Hypertension, or high blood pressure, is widely reported in humans but is also commonly encountered in small animals. It may go undetected unless there are specific clinical signs, such as retinal detachment. Diagnosis and treatment are based on reliable and repeatable blood pressure measurements, which are usually carried out by a veterinary nurse. In busy practices with numerous time and pressure commitments, blood pressure is often not measured as regularly as it should be, and the number of cases is likely underestimated. Guidelines from both the American College of Veterinary Internal Medicine (ACVIM) and the International Society of Feline Medicine (ISFM) recommend regular screening of dogs and cats, particularly at senior life stage or if there is suspicion of target organ damage. Most commonly, hypertension is secondary to other disease process, such as chronic kidney disease, which may need to be treated alongside the hypertension. Nurses can play an important role in raising the profile of measuring blood pressure within practice and with clients.
Blood pressure
Blood pressure is a measure of cardiac output and systolic vascular resistance. A decrease in blood pressure can occur in a response to a drop in cardiac output, such as serious haemorrhage, a poorly functioning heart, or as a result of a problem with the contractility of blood vessels. To counteract this, the neurohormonal system is activated, secreting renin to constrict blood vessels and increase blood pressure. If renal disease is present, the kidney can produce too much renin, causing hypertension.
The heart pumps blood around the body under pressure. Systolic pressure in the left ventricle should be approximately 120 mmHg, which means that the pressure in the arteries should be around the same. When indirect systolic blood pressure is measured, either using Doppler ultrasonography or oscillometry, the recording measures the force of blood against the artery walls. If the blood pressure reading at the periphery, either at the radial or coccygeal artery, is high, then the pressure in the left ventricle has to match it, which can cause hypertrophy of the left ventricle.
Factors influencing blood pressure measurement
Numerous studies have tried to define the average blood pressure for both dogs and cats, but this is a challenging task, because many things can influence blood pressure measurements (Box 1). For example, defining a standardised blood pressure ‘normal’ range for all dogs is difficult, because breed variations influence blood pressure. It is well known that the resting blood pressure of hounds such as Greyhounds and Deerhounds is approximately 10-20 mmHg higher than that of mongrels (Bodey and Michell, 1996). However, there is no evidence of breed variances in cats. Tables 1 and 2 summarise average blood pressure ranges in conscious dogs and cats and the studies that have investigated them, as reported in the ACVIM consensus statement (Acierno et al, 2018).
Box 1.Factors influencing blood pressure measurements
- Breed of dog
- Temperament of patient
- Patient position
- Measurement method (Doppler, oscillometry, or intra-arterial)
- Different operators
- Operator experience and expertise
Table 1. Average blood pressure (BP) ranges using oscillometry and Doppler ultrasonography in conscious dogs
| Systolic BP (mmHg) | Study size | Original study authors |
|---|---|---|
| Oscillometry | ||
| 131 ± 20 | 1267 | Bodey and Michell (1996) |
| 144 ± 27 | 51 | Coulter et al (1984) |
| 137 ± 15 | 14 | Kallet et al (1997) |
| 150 ± 20 | 28 | Stepien et al (1999) |
| 136 ± 16 | 22 | Meurs et al (2000) |
| 139 ± 16 | 89 | Hoglund et al (2012) |
| Doppler | ||
| 145 ± 23 | 12 | Chalifoux et al (1997) |
| 151 ± 27 | 28 | Stepien et al (1999) |
| 147 ± 25 | 51 | Rondeau et al (2013) |
Adapted from Acierno et al (2018)
Table 2. Average blood pressure (BP) ranges using oscillometry and Doppler ultrasonography in conscious cats
| Systolic BP (mmHg) | Study size | Original study authors |
|---|---|---|
| Oscillometric | ||
| 139 ± 11 | 104 | Bodey et al (1998) |
| 115 ± 10 | 60 | Mishina et al (1999) |
| Doppler | ||
| 118 ± 11 | 33 | Kobayashi et al (1990) |
| 162 ± 19 | 50 | Sparkes et al (1999) |
| 134 ± 16 | 53 | Lin et al (2006) |
| 125 ± 16 | 30 | Dos Reis et al (2014) |
| 133 ± 20 | 113* | Taff in et al (2016) |
| 137±16† | 113 | Quimby et al (2011) |
| 131 ± 18 | 87 | Paige et al (2009) |
| 151 ± 5 | 30 | Chetboul et al (2014) |
| 122 ± 6 | 780 | Payne et al (2017) |
*Includes three cats with renal azotemia. †Data not included in original publication but obtained after a direct approach to the authors. Adapted from Acierno et al (2018)
Age may also influence blood pressure measurements. An increase of 1-3 mmHg has been reported in aging dogs (Bodey and Michell, 1996; Bright and Dentino, 2002), but this has not been repeated. Increased blood pressure in cats over the age of 9 years has been shown (Bijsmans et al, 2015; Payne et al, 2017), but other studies have not found a connection. The effect of sex is also debatable. Bodey and Michell (1996) found that intact male dogs had higher blood pressure than females, and in cats one study showed that entire males had higher blood pressure than neutered and female cats, but the differences were small (Payne et al, 2017). Obesity has not been shown to make a difference to blood pressure readings, but the study by Payne et al (2017) did show that underweight cats had slightly lower blood pressure than those of ideal bodyweight or obese cats.
Hypertension
A diagnosis of hypertension is made when a sustained increase in blood pressure has been recorded. There are two types of hypertension: systemic hypertension and pulmonary hypertension. Increased blood pressure to and from the lungs causes pulmonary hypertension to occur. This is usually secondary to another disease process, such as pulmonary thromboembolism, pulmonary fibrosis, chronic obstructive pulmonary disease, Angiostrongylus vasorum or advanced heart failure. In countries where Dirofiliria immitis is endemic, this can also be a cause of pulmonary hypertension.
Pulmonary hypertension is more common in dogs than cats. Clinical signs include lethargy, cough, dyspnoea or syncope. It is diagnosed by echocardiography, particularly Doppler colour flow, which is used to measure pressures in the pulmonary artery. It is quite often acute in nature, and requires oxygen therapy, minimal stress and treatment of the underlying cause. Sildenafil citrate is used to treat pulmonary hypertension by inhibiting phosphodiesterase, thereby vasodilating the pulmonary vasculature. Prognosis varies according to the underlying cause.
Systemic hypertension is more common in small animal medicine and is categorised into three types: situational hypertension; idiopathic (or primary) hypertension; secondary hypertension.
Situational hypertension
Situational hypertension, or ‘white coat’ hypertension as it may be better known, occurs when stress activates the autonomic nervous system and increases blood pressure. It is difficult to assess exactly how much stress effects blood pressure, and also why some patients will be stressed and exhibit an increase in blood pressure, while other stressed animals do not experience an increased blood pressure. One study recorded blood pressure in 780 apparently healthy cats, and documented blood pressure along with demeanour. A rise in blood pressure was seen with cats in states of increased stress (Payne et al, 2017). Table 3 summarises their findings. Three randomised placebo-controlled studies recently showed that cats can adapt to having their blood pressure measured (Huhtinen et al, 2015; Coleman et al, 2019; Glaus et al, 2019). The placebo groups saw a reduction in blood pressure of 18-28% or to less than 150 mmHg in 28 days. The ACVIM guidelines (Acierno et al, 2018) do not recommend treatment of situational hypertension.
Table 3. Blood pressure and demeanour in cats
| Demeanour | Median systolic blood pressure (mmHg) |
|---|---|
| Calm | 112.8 |
| Cooperative but anxious | 123.2 |
| Nervous, excited, aggressive | 131.6 |
From Payne et al (2017)
Idiopathic hypertension
Idiopathic, or primary, hypertension occurs when no underlying clinical cause can be found for a persistently increased blood pressure. Idiopathic hypertension has been reported on multiple occasions in dogs (Acierno et al, 2018) and three feline studies showed that 13-24% of cats had no clinical reason for their hypertension (Geddes, 2020). A definitive diagnosis of primary hypertension is often challenging, because ruling out situational hypertension, hypertrophic cardiomyopathy or subclinical renal disease may be difficult.
Secondary hypertension
Secondary hypertension occurs when a sustained increase in blood pressure is associated with a disease process, toxin or medication that is known to cause hypertension. Even if the underlying disease is treated, hypertension may persist. In cats and dogs, chronic kidney disease is the most common cause of secondary hypertension (Acierno et al, 2018). Table 4 shows the most common secondary diseases associated with hypertension in dogs and cats.
Table 4. Percentage of cases with secondary hypertension in dogs and cats, according to studies summarised in the American College of Veterinary Internal Medicine guidelines
| Disease | Percentage of hypertensive patients with secondary hypertension |
|---|---|
| Chronic kidney disease | Cats: 19-61% |
| Dogs: 9-93% | |
| Acute kidney disease | Dogs: 15-87% |
| Hyperadrenocorticism | Cats: 19% |
| Dogs: 20-80% | |
| Diabetes mellitus | Cats: 15% |
| Dogs: 24-67% | |
| Hyperthyroidism | Cats: 12-87% |
Adapted from Acierno et al (2018)
Complications: target organ damage
Untreated systemic hypertension can have severe consequences if left untreated. To maintain such high arterial pressures, autoregulatory mechanisms are lost, and this can damage areas that are supplied with a rich arteriolar blood supply, or via sustained increases in systemic vascular resistance. Untreated hypertension can cause small blood vessels to leak and sometimes rupture. The areas particularly at risk are known as target organs and are the kidney, eyes, heart and brain. Table 5 summarises target organ damage.
Table 5. Target organ damage, clinical findings and suggested diagnostic tests
| Tissue | Hypertensive injury | Clinical findings | Diagnostic tests |
|---|---|---|---|
| Kidney | Progression of chronic kidney disease |
|
|
| Eye | Retinopathy/choroidopathy |
|
Ophthalmic examination |
| Heart and blood vessels |
|
|
|
| Brain |
|
|
|
Adapted from Acierno et al (2018)
Kidney damage
Hypertension is most commonly associated with renal disease. Azotaemia was reported in 70% of cats with hypertension (Jepson et al, 2007), approximately 60% of cats diagnosed with chronic kidney disease were hypertensive (Bijsmans et al, 2015). In dogs, strong association has also been established with increased blood pressure, renal injury and shorter survival times (Werner et al, 2008). Proteinuria and hypertension play a significant role in renal damage in dogs and cats and have been linked with a poorer prognosis (Syme et al, 2006; Acierno et al, 2018). Therefore, treatment aims include reducing proteinuria. Albuminuria in cats has also been associated with increased blood pressure (Acierno et al, 2018).
Ocular damage
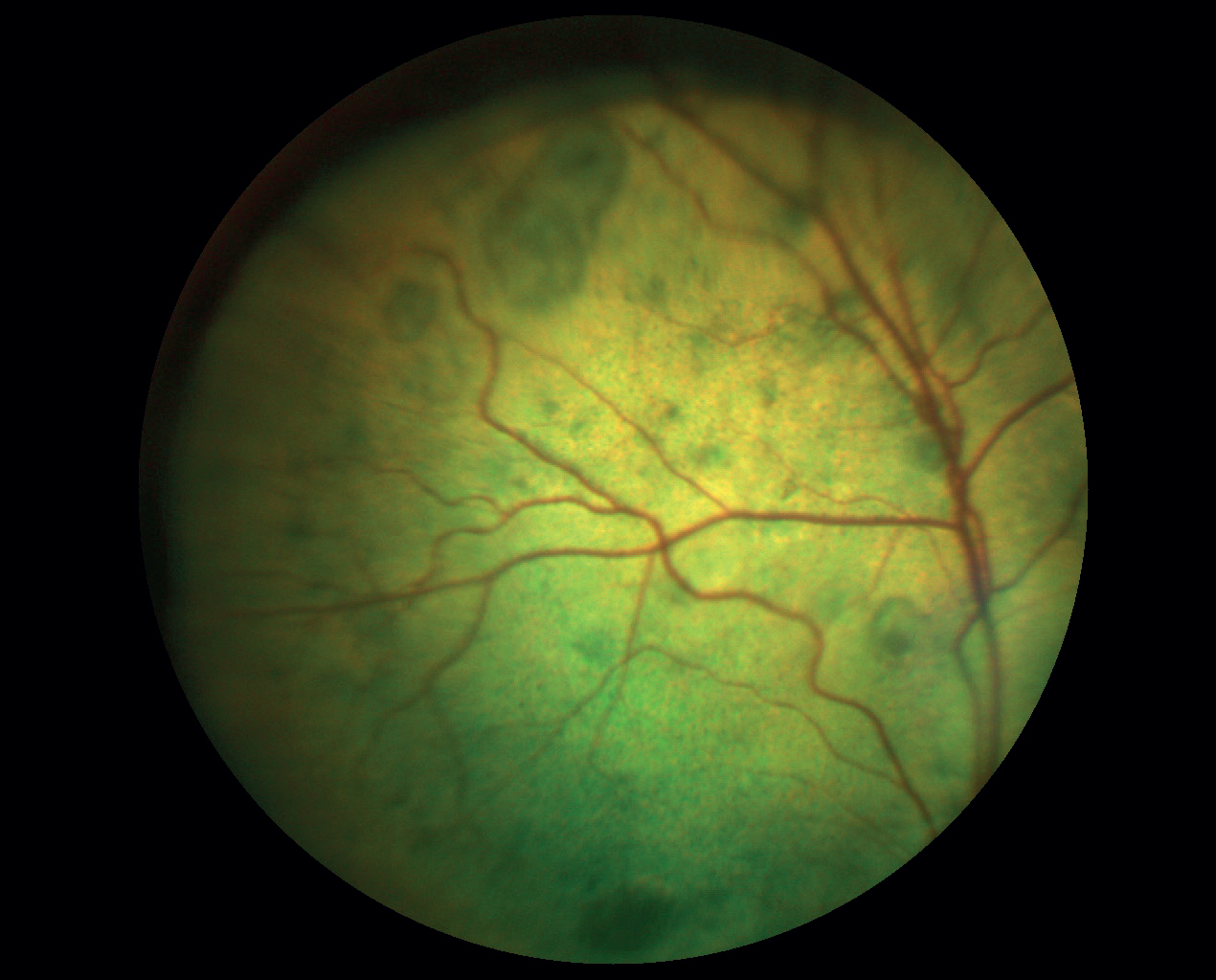
Ocular lesions are found in many dogs and cats, although the degree of injury can vary. Numerous feline studies have shown that 100% of cats have some ocular change (Maggio et al, 2000; Elliot et al, 2001; Chetboul et al, 2003; Sansom et al, 2004). Alarmingly, ocular changes have been recorded with blood pressure measurements as low as 168 mmHg (Sansom et al, 2004). The most common finding is retinal detachment, but haemorrhage, oedema, retinal vessel tortuosity, hyphaema, secondary glaucoma and retinal degeneration have been reported. Return of sight after effective hypertensive treatment used to be seen as unlikely, with one report showing only 13% of cats regained vision (Maggio et al, 2000), but a study of 88 cats showed that sight returned in 57.6% of cats diagnosed with chorioretinopathy after treatment for hypertension (Young et al, 2019). Owing to the high incidence of ocular changes, the ACVIM guidelines recommend fundic examination in all patients with a blood pressure greater than 160 mmHg (Acierno et al, 2018). Figure 1 illustrates focal bullous detachments.
Cardiac changes
Cardiac changes are also a common finding in dogs and cats with systemic hypertension. Continuous increased systemic vascular resistance can cause left ventricular hypertrophy, although the severity of the hypertrophy does not appear to match the degree of hypertension (Taylor et al, 2017). Left ventricular concentric hypertrophy has been documented in 70-85% of cats diagnosed with hypertension (Lesser et al, 1992; Chetboul et al, 2003). Clinical findings include a systolic heart murmur, gallop rhythm, arrhythmias and, in severe but rare cases, congestive heart failure or aortic aneurysm (Taylor et al, 2017).
Neurological changes
Hypertensive encephalopathy has been reported in dogs and cats and occurs as white matter oedema and vascular lesions (Acierno et al, 2018). Neurological signs were reported in 29% (Maggio et al, 2000) and 46% (Littman, 1994) of hypertensive cats. Clinical signs include seizures, lethargy, altered mentation, ataxia, vestibular signs and stroke. Hypertensive encephalopathy is responsive to treatment if caught early (Acierno et al, 2018).
Diagnosis
Diagnosing hypertension relies on exclusion. Haematology, biochemistry, symmetric dimethylarginine (SDMA), total thyroxine (T4) and urinalysis should be measured to rule out concurrent disease. Blood pressure measurement is the primary diagnostic tool, and this should be done according to the ACVIM Consensus Guidelines (Acierno et al, 2018), or the ISFM guidelines (Taylor et al, 2017). Both guidelines are free to access and, by following them, blood pressure measurements can be standardised and repeatable. Figures 2 and 3 show how to take a blood pressure measurement in a dog and cat, minimising stress as much as possible.


When to treat hypertension is the veterinary surgeon’s decision, but both guidelines offer advice to assist with this. They both advise to treat based on the risk of target organ damage. A summary of the ACVIM recommendations is shown in Table 6. Once antihypertensive medication is initiated, regular check-ups are necessary, to assess efficacy of treatment.
Table 6. American College of Veterinary Internal Medicine consensus classification, based on risk of target organ damage
| Classification | Risk of target organ damage | Systolic blood pressure |
|---|---|---|
| Normotensive | Minimal risk | <140 mmHg |
| Prehypertensive | Low risk | 140-159 mmHg |
| Hypertensive | Moderate risk | 160-179 mmHg |
| Severely hypertensive | High risk | >180 mmHg |
From Acierno et al (2018)
Treatment
Treatment of hypertension varies in dogs and cats, and as hypertension is often secondary to another disease process, concurrent treatment may be necessary. The primary goal of antihypertensive therapy is to prevent target organ damage, and decreases in blood pressure should be done gradually. The ACVIM guidelines (Acierno et al, 2018) recommend decreasing blood pressure to 140 mmHg or lower.
In dogs, there are three treatment options; drugs that block the renin-angiotensin-aldosterone system such as angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or calcium-channel blockers. The first-line treatment in dogs is usually an angiotensin-converting enzyme inhibitor, such as benazepril or enalapril. An angiotensin-converting enzyme inhibitor is chosen for two reasons, first because it prevents vasoconstriction (an action of the renin-angiotensin-aldosterone system), and second, because angiotensin-converting enzyme inhibitors decrease proteinuria. Angiotensin II receptor blockers, such as telmisartan, also decrease proteinuria, but because veterinary surgeons are more experienced with angiotensin-converting enzyme inhibitors, they are usually preferred as a first-line treatment (Acierno et al, 2018). However, angiotensin-converting enzyme inhibitors may not completely blockade the renin-angiotensin-aldosterone system, and so angiotensin II receptor blockers may be indicated also. Calcium-channel blockers are not recommended as a monotherapy in dogs with hypertension but may be combined with an angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker.
There are two main groups used in the treatment of hypertension in cats. Traditionally, calcium-channel blockers, such as amlodipine besylate have been prescribed. While this effectively reduces blood pressure, long-term studies have not indicated a change in survival times (Acierno et al, 2018). However, as increased proteinuria has been associated with reducing survival times, a newer drug has been adopted. First licensed for the treatment of proteinuria in cats with chronic kidney disease, the angiotensin II receptor blocker telmisartan has now been licensed for the treatment of systemic hypertension in cats (European Medicines Agency, 2012), and has been shown to reduce blood pressure and proteinuria (Girens and Swift, 2019).
The hypertensive emergency
Hypertensive emergencies occur in humans and in dogs and cats. It is a rare presentation in both fields, and so both suffer from a lack of supporting literature and guidelines. Furthermore, patient presentation varies considerably. In the first retrospective study investigating hypertensive emergencies in small animals, Beeston et al (2022) defined a hypertensive crisis by a sustained blood pressure >180 mmHg, accompanied by some of the following neurological presentations of target organ damage:
- Acute onset seizures
- Altered mentation
- Lateral recumbency
- Blindness.
In this study, 15 cases fitted the criteria from 2003-2019 at a referral hospital. There were seven dogs and six cats. Acute kidney disease was the most common cause in both species. There are no evidence-based treatment recommendations for a hypertensive crisis in dogs or cats. Beeston et al (2022) recommend direct blood pressure monitoring to closely monitor the efficacy of treatment. In the study, amlodipine was the most commonly prescribed medication.
Acierno et al (2018) recommended amlodipine for cases with hypertensive urgency, but not for hypertensive emergencies. This is possibly because it is an oral medication, and has a longer onset of action. In human medicine clevidipine, a parenteral alternative to amlodipine, is used, but there is no literature detailing its use in veterinary medicine.
If amlodipine has not significantly reduced blood pressure, then alternative medications may be considered. In one study, hydralazine was the next most used (Beeston et al, 2022), even though there is no literature to support its use. The third most common medication was sodium nitroprusside. Used in severe acute heart failure, there is no evidence to support its use in a hypertensive emergency. Sodium nitroprusside is difficult to titrate so needs constant observation because it can result in hypotension. It is also unstable in light, so the whole bag and fluid line needs to be covered. Finally, prolonged use can cause cyanide toxicity. One cat in the study received a hyperosmolar agent. However hyperosmolar agents are very powerful, and its use can cause hypertension with concurrent bradycardia (a phenomena known as the Cushing reflex). There are other drugs used in human medicine, such as labetalol and fenoldopam, which may be used in the future, but at the time of writing, there has been no mention of them being used in veterinary medicine.
Nursing role
The nurse’s role is crucial in the diagnosis and treatment of systemic hypertension. Measurement of blood pressure is often delegated to the nurse, and it is their responsibility to ensure that results are recorded, reliable and repeatable. The wide variations in average blood pressure measurements seen in Tables 1 and 2 show that standardised technique, operator experience and equipment are vital to determine baselines and assess medication efficacy.
Client education is vital, and nurses can be used to explain the importance of consistent administration of medication. The ACVIM guidelines recommend that owners are given a working knowledge of hypertension and its consequences, and suggest telling owners the actual blood pressure readings, to encourage their ‘buy in’. Owner compliance can be difficult because hypertension is often a hidden disease, and so helping owners understand the drastic consequences of target organ damage is paramount.
Conclusions
Systemic hypertension is often a chronic, progressive and hidden disease, unless severe target organ damage is present. ACVIM guidelines suggest all senior patients have their blood pressure recorded to establish baseline readings and detect early changes. Treatment is aimed at preventing target organ damage, which can be irreversible. Client education is important, but also practice behaviour. Nurses are in a pivotal role in practice to set up and run blood pressure clinics and instigate best-practice measurement taking.
Key points
- Free reputable guidelines are available to standardise blood pressure measurement, making numbers repeatable and reliable.
- Exact blood pressure ranges are difficult to define, so finding a baseline for each individual is important.
- Nurses can encourage blood pressure screening through clinics and proactively looking through the practice diary for senior pets.
- Target organ damage is a concern for uncontrolled hypertension.
- Target organ damage affects the kidneys, eyes, brain and heart.
- Secondary hypertension is the most common of the three types, and most cases are the result of chronic kidney disease.


