an interaction between allergenic compounds present in fleas’ saliva and dysregulated immune response in a predisposed animal.
Key Points
- Flea allergy dermatitis (FAD) is a serious skin disease, particularly affecting dogs and cats.
- FAD results from the bites of fleas, and is caused by an exaggerated host immune response to antigens present in flea’s saliva.
- Clinical signs vary depending on the degree of sensitivity.
- Pruritus is the main clinical manifestation of FAD.
- Eosinophilia and pruritus are the hallmarks of FAD; however, they occur under other infectious and non-infectious conditions.
- The presence of fleas, a positive intradermal test, or specific anti-flea IgE antibody does not rule out the presence of another skin disease linked to the clinical signs.
- Appropriate insecticide should be applied as directed at the correct time.
- Recurrence of flea infestation and FAD are common once therapy is discontinued.
- Considerable efforts should be devoted to develop rational integrated management tools.
- To answer the CPD questions on this article visit www.theveterinarynurse.com

