Pain can be detrimental to a patient's recovery because of the negative emotional experience, protracted recovery and an increased risk of malnutrition, which collectively lead to an impaired immune system (Murphy, 2016). Pain is linked to the stimulation and release of catecholamines and adrenal hormones such as cortisol (Self and Grubb, 2019). This will contribute to weight loss, wound dehiscence, leucocytosis and insulin resistance, leading to the development of chronic pathological pain, client dissatisfaction and a loss of time and money (Self and Grubb, 2019). Milella and Gurney (2017) identified surgeries that are moderate to severe in their pain scale and should have the combination of an opioid, non-steroidal anti-inflammatory drug (NSAID) and local anaesthetic to provide a multimodal analgesia approach; local anaesthetic agents prevent the pain stimulus reaching the central nervous system. Klinck and Troncy (2017) described pain as a mixture between the origin and stimulus creating a combination of various pain types, such as nociceptive, neuropathic and inflammatory. Klinck and Troncy (2017) explained the contribution of neuropathic pain which depends on the two factors, the type of surgery and the degree of surgical nerve injury.
Pain pathway
Woolf (2011) defined the three types of pain as: neurological, this stems from the nervous system because of abnormal function; nociceptive, this is a result of a noxious stimulus damaging the tissue; and inflammatory, once there has been tissue damage there is an infiltration of inflammatory cells from the immune cells. During surgery the tissue will be damaged, triggering the nociceptor cells within the skin and muscles to open their ion gates. This allows sodium and calcium to move across the gradient of the cell, causing nerve endings to depolarise; in addition potassium is blocked to allow an action potential to form (Klinck and Troncy, 2017). The chemicals will activate the receptors at the nerve endings to send this information along the spinal cord to the brain before the sensation of pain can be detected by the patient (Klinck and Troncy, 2017). Inflammatory pain is triggered once the tissue is damaged and nociceptors activated — the tissue becomes inflamed and remains this way until the tissue has healed (Klinck and Troncy, 2017).
Duke-Novakovski (2017) defined local anaesthetics as either amino-esters or amino-amides. They act by inhibiting and preventing a surge in sodium ions within the nerve axons; this will prevent any nerve action potential and propagation of nerve impulses being transmitted to the central nervous system (Duke-Novakovski, 2017). According to Milella and Gurney (2017), the local anaesthetic should be administered after the induction of the anaesthetic, but prior to the surgery, reducing the amount of inhalant anaesthetic and analgesia required intraoperatively and postoperatively. Reducing the inhalant will reduce the risk of potential side effects of the general anaesthetic. There are a number of negative effects inhalants have on the body (Pang, 2017):
- Decreased cerebral metabolic rate
- Increase intracranial blood volume
- Cardiovascular depression
- Hypotension
- Vasodilation
- Hypercapnia
- Hypoventilation
- Bronchodilator
- Reduced renal and hepatic perfusion as a result of hypotension
- Reduced urine output postoperatively
- Hepatic dysfunction.
Finally, Pang (2017) stated inhalant agents do not have analgesic properties. They can only block pain perception as a result of loss of consciousness. Once the patient has recovered from the surgical procedure the patient will be able to perceive pain.
A multidimensional scale can be used to measure the patient's pain intensity, sensory and components of pain that affect the patient's behaviour (Self and Grubb, 2019). Using a pain scoring system postoperatively allows the registered veterinary nurse (RVN) to demonstrate how effective the multimodal analgesia has been, and create a standard of assessment and justification towards the treatment of pain.
Use and benefit of pain scores
RVNs can improve pain management within the veterinary practice by addressing the underuse of analgesia within the veterinary practice (Malik and Bradbury, 2016). Malik and Bradbury encouraged the use of a pain assessment protocol to provide written evidence and justification for analgesia. They explained that it is essential that RVNs and veterinary surgeons (VS) have an understanding of the negative and detrimental effects pain can have on patients, as discussed earlier, this is in accordance with the Royal College of Veterinary Surgeons (RCVS) Code of Professional Conduct (RCVS, 2020).
Pain should be considered the fourth vital sign (Richmond, 2016) and there is a need to have a standard of care towards analgesia. Richmond (2016) explained that the attitudes of various veterinary professionals within a team can have a knock on effect on the analgesia a patient will receive; this is usually a result of the lack of formal guidance and understanding of analgesia. Richmond (2016) explained there are three steps to successful pain management, including:
- Pre-emptive analgesia — it has been shown in both human and veterinary medicine that prevention is the ideal approach to any procedure or treatment
- Multimodal analgesia — this will involve blocking each pathway of pain using three different classes of analgesic medications, including opiates, local anaesthetics and NSAIDs
- The continuation of analgesia after the procedure has finished.
The continuation of analgesia after the procedure should be made a priority to prevent any break in analgesia that could allow the patient to perceive pain. Ultimately consistency and communication within the veterinary team will ensure there is no lapse in pain management.
Client communication with the RVN or VS is essential to understand if the patient's pain is being managed correctly. A study that evaluated the perceptions and opinions of Canadian pet owners regarding anaesthesia, pain and surgery in small animals (Steagall et al, 2017) revealed that owners believe that surgical pain should be treated and that analgesia is an important part of veterinary care; however, some pet owners still believed that pain is a requirement postoperatively to limit their pet's activities. The study highlighted the role RVNs and VS play in educating clients regarding pain, and when to seek attention and analgesia treatment. An essential element of pain management is recognition and quantification of pain utilising a pain score tool (Murrell and Alderson, 2019). Using a pain score system such as the Glasgow Composite Measure Pain Scale Short Form (CMPS-SF), the RVN can communicate effectively the signs of pain to the owners to allow them to monitor for signs of pain while within the home environment. Based on the recommendations of both Malik and Bradbury (2016) and Richmond (2016), using CMPS-SF will provide a set protocol for the postoperative phase, and written evidence to show justification for further analgesia. This information can then be communicated back to the owners and they can understand how their pet may exhibit pain.
Local anaesthetics administration techniques
For a multimodal analgesia approach to work it is vital that all medications used complement each other as they each implement their role in inhibiting the pain pathway. Local anaesthetic can play an important role in the intraoperative and postoperative phase (Murrell and Alderson, 2019). Local anaesthetic can be administered by a variety of routes, such as perineural, epidural, in-traperitoneal, topical and transdermal (Corletto and Jolliffe, 2019) (Figure 1).

Benito et al (2015) performed a study examining the analgesic effects of intraperitoneal administration of bupivacaine in cats undergoing ovariohysterectomy. The study separated participants into three groups, each consisting of 15 cats; only one group was given intraperitoneal bupivacaine (BG) the other two groups were given 0.9% saline, with either the addition of an opioid and a NSAID (PG) or just an opioid (NG). The study showed that 80% of the NG, 27% of the BG and 13% of the PG required rescue analgesia. This study, the first of its kind to be performed, provided insight into the benefits of multimodal analgesia used during ovariohysterectomy in cats. It was able to provide reliable results by using the same surgeon to perform all the ovariohysterectomies and the same assessors for pain assessment postoperatively. The assessors were blinded to the study; this provided an effective measuring tool to produce consistent results (Crombie, 1996). Pain and sedation were assessed using DIVAS, mechanical nociceptive threshold and a UNESP-Botucatu multidimensional composite pain scale. Patients were assessed 60 minutes preoperatively and up to 8 hours postoperatively. The study was unable to give any clinical recommendations for intraperitoneal administration of bupivacaine in cats because of limited knowledge on plasma concentrations and pharmacokinetics. Before the initial study started, an unpublished safety study was performed in eight cats where intraperitoneal bupivacaine was administered to monitor the peak plasma concentrations to assess if any hypotension or arrhythmias were noted. The authors were also unaware if a higher concentration would increase the magnitude and duration of analgesia; the authors chose to dilute the medication to help achieve a larger volume of the anaesthetic spread. The doses of bupivacaine used were based on the author's experience so it was not known how long the duration of action would be. The effects of a higher dose of bupivacaine on the overall outcome of the study are unknown. The study highlighted how effective and simple it is to use a local anaesthetic to reduce pain in cats after ovariohysterectomy. However, it was advised to use both an opioid and NSAID to provide a multi-modal anaesthetic.
Kalchofner Guerrero et al (2016) carried out a study on the postoperative analgesia benefits of intraperitoneal bupivacaine with or without the addition of incisional bupivacaine on dogs undergoing ovariohysterectomy. This study involved 39 dogs of similar weights and ages. All of the dogs received the same pre-medications, NSAID and opioid; this would help to ensure reliable results supporting the author's hypothesis (Crombie, 1996). The dogs were split into two groups; 20 in group B that received additional bupivacaine in their incision, and 19 in group S that received saline. Both groups received their additional solutions as a topical application before the skin was closed. The results from this study showed there was no significant difference between the group that received the additional bupivacaine compared with the group that received saline. The study recognised its limitations, in particular the sample size and lack of a control group (Dytham, 2011), which made it difficult to determine the optimal choice of treatment for analgesia. There was also a variation in group B in the incisional dose of bupivacaine that each dog received. It was suggested the infiltration of bupivacaine using a fine needle could have produced different results. The study concluded that the addition incisional bupivacaine had no effect on the postoperative pain scores; however, the study did show the benefits of using bupivacaine and validation for it to be routinely used during ovariohysterectomy.
Fudge et al (2019) performed a study looking at administration of bupivacaine over the ovarian suspensory ligament and vessels in ovariohysterectomy in cats. This study showed the benefit of targeted bupivacaine in reducing postoperative pain and reducing pain scores. This study; along with the earlier studies, provided justification for the use of local anaesthetics during routine procedures such as ovariohysterectomy, which is simple and economical to use. Steagall et al (2020) highlighted the various studies that had previously been performed providing validation for intraperitoneal or incisional analgesia in small animals. Steagall et al (2020) suggested that either administration technique can be used. However, intraperitoneal seemed to be the preferred method because of its prolonged effect and safer option based on previous studies. Steagall et al (2020) suggested that if incisional administration is preferred, then it should be done during the preoperative phase instead of postoperatively. The paper gave further guidance for the dosage of bupivacaine, in particular for cats, which could be discussed with the VS to create an appropriate and in-dividualised treatment plan, but should not exceed 0.5%. A dose of 4 mg/kg in dogs and 2 mg/kg in cats should not be exceeded. Ultimately local anaesthetics can work to their full benefit for the patient when incorporated with other medications, such as NSAIDs and an opioid, to create a multimodal analgesic approach to achieve exceptional care and management of pain.
Comparison of long-term and short-term acting local anaesthetics
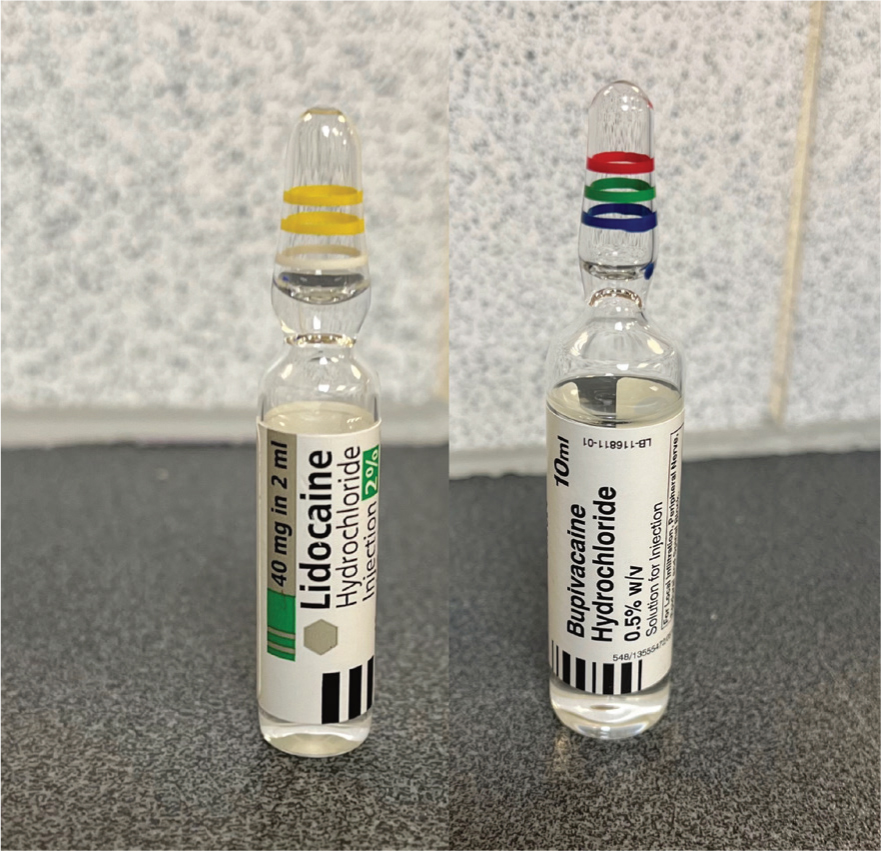
Both lidocaine and bupivacaine are commonplace within the veterinary practice, each having their own benefits and usages (Goldberg, 2017). Lidocaine has a quick onset of action of 15–20 minutes, however, it is relatively short acting being effective for 1–2 hours (Goldberg, 2017). Bupivacaine has a slower onset of action to reach full effect of 20–30 minutes, however, it is effective for 4–6 hours (Figure 2) (Goldberg, 2017). Bupivacaine liposome is a formulation of bupivacaine to encapsulate the bupivacaine within the liposome, postponing the peak plasma concentrations of bupivacaine. This allows a slower onset and prolonged action of analgesia of 72 hours, reducing the requirement for rescue analgesia from an opioid (Chahar and Cummings, 2012).
Vicente and Bergström (2018) discussed the intraoperative benefits of the combined effect of lidocaine and bupivacaine. The study consisted of 75 cats assorted into three different groups of 25: the control group (CG) received 0.9% sodium chloride; the lidocaine group (GL) received 1.5 mg/kg lidocaine; and the lidocaine bupivacaine group (GLB) received 1 mg/kg lidocaine and 1 mg/kg bupivacaine. Each group received their dose 15 minutes before the incision was made. Overall, the results showed all groups required an additional dose of propofol during the anaesthesia because of the increase in muscle tone and pupillary reflex. However, there was a higher percentage in the CG that required propofol (60%) compared with 43% in the GL and 44% in the GLB. The heart rate and mean arterial pressure (MAP) were notably higher in the CG during the excision of the ovary and uterine body compared with the GL and GLB, which maintained a stable heart rate and MAP. This study highlighted the benefits of local anaesthetic used during the intraoperative phase. Nevertheless, the study concluded the use of GLB to be the favoured group as this reduced the required dose of each medication with the conclusion of early onset of action and a prolonged effect. It was not mentioned whether any of the patients had a pain score performed postoperatively. It would have been beneficial to perform pain scores postoperatively to demonstrate if there was a prolonged effect with the GL and GLB groups. This could be the potential for further research into the postoperative benefits of lidocaine mixed with bupivacaine.
Gordon-Evans et al (2020) analysed the effect of a bupivacaine liposome injectable suspension (BLIS) on cats undergoing ovariohysterectomy — they hypothesised the BLIS could provide analgesia for 72 hours. The study included 47 cats split into two groups: both groups received their local anaesthetic as an incisional block. The control group consisted of 24 cats that received standard bupivacaine and robenacoxib, and the BLIS group consisted of 23 cats that received BLIS and saline. The results indicated that only one cat from each of the groups required rescue analgesia. In the control group this was in the form of buprenorphine and in the BLIS group was in the form of robenacoxib—neither of these cats was excluded from the study. The study did mention that during the postoperative assessment it was a blinded investigator who assessed the cats. The study was unable to contain the patients for 72 hours so they were unable to prove their hypothesis. Overall the study showed incisional BLIS blocks provide adequate analgesia that is equivalent to a bupivacaine block and two daily robenacoxib injections. This reduces the need for continual postoperative analgesia administration making BLIS a cost-effective analgesia ideal for use in clinics that provide low-cost neutering facilities.
Recommendations for further study
Further study is required for the toxic dose of bupivacaine in cats (Benito et al, 2015); however, this does come with its own ethical dilemma because of the aim of the study to monitor for signs of cardiotoxicity, peak plasma concentrations and to assess the presence of hypotension. Malik and Bradbury (2016) stated that analgesia is underused within the veterinary practice — this could be an area for further investigation to understand if this statement is accurate or if there is a lack of knowledge. Gordon-Evans et al (2020) were unable to determine if BLIS does provide 72 hours of analgesia — a study to investigate the prolonged effects of BLIS in both cats and dogs would be beneficial because of the lack of data to demonstrate the prolonged effects.
Conclusions
Overall veterinary professionals need to be understanding and determined to provide exceptional pain management to their patients. Treating pain as the fourth vital sign, and having set protocols within the veterinary practice, will help to prevent unmanaged pain and the problems that follow, such as reduced immunity, insulin resistance, leucocytosis and malnutrition. Based on the recommendations of Malik and Bradbury (2016) and Richmond (2016) using CMPS-SF will provide a protocol for the postoperative phase and written evidence to justify further analgesia. This information can be communicated back to owners so they can understand how their pet displays pain. All studies agreed that local anaesthesia is economical and straightforward to administer by either the RVN or VS, making it ideal to use in ovariohysterectomy in both dogs and cats. RVNs can be involved in the administration of the local anaesthetic, and should be encouraged as doing so will utilise and specialise their skills. Both Fudge et al (2019) and Steagall et al (2020) agreed the intraperitoneal route is preferred because of the prolonged effect. Based on Vicente and Bergström's (2018) study, a mixture of both bupivacaine and lidocaine should be used to lower dose of each medication required, and provide an early onset of action with a prolonged effect. All studies supported the need to incorporate a local anaesthetic and create a multimodal analgesia approach for all patients undergoing ovariohysterectomy. This will ensure all analgesia medications are complementing each other and less anaesthetic inhalant is required, reducing potential side effects of the general anaesthetic.
KEY POINTS
- There are three steps to successful pain management, including pre-emptive analgesia; in both human and veterinary medicine it has been shown that prevention is the ideal approach to any procedure or treatment.
- Multimodal analgesia, the second step, involves blocking each pathway of pain using three different classes of analgesic medications, including opiates, local anaesthetics and NSAIDs; the third step involves the continuation of analgesia after the procedure.
- Pain scoring systems should be used routinely in all patients regardless of the reason for their attendance to the surgery.
- Ovariohysterectomy is a painful procedure and appropriate analgesia is paramount for the patient's recovery. Multimodal analgesia provides intraoperative and postoperative benefits for the patient and can be incorporated into ovariohysterectomy.
- Multimodal analgesia should be applied to surgeries that are moderate to severe in their pain scale.
- Pain that is inappropriately managed can lead to malnutrition, prolonged recovery, weight loss, wound dehiscence, leucocytosis and insulin resistance, leading to the development of chronic pathological pain, client dissatisfaction and a loss of time and money.


