References
Anaesthesia for head trauma patients
Abstract
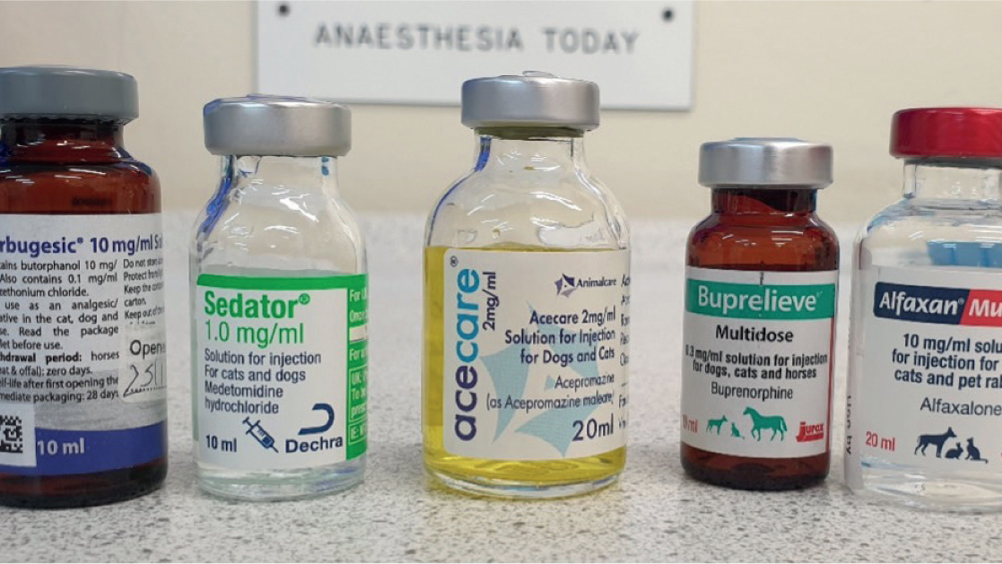
There are many reasons anaesthetising a patient with head trauma may be required. These include for diagnostic imaging, surgery, or it may be required in severe cases to control the patient's ventilation. Many anaesthetic agents cause changes to the blood flow to the brain and therefore may cause further detriment to the patient. Thus, the veterinary nurse assisting the veterinary surgeon with these cases requires a thorough understanding of the physiology of head trauma and the effects of anaesthetic agents on cerebral blood flow, intracranial pressure and the cardiac and respiratory systems, as well as possible neuroprotective benefits that can be gained from the use of some agents.
The skull is unable to expand so any increase in the intracranial pressure (ICP) as a result of an increase in cerebrospinal fluid (CSF) or intracranial blood can have severe consequences such as brain herniation and ultimately death (Bell, 2020). Therefore, there are homeostatic systems in place to tightly regulate the intracranial volume to ensure it remains stable (Bell, 2020). The brain relies on maintenance of intracranial blood volume to meet its high metabolic demands, the cerebral prefusion pressure (CPP) ensures blood is driven into the calvarium to provide oxygen and nutrients and regulates the cerebral blood flow. CPP and mean arterial pressure together determine ICP (Bell, 2020). A trauma to the head will cause an increase in the volume of fluid within the skull because of haemorrhage or oedema; this will cause the CSF and intracranial blood compartments to decrease to maintain ICP. This ultimately results in a reduction in cerebral blood flow and therefore oxygenation and metabolism in the brain (Bell, 2020).
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

