This article will first look at how veterinary nurses became advocates for their patients. Naturally, the published literature will be considered including human nursing where most of the evidence can be found.
Nursing leaders since the time of Florence Nightingale have envisioned advocacy for both patients and caregivers as an integral part of nursing's mission. The first ‘Nightingale nurses’ began training in 1860 and spread throughout the UK and the British Empire. While advocacy on behalf of patients and caregivers has remained a central concern — the American Nurses Association (ANA) publication Nursing: Scope and Standards of Practice identifies advocacy for safe, effective practice environments as a responsibility of the professional nurse (Walker et al, 2015) (ANA, 2015) Nursing occurs in any environment where there is a healthcare consumer in need of care, information, or advocacy (ANA, 2015). Nurses can fulfil the role of patient advocate by determining the best interests of their patients and using their own voices to promote those interests (Walker et al, 2015).
The use of behavioural and physiological indicators is recommended for pain assessment in non-verbal patients (Arbour and Gelinas, 2014). In humans, this group includes paediatric patients, traumatic brain injury patients, mental disabilities patients, geriatric patients and Alzheimer's patients.
Veterinary nurses as advocates
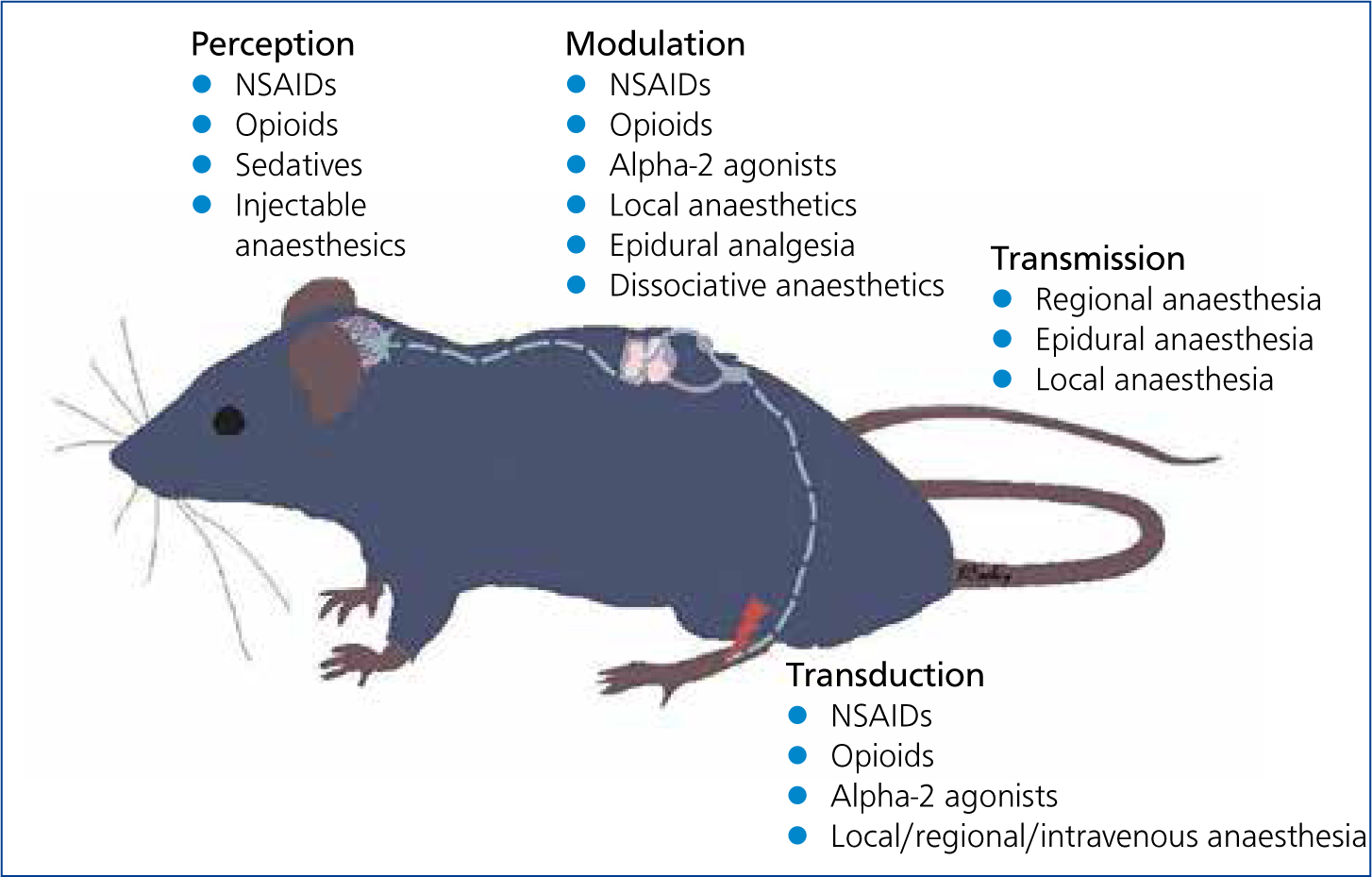
The quality of pain management in practices seems to be directly related to veterinary nurses (Shaffran, 2008). The veterinary nurse interacts with the patient more than the veterinarian. They are responsible for the primary nursing care of their patients. Therefore, their observations should be directly communicated to the veterinarian so that proper, updated analgesia can be provided. The role of advocate for a non-verbal patient can be daunting. Veterinary nurses are in the unique position of being responsible for most of and the quality of patient care without the freedom to prescribe or initiate therapy (Shaffran, 2008). Knowledge of the physiology of pain (Figure 1) and pharmacology of analgesics is essential for good communication between veterinarians and veterinary nurses. The skilled nurse is a source of vital information required to choose and administer appropriate analgesics.
Communication
Nurses use critical thinking, observation, and interpretation skills to make important pain management recommendations. Since pain is considered the 4th vital sign, pain should be assessed along with temperature, pulse and respiration (Hansen, 2006). Discussion about each case directly with the clinician might include the nurse's concerns about a patient or a general approach to managing different types of pain. Based on his or her interaction with patients, the nurse may offer suggestions for adjustments in analgesic regimens or changes/additions to drug protocols, or the possible addition of sedatives, if needed (Shaffran and Grubb, 2015). Nurses must learn to include important criteria when reporting to the veterinarian. The veterinary nurse must present information in a factual manner to support their statement. They cannot just say something similar to, ‘I think Fluffy hurts, but cannot prove it’. Veterinary nurses need to indicate that they can accurately tell how painful the patient is while explaining why or why not additional analgesics could be beneficial. Veterinary nurses have the responsibility of continually monitoring their patients and often develop a sense of which analgesics seem to work best under various circumstances. Nurses should provide as much feedback as possible for which analgesic protocols are working well, and which need to be improved to increase patient comfort. Pain management issues, such as the appearance and behaviour of the patient that prompted the administration of analgesics; the type, dose, and timing of previous analgesic administration; and the response and any adverse reactions after administration, should be described (Shaffran, 2008).
Allowing the nurse additional freedoms
For the veterinary nurse to have greater freedom, the veterinarian must be able to trust the nurse's judgement and experience (Shaffran, 2008). If legally allowable, once standing orders (such as dose ranges) are established, the success of pain management can rely on skilled nurses having the freedom to give analgesics as needed, to adjust dosages when required, to administer adjunctive medications, and to potentially reverse drugs when severe adverse reactions occur. If trust has been established, then the responsibility and freedom to administer agreed-on analgesics is rewarding for all concerned. Giving nurses a voice in the pain management process creates a truly positive team environment in which nurses' thoughts and skills are valued. Patients ultimately receive better care, and nurses are satisfied knowing that they are doing everything they can to ensure the wellbeing of patients in their charge (Shaffran, 2008).
How stress and pain intersect
Pain and distress can be thought of in terms of a continuum of emotional and experiential states that may occur in an animal (Goldberg, 2017). Comfort represents a state of wellbeing, where the animal is contented and comfortable. Stressors acting on the animal in increasing severity cause the animal to progressively become uncomfortable (discomfort), then stressed (stress), and finally distressed (distress). Distress represents the extreme point in this continuum, on the far right. Stressors acting on the animal may move the animal's experience along this continuum between the extremes of wellbeing and distress. Depending on the nature and severity of a stressor and on the animal's current state of being, the animal may adapt successfully to a stress (adaptive behaviours) or it may become distressed in a way that threatens its wellbeing or health (maladaptive behaviours). Maladaptive behaviours include abnormal feeding, absence or decreased grooming, and changes in social interaction (aggression, withdrawal). A departure from an animal's normal behaviour is an important indicator that it is undergoing pain and distress. The veterinary nurse will not be prescribing medications, but instead making suggestions to the veterinarian about behaviours they have seen.
Signs of pain and distress
There are numerous stereotypical responses to stress or pain stimuli in animals, particularly in mammals (Clark et al, 1997). Nevertheless, species differences do exist. Recognition of changes in behaviour and physical appearance in the species under study will allow early identification of an animal experiencing pain or distress. As caregivers, humans may know that an event or situation is no threat, but the animal usually does not function with the same information base as humans.
The following are personal observations by the author.
Non-human primates (NHP)
Monkeys often show remarkably little reaction to surgical procedures or to traumatic injury (Wolfensohn and Honess, 2005). Obvious signs of pain are not readily seen. Loud and persistent vocalisation, for example, commonly signifies only alarm or anger. The animal in pain may be huddled in a crouching posture with a ‘sad’ facial expression and glassy eyes, or it may sit hunched with its head forward and its arms across its body. It may avoid its companions and may stop grooming itself. A monkey in pain may also attract increased attention from its cage mates, which can vary from social grooming to attack. Acute abdominal pain may be shown by facial contortions, clenching of the teeth, restlessness, and shaking accompanied by grunts and moans. Food and water intake is usually diminished or absent.
Key signs: hunched position, failure to groom, refusal of food or water, dejected appearance (Wolfenson and Honess, 2005; Murphy et al, 2012).
Mice
After procedures that cause pain, mice may increase their sleeping times. Reduced food and water intake, with resultant weight loss, dehydration and wasting of the muscles on the back may be observed. Piloerection (erection of hair) and a hunched appearance indicate pain or distress. The animal fails to groom, but scratches more frequently. Sick mice are often isolated from the remainder of the group. Aggressive vocalisation is observed in the early stages, decreasing where pain or stress reduces the ability to move and respond. The eyes appear sunken, and ocular and nasal discharge may be noted as the animal's condition worsens. The Mouse Grimace Scale developed in 2010, gives an excellent description of facial expressions from painful mice (Langford, 2010) (Figure 2). The respiration rate increases and breathing may be forced or laboured. As its condition worsens, the animal becomes quiet and unresponsive, separates from the group and eventually becomes unaware of its surroundings. Hypothermia is observed with increasing deterioration in condition; the animal feels ‘cold’ to the touch.
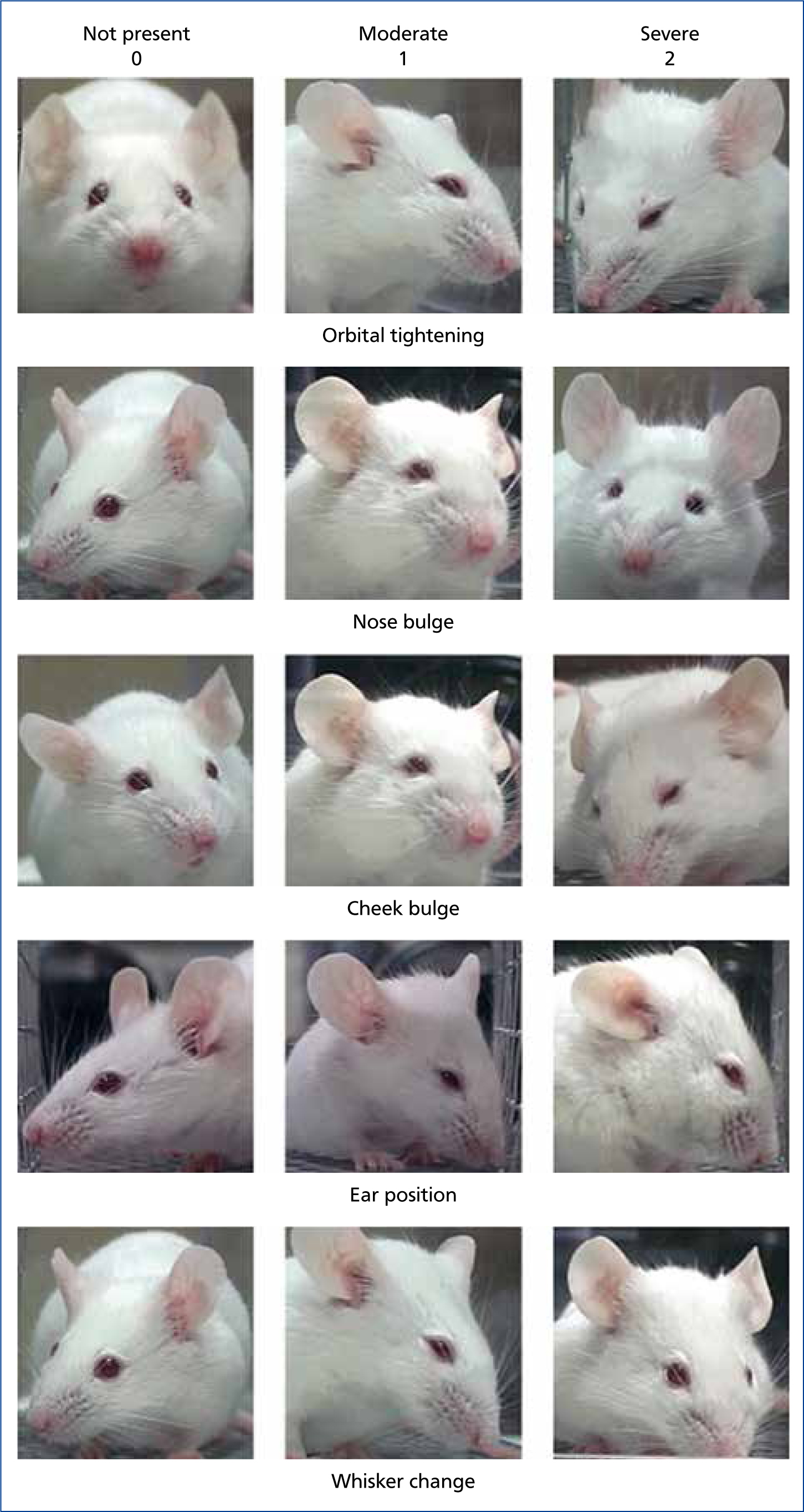
Key signs: withdrawal, biting response, piloerection, hunched back, sunken eyes and abdomen, dehydration, weight loss (Langford, 2010; Malik and Leach, 2017).
Rats
Rats are generally docile and less aggressive than mice towards members of their own species and humans. Acute pain or distress is usually accompanied by constant vocalisation and struggling. Rats will often lick or guard a painful area. Increased scratching can indicate chronic pain. A rat in pain will often sit crouched with its head turned into its abdomen. Sleeping periods will be disturbed and increase if pain or distress is present. The Rat Grimace Scale shows pictures of facial expressions from rats in pain (Sotocinal et al, 2011) (Figure 3). An elevated respiratory rate associated with sneezing occurs where the respiratory system is affected. Increasing piloerection (staring coat) is noted, along with an increasingly untidy appearance as the animal fails to groom itself. The eyes may appear sunken, and ocular discharge is common, often progressing to red-coloured haematoporphyrin exudate which may encircle the eye. Nasal discharge, if present, may be red-coloured as well.
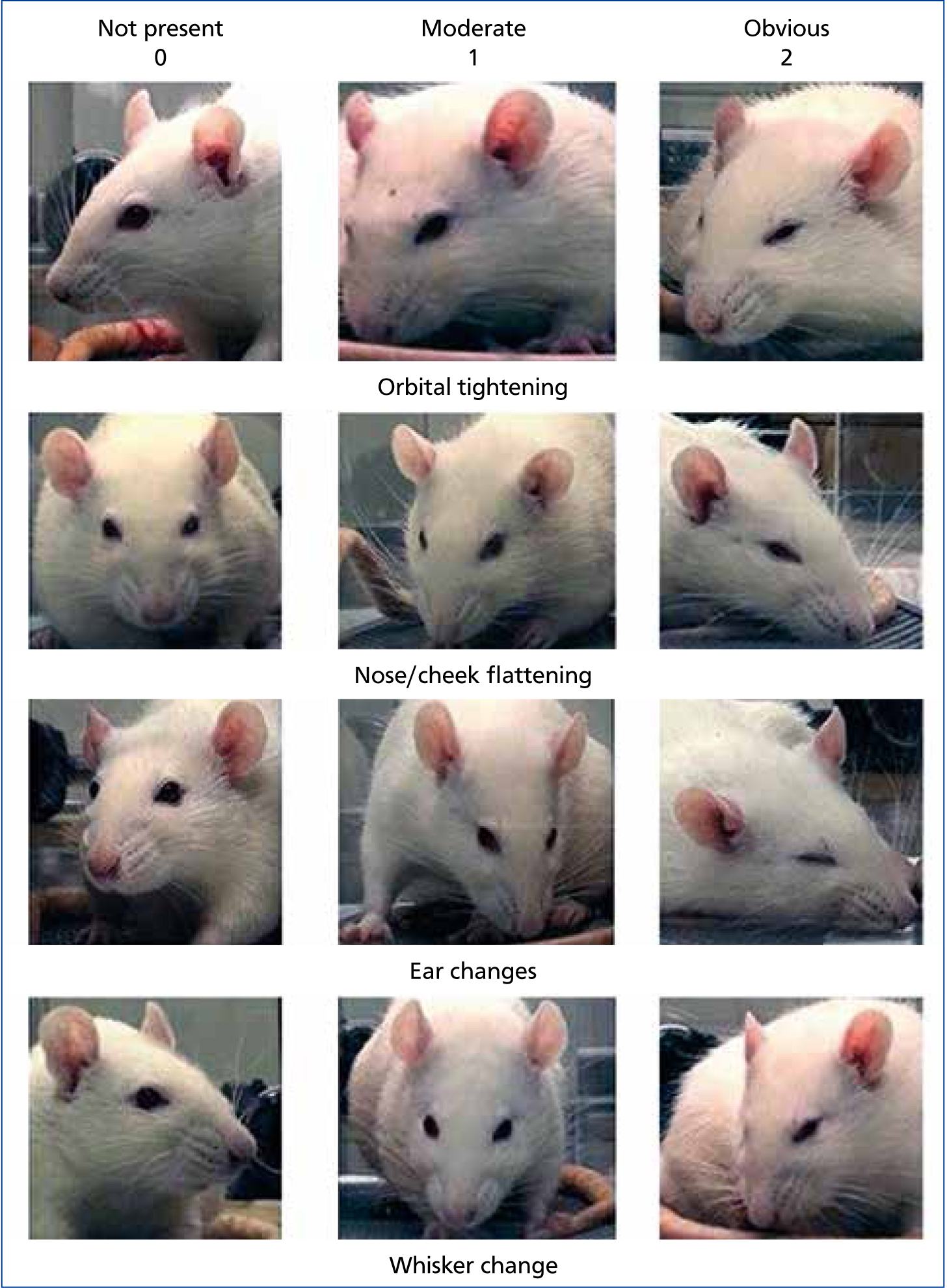
Initially, the rat exhibits increased angry or aggressive vocalisation, especially on handling. There is a gradual reduction in vocal response as the pain or stress continues, and movement ceases unless a sudden painful stimulus is experienced. Hypothermia indicates significant deterioration in the animal's condition. A pale appearance indicates anaemia or blood loss.
Key signs: vocalisation, struggling, licking/guarding, weight loss, piloerection, hunched position, hypothermia (Carstens and Moberg, 2000; Malick and Leach, 2017).
Guinea pigs
Guinea pigs are alert, but timid and apprehensive animals which will try to avoid capture and restraint. Rarely is there any aggression towards humans. Any sign of acceptance indicates the animal is unwell. Loud vocalisation will accompany even minor and transient pain. Guinea pigs often appear sleepy when in pain. The eyes may be sunken and dull. There may be pain associated with locomotion, lameness, and careful gait due to sore feet in older animals.
Key signs: withdrawal, vocalisation, failure to resist restraint, staring coat, unresponsive (Carstens and Moberg, 2000; Gaertner et al, 2008).
Mongolian gerbils
Gerbils are highly active, nervous animals and usually attempt to avoid restraint. Signs of pain and distress are difficult to assess, as gerbils apparently object to any interference. There is an increased level of response under painful or stressful stimuli. Ocular discharge is common. Under stressful conditions, the eyelids may be half closed, with dry matting of the eyelids. Dehydration is rarely seen, since the gerbil's normal metabolism enables full utilisation of the water content of the diet. Only small quantities of urine are voided under normal conditions. Faeces are normally firm, dry pellets. A hunching up and arching of the back may be observed when pain is present especially with abdominal involvement. Abnormal gait is associated with locomotion or abdominal involvement.
Key signs: hunched appearance, weight loss, shock syndrome (Carstens and Moberg, 2000; Gaertner et al, 2008).
Syrian (golden) hamsters
Under normal conditions, hamsters will sleep for long periods during the day, and little activity will be seen. They often appear aggressive towards their cage mates and emit loud screeching noises, disproportionate to the degree of interference, when handled. This response increases under painful or stressful stimuli. Ocular discharge is commonly associated with stress. Daytime sleep periods may be extended and increasing lassitude may be seen except when the animal is being handled. Exploratory behaviour is reduced. A hunched appearance is noted, as is an unwillingness to move, especially where abdominal organs are involved. Lateral recumbency can indicate that the animal is moribund. Normal gait is affected when pain is associated with locomotion. Stilted movements are sometimes associated with abdominal involvement, e.g. ascites following cirrhosis of the liver.
Key signs: weight loss, hunched appearance, increased aggression or depression, extended sleep periods (Carstens and Moberg, 2000; Gaertner et al, 2008).
Rabbits
The rabbit presents significant difficulties in recognition of pain and distress, as it often quietly accepts apparently painful or distressing procedures; this may relate to its feral behaviour where concealment is important to survival. Even healthy rabbits may not move frequently or indulge in exploratory behaviour. Pain is usually characterised by a reduction in food and water intake (and thus weight loss and dehydration) and limited movement. Ocular discharge is a common response to stress in the rabbit, with protrusion of the nictitating membrane. The Rabbit Grimace Scale, developed in 2012, clearly shows images of this appearance in rabbits (Figure 4).
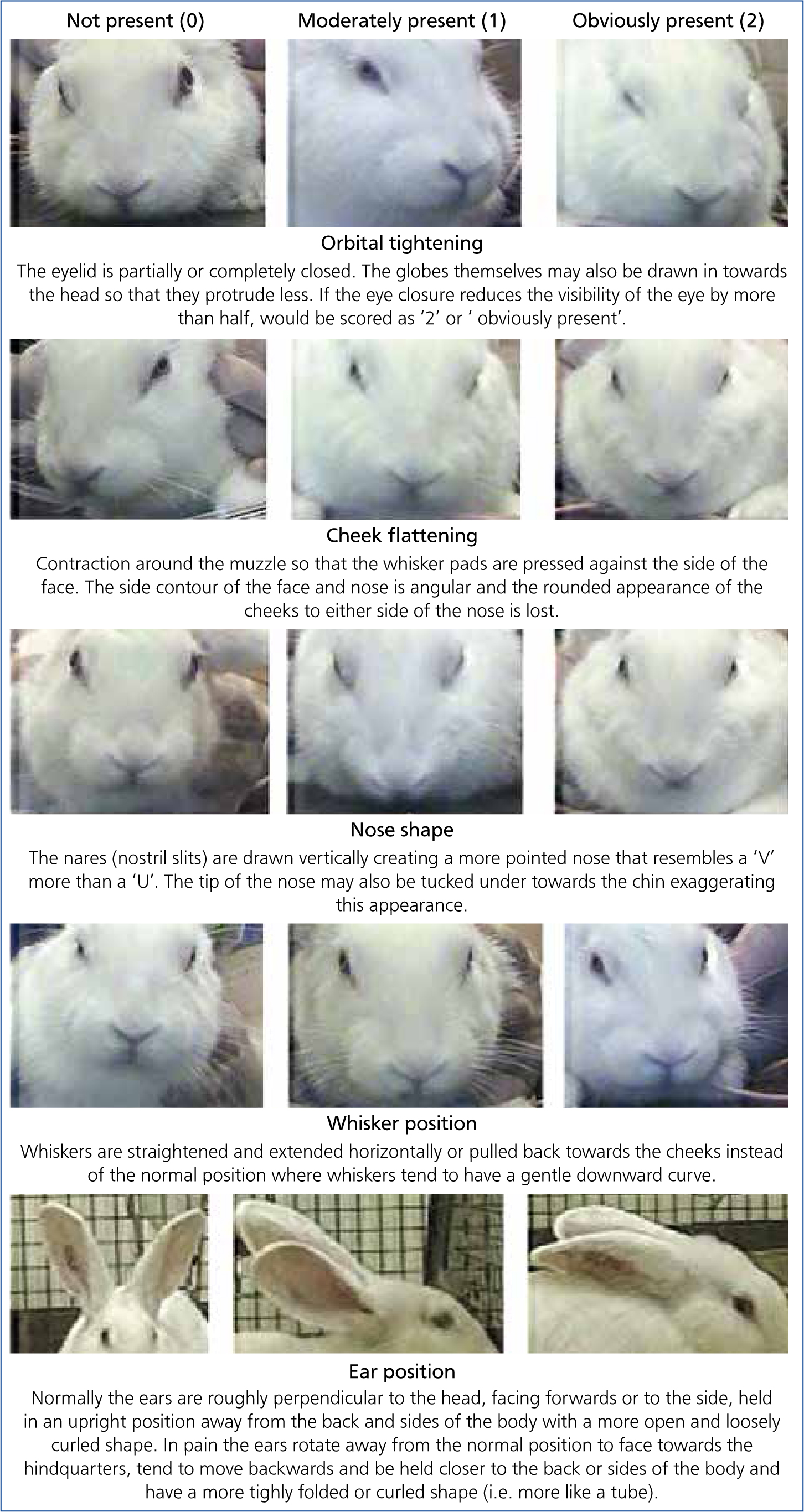
Under continued pain or stress, rabbits assume a ‘sleepy’ appearance. The animal exhibits increased depression, progressive unawareness and lack of response. The animal will often face the back of cage, away from light. Where foot soreness is involved, weight may be thrown forward or backward to reduce discomfort. Body stretching and lying flat are common indications of abdominal discomfort. Pain may be associated with locomotion, especially with sore feet.
Key signs: reduced eating and drinking, faces towards back of cage, limited movement, and apparent photosensitivity (Johnston, 2005; Carbone and Austin, 2016).
Ferrets
Pain tolerance likely varies greatly between individual ferrets just like in other species. There is evidence that solitary-living animals and prey animals are masters of disguising pain (van Oostrom et al, 2011). Ferrets in pain may stay curled in a tight ball or have a hunched back. They may have an altered gait. They may have decreased or increased food and water intake. They may exhibit bruxism. They may hide in the back of a cage, vocalise, be aggressive, not groom and look unkempt. The most likely causes of pain in ferrets are arthritis, cancer, or dental problems (Lafferty et al, 2015).
Key signs: stiff posture, demented behaviour, lack of grooming, hunched head and neck, and inappetence (Johnston, 2005; Ko and Marini, 2014; Johnson-Delaney, 2017).
Birds
Many clinical signs may be associated with pain in birds including change in temperament to either aggressive or passive, restlessness, reluctance to stand, perch or even move, anorexia, lethargy, a hunched appearance, tachypnea, and lameness. Birds may avoid a painful area and reduce preening, or they may over-groom, feather pick, or chew at the area. Behaviours such as vocalising and writhing may only manifest during acute or severe pain or may not manifest at all in birds.
Few consistent physiological indicators of pain have been identified in birds. In feather-plucked chickens, heart rate and respiratory rate varied between animals but hypertension was a reliable indicator (Gentle and Tilston, 1999). Faecal corticosterone concentrations have shown potential as a non-invasive method of determining stress and pain (Machin, 2001).
Key signs: escape reactions, atonic immobility, inappetence, and avoidance of use of pain site (Murphy and Ludders, 2001; Lichtenberger and Ko, 2007; Petritz, 2017).
Reptiles
Acute pain in reptiles may be characterised by flinching and muscle contractions. There may be aversive movements away from the unpleasant stimulus, and attempts to bite (Figures 5 and 6). More chronic and persistent pain may be associated with anorexia, lethargy and weight loss, although it is difficult to associate any of these signs of lack of wellbeing specifically with pain (Mosley, 2011).


Key signs: flinching and muscle contractions, weight loss, anorexia.
Fish and amphibians
It is difficult to determine the nature of the response to pain in fish and amphibians. Although they exhibit a pronounced response to injuries or to contact with irritants, their response to chronic stimuli may be small or absent. Although the response may be subtle and small this does not negate the need for analgesics in fish (Stevens, 2011). Fish and amphibians with severe wounds which would cause immobility in a mammal, will often appear to behave completely normally, even resuming feeding (Figure 7). Fish and amphibians will react to noxious stimuli, such as that administered by a hypodermic needle, by strong muscular movements. Fish, when exposed to a noxious environment, such as a strong acid, show abnormal swimming behaviour with attempts to jump from the water, their colouring becomes darker and their opercular movements become more rapid (Weber, 2011). Such effects are indicative of some degree of distress; however, it is not possible to describe these unequivocally as signs of pain. However, it must be assumed that whatever causes pain in mammals, birds and reptiles will also cause pain in fish and amphibians.

Key signs: amphibians — muscular movements, closed eyes, colour changes, rapid respirations, immobility, and anorexia (Machin, 1999; Stevens, 2011). Fish — abnormal swimming behaviour, attempting to jump out of water, rapid opercular movements, clamped fins, pale or darkened colour, and hiding. Anorexia is the first sign (Neiffer and Stamper, 2009; Posner, 2009; Sneddon, 2012).
Invertebrates
Although invertebrates do not possess a central nervous system with a well-described cortex or similar structure, it has been shown that a nociceptive response is present in invertebrates (Mosley and Lewbart, 2014). Nociceptive cells have been found in invertebrates and opioid systems are functional in invertebrate nociception (Lafferty et al, 2015). Opioids and local anaesthetics provide good analgesia.
Key signs: invertebrates — rapid withdrawal (Mosley and Lewbart, 2014; della Rocca et al, 2015).
Zoo and wild animals
Analgesia is becoming increasingly important in veterinary medicine, and controlling pain in zoo animals is an important component to improving the welfare of captive animals (Wesselman et al, 2015). Behaviours associated with pain are variable between species, and some animals may not show signs until severely distressed. Careful observation of behaviour by animal care staff can aid in the recognition and therefore treatment of painful conditions in zoo animals (Souza and Cox, 2011). Species involved can typically include, elephants, rhinoceros, hood stock (such as gazelles, zebra, kudus, water buffalos), non-human primates (such as chimpanzees, gorillas and orangutans), hippopotamus, giraffes, and large felines (such as lions, tigers, cougars, cheetahs). Zoo and wild animals look different, have different social systems, and react to pain and pain medications differently to their domestic species counterparts. Prey and predator species mask issues from their conspecifics (belonging to the same species) and caretakers. Predators also mask their pain in front of conspecifics due to the competition for territories and prey. Despite the differences in patients, the role of a veterinary technician as a patient advocate in zoo and wildlife medicine is like that of a domestic animal technician/nurse. The nurse is there to help ensure that every animal is well cared for and has an excellent quality of life. Husbandry staff are trained to read subtle changes in the behaviour, gait, or appearance of an animal (Figure 8). They will alert the veterinarian as soon as an animal begins to act uncharacteristically, utilising their knowledge to understand the basics of that animal or species. The entire team needs to be part of any treatment plan, as the responsibility of the animal's daily care does not rest on one person.

Overall appearance of an animal can also be a good indicator that something is awry with an individual animal. An animal that appears unkempt is most likely unthrifty due to illness, but this effect is also seen in animals with chronic pain. Animals will keep their heads lower; their ears may droop or fall back towards their heads (Figure 9). Stance can change by arching the back or tucking in the limbs or abdomen (Bradley, 2001). Some animals that are sick or injured will allow a threat, that is, veterinary staff, to get closer than if they were healthy. An observer could then use changes in flight distance as an indicator of the severity of the injury or illness. While veterinary nurses do not prescribe medications, they typically dispense and administer them. Currently used treatments and doses have been extrapolated from similar species, which works in some cases, but not in the others (Machin, 2007). Forums and networking between institutions and zoo or wildlife professionals are valuable tools when trying to determine the appropriate analgesic protocol to use. Veterinary nurses have a discussion forum at the Association of Zoo Veterinary Technicians (AZVT) website http://www.azvt.org/.

Key signs: behavioural changes, appetite changes, animal isolation from their group or pack, aggression, lameness, unkempt appearance, or lowered head (Whiteside, 2014; Boothe et al, 2016).
Conclusion
Identification of pain and distress in exotics and zoo/wildlife animals requires a knowledge of normal behaviours. Many of the species hide any sign that something may be abnormal because of a survival instinct. Once normal is recognised, then anything apart from those behaviours could be indicative of pain. Veterinary nurses are taught that from an animal welfare perspective the patient should not be required to prove it is in pain (Clark et al, 1997). The question asked shouold no longer be ‘does the animal experience pain’, but rather ‘what kind of pain can the animal experience’ (Whiteside, 2014). The animal patient is always given the benefit of the doubt and should have analgesics prescribed or non-pharmacological therapy provided to alleviate a problem. The veterinary nurse is the patient's primary advocate since they are non-verbal and cannot state where they feel pain. Veterinary nurses should strive to learn the signs of pain in non-traditional species.

