In order to deal with wounds effectively it is essential that veterinary staff have a good understanding of the normal processes involved in wound healing. In all wounds, irrespective of their aetiology, the healing process will generally be the same.
There are three main phases to wound healing: haemostasis and inflammation, proliferation, and maturation and remodeling.
Whenever dealing with a wound consideration should always be given to the fact that normal wound healing phases are interlinked and can be affected by a variety of patient, environmental and surgeon factors, e.g. the systemic health of the patient, wound environment. Also when dealing with feline wounds the clinician should be reminded that they will heal differently to canine wounds as they have different cutaneous vascular supply, and their granulation tissue production, epithelialisation and overall healing times will be decreased (Demetriou and Stein, 2011).
Options for wound closure
When considering the closure of wounds, the timing of closure can be assigned to various categories. First either primary closure or first intention, whereby the wound is immediately sutured closed at the time of creation, e.g. following mass removal, or where a clean wound or clean-contaminated wound has been debrided and is deemed suitable for immediate closure without tension. The classification for open wound healing includes:
When selecting which wound closure technique is most appropriate for a wound various factors need to be taken into consideration, including wound aetiology, wound size and location and the degree of contamination present. It is vital to consider the degree of contamination in any wound when selecting the most appropriate technique for closure and assign an appropriate classification to the wound (Table 1).
| Category | Definition | Example |
|---|---|---|
| Clean | Wounds created under aseptic conditions (non-traumatic, surgically created wounds) No entry into gastrointestinal, respiratory, genitourinary or oropharyngeal body cavities | Skin mass removal |
| Clean-contaminated | Operative wounds with minimal contamination where level of contamination has been removed or reduced to a biologically insignificant level May involve entry into gastrointestinal, respiratory, genitourinary or oropharyngeal body cavities, but with no evidence of infection | Gastrotomy (minimal spillage) |
| Contaminated | Heavily contaminated traumatic wounds Operative wounds with major break in aseptic technique, | Fresh traumatic wounds Spillage of gastrointestinal contents during an enterotomy |
| Dirty | Active infection present in traumatic wound Perforated viscus | Dog bite wounds |
Complications in wound healing
With appropriate management, the vast majority of patients' wounds will heal quickly, and without any problems. In veterinary medicine a patient's wounds can be considered easier to heal than human wounds because of the elasticity of their skin, which allows contraction to play a huge role in wound healing. In addition, veterinary practitioners are not faced with some of the issues human healthcare practitioners are, such as smoking and alcohol intake, which are known to decrease wound healing rates (Ramasastry, 2005).
Non-healing wounds can arise due to a single cause, or multiple factors, and the successful management of these cases will ultimately require the treatment, or removal of these problems (Demitriou and Stein, 2011).
Poor nutrition
Adequate, and correct nutrition are essential for normal wound healing but despite this requirement, malnutrition is a fairly uncommon cause of wound complications and delayed wound healing in veterinary patients. Glucose and protein are vital for the normal wound healing process to occur (Demitriou et al, 1985).
Following injury, numerous metabolic changes occur that can contribute to impaired wound healing and poor host defenses. Malnutrition can encompass a host of factors from poor nutritional intake to overall metabolic equilibrium. Studies over the past century have shown changes in energy, carbohydrate, protein, fat, vitamin, and mineral metabolism after wounding or injury, each affecting the healing process (Levenson and Demetriou, 1992).
Nutritional deficiencies can result in delayed wound healing and may also decrease the body's ability to fight infection (Stanley, 2012). Patients with wounds will have increased calorie requirements, but it is also important to ensure adequate levels of vitamin C, vitamin B6, iron, vitamin B12, folate and zinc are provided as these are vital for cell division and growth (Demetriou and Stein, 2011). Protein levels of less than 60 g/litre slow the healing process, while levels below 55 g/litre increase the risk of wound disruption to 70%. Furthermore, sufficient calories must be provided to help spare body protein from being metabolised (Demetriou and Stein, 2011).
Non-healing wounds
Failure in wound contraction
The failure of wound contraction to occur has two main causes: insufficient skin being available locally (thus causing peripheral counter tension) and restrictive fibrosis, which prevents skin advancement. When such situations arise the only solution may be surgical intervention and/or reconstruction. This can include undermining of the surrounding skin, therefore meaning less tension across the wound bed, through to more complex procedures such as flaps and grafts (Demetriou and Stein, 2011).
Failure in epithelialisation
In order for reepithelialisation to occur, the wound requires a viable vascular bed. The most common cause of failure of epithelialisation is repeated trauma to the wound surface. This can arise due to high movement of the contact layer, or trauma over areas such as bony prominences or footpads. This type of damage to the wound bed will require debridement of necrotic tissue and fibrotic scar tissue (Demetriou and Stein, 2011). This issue in wound healing highlights the importance of good knowledge of the wound healing process, an understanding of wound dressings available, and excellent skills in dressing placement/bandaging.
Indolent ‘pocket’ wounds
A pocket wound is one where a wound which has been closed via primary intention (suturing) appears to have healed normally but the subcutis fails to cross-link with the underlying granulation bed (Demetriou and Stein, 2011). It is not uncommon in this situation for complete dehiscence to occur when tension is placed on the closure (e.g. grooming or jumping).
Common examples of when such pocket wounds are likely to occur include wounds in the inguinal, axillary and flank areas (Figure 1), bite wounds (Figure 2 and 3), and wounds following major tumour resection. Successful management requires control of infection, excision of the scar border and careful release of incisions in the restrictive dermal layer to allow advancement of the skin. A period of open wound management is likely to be required in order to treat any infection, and to ensure a healthy granulation bed is present. When closing the wound the skin margins should be sutured directly to each other or firmly anchored to the granulation bed to promote wound closure, and any dead space may be managed with drains (Demetriou and Stein, 2011). In complicated cases, the omentum can be mobilised through the abdominal wound to fill the pocket wound with viable vascular tissue and to obliterate dead space.



Wound scarring and contracture
During open wound healing, fibroblast, myofibroblasts, and collagen of granulation tissue are responsible for the contraction that occurs during the repair stage of wound healing (Swaim and Henderson, 1997; Swain et al, 2001). When the contraction of second-intention healing of a large wound takes place over the flexion surface of a joint, folding or bunching and bonding of collagen fibers may occur with flexion. The result is contracture such that joint extension is severely limited, which can lead to disuse atrophy of muscles, or it can result in restriction of function, e.g. wounds around the eye, external nares and preputial orifice. Treatment may include scar excision, partial myotomies, skin flaps or free skin graft coverage, and physical therapy (best achieved by early resumption of normal activity) may be required once a contracture has developed (Demetriou and Stein, 2011). This complication is best prevented by not allowing wounds over joints and other ‘mobile’ areas to heal by secondary intention.
Infection
When infection is present within a wound, this will cause inhibition of wound healing throughout all stages of the wound healing process. In order to identify infection a deep tissue culture should be obtained, this is preferable to a surface swab as surface contaminants do not truly reflect infection (Demetriou and Stein, 2011). Infection is thought to be present in around 3% of all wounds at the time of suture removal (Eugster et al, 2004), but infection rates are very variable, dependent on the degree of wound contamination. The aetiology of the wound also will affect the likelihood of infection occurring, with bite wounds having a high probability of infection due to the wound and its surrounding tissues creating the ideal environment for bacterial replication, along with poor drainage and a hypoxic environment (Demetriou and Stein, 2011). There are also surgical causes of infection, e.g. duration of the procedure, number of theatre staff, placement of surgical drains, suture material, underlying disease and the use of propofol, have all been associated with increased incidence in surgical site infections in veterinary patients (Demetriou and Stein, 2011). When faced with chronic wound infections, where a purulent discharge is present, a multimodal approach to dealing with infection is recommended. Demetriou and Stein (2011) recommend the following approach:
Drugs and chemical ulcers
Perivascular injection of some intravenous drugs (e.g. pentobarbital sodium, vincristine, doxorubicin) may cause necrosis and tissue slough as well as a chronic open wound (Swaim and Angarano, 1990) (Figure 4). The size and severity of the wound are dependent on the type of medication, its volume and pH, and whether an attempt was made to prevent an impending lesion. Dependent on the drug that has extravasated, local infiltration (e.g. with anti-inflammatory drugs/corticosteroids, sterile saline and lidocaine) or excision of the whole area is recommended. Corticosteroids are potent anti-inflammatory agents, but reduction of inflammation decelerates the early wound healing process and increases the risk of infection (Demetriou and Stein, 2011).

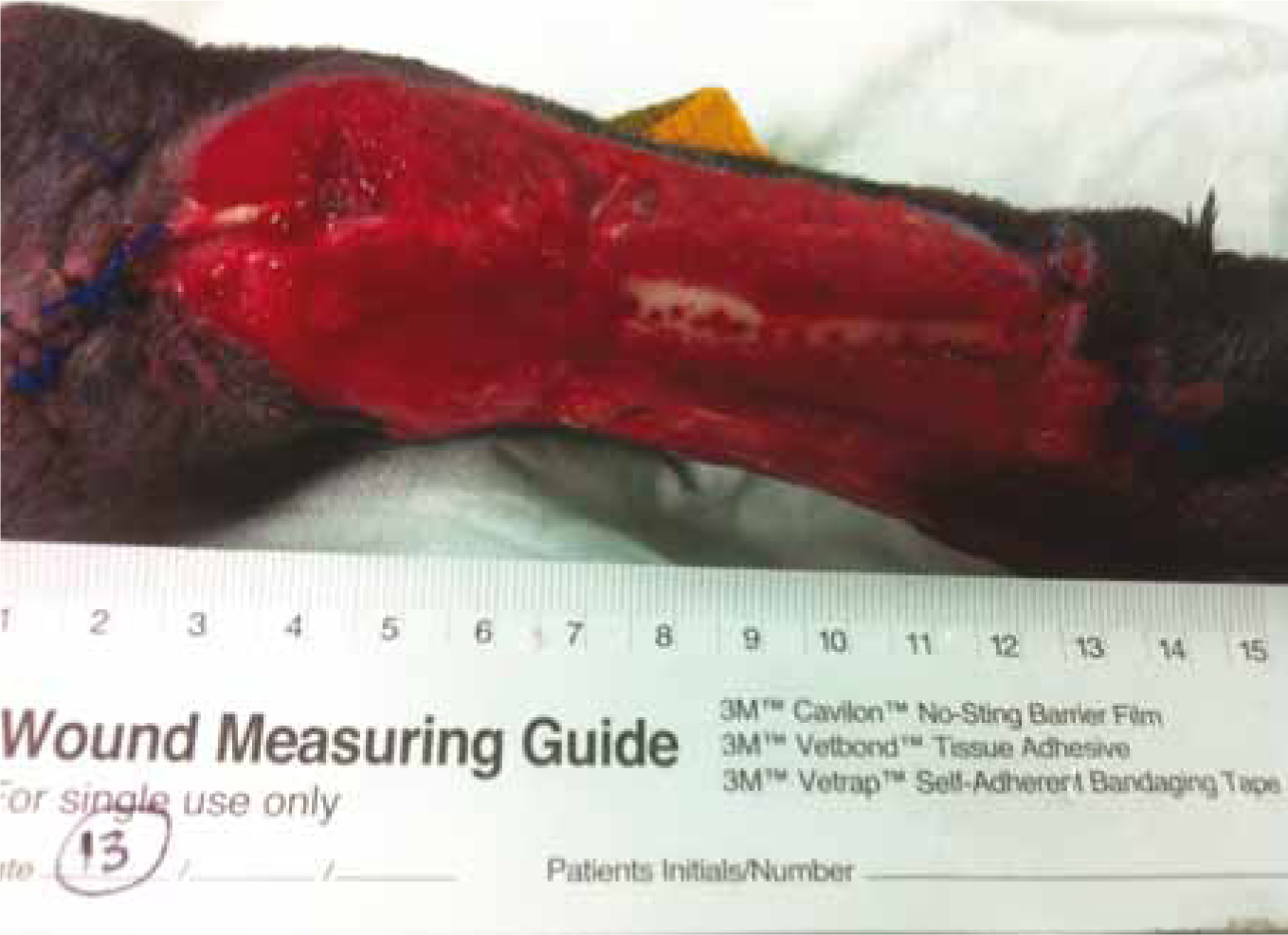
Exposed bone
When dealing with shearing injuries to the lower limbs, it is not uncommon for exposed bone to be present (Figure 5). Exposed bone is often encountered in distal limb degloving wounds and inhibits wound contraction and epithelialisation (Bradley et al, 1998). When allowed to heal by second intention, a bed of granulation tissue is required for second-intention healing to progress (Swaim and Henderson, 1997). During the wound healing process the majority of exposed bone will become covered with granulation tissue (Figure 5–9) that arises from the viable periosteum or viable soft tissues adjacent to the bone surfaces, but there is always the risk of potential for osteomyelitis or sequestrum formation. One useful technique is to drill a number of small holes into the vascular medullary canal of the bone (forage) (Figure 6), which will promote granulation tissue formation (Demitriou and Stein, 2011). This obviously needs to be done carefully, to ensure the bone is not weakened, resulting in fracture.




Underlying metabolic disease
An awareness of any underlying disease should be at the forefront of any clinician's mind when dealing with difficult to heal wounds. Three underlying diseases that can affect wound healing are Cushing's syndrome, diabetes mellitus, and hypothyroidism. Cushing's syndrome, or hyperadrenocorticism, may be a spontaneous pituitary-related disorder manifested by a collection of clinical and biochemical abnormalities, or it may be iatrogenic. Cushing's syndrome arises where there is an overproduction of cortisol by the adrenal cortices or prolonged administration of corticosteroids, respectively (Kintzer et al, 2000). In cases of Cushing's syndrome the negative effect on wound healing would be similar to what is seen with the effects of corticosteroids on healing.
Diabetes in human beings has a marked effect on wound healing related to a combination of peripheral neuropathy and angiopathy. There are also abnormalities in leukocyte function, cell adherence, chemotaxis, and collagen synthesis (Amalsadvala and Swaim, 2006). Although diabetes has not been reported to cause complications in surgery or delayed wound repair in animals, the possibility should be considered. Diabetic animals are thought to be more susceptible to wound infections because of compromised leukocyte function. Additionally human diabetic patients frequently develop non-healing chronic wounds due to neuropathic and angiopathic effects of the disease, as well as abnormalities of collagen synthesis (Hosgood, 2003). Hypothyroidism may also have a negative effect on wound healing. A thyroid function test should be included in the evaluation of chronic wounds. Swaim et al (1991) found hypothyroidism to be associated with the chronic infection or wounds associated with chronic fibrosing interdigital pyoderma.
Wound dehiscence
Dehiscence is defined as the breakdown of a surgically closed wound immediately after closure (Figure 10). Signs of a problem incision may be erythema, oedema or pain (Remedies, 1999) with signs of imminent wound dehiscence including necrosis of the skin edges, extensive cutaneous bruising, the presence of serum beneath the skin and serosanguineous discharge from the suture line (Demitriou and Stein, 2011). Demitriou and Stein (2011) listed the most common causes of wound dehiscence as:

Postoperative haemorrhage and haematomas
The presence of postoperative haemorrhage, or haematoma formation, may delay wound healing by putting pressure on suture lines, providing a rich environment for infection and causing discomfort to the patient, thus resulting in self trauma (Swain, 1980). In addition to the indirect effect on wound tension, there is experimental evidence that postoperative haematoma formation can directly affect flap survival where reconstructive surgery has been performed (Hillelson et al, 1980). Adherence to Halstead's principles, including effective haemostasis, can help to prevent this. Minor incisional haemorrhage can be controlled with direct manual pressure for 10 to 15 minutes, but moderate to severe haemorrhage will require further intervention (Demitriou and Stein, 2011). Conservative management involving placement of pressure bandages, movement restriction and fluid deficit replacement can be instituted initially if the patient is stable. In more severe cases of haemorrhage, or those not responding to conservative management, surgical intervention may be required to identify the source and provide definitive haemostasis.
Management strategies
There are a number of techniques that can be used as part of a wound management protocol to reduce the incidence of postoperative wound complications.
Active or passive surgical drains
Drains can be used to eliminate dead space and to remove accumulated fluid, but it is vital they are used correctly, as their placement is no substitute for inadequate wound lavage and debridement. Additionally, incorrect placement can increase the infection rate, so it is essential that they be handled with strict asepsis. Certain guidelines should be adhered to when placing and maintaining surgical drains:
Flaps and grafts
The closure of larger skin deficits may require more extensive mobilisation of skin into skin flaps in order to ensure the closed wound is not under excess tension (Figure 11). Skin flaps are classed by their vascular supply: subdermal plexus flaps and axial pattern flaps.

Subdermal plexus flaps have a blood supply via the subdermal plexus which is maintained at their cutaneous attachment. They are raised adjacent to a wound and are useful in wounds located close to structures such as eyelids, prepuce, and the anus (Tatton, 2007).
Axial pattern flaps take advantage of the anatomy of the blood supply to the skin by incorporating a direct cutaneous artery (DCA) and vein in their design (Figure 12).

Subdermal plexus and axial pattern flaps are relatively resistant to infection and provide full-thickness skin coverage without depending on early immobilisation and neovascularisation to ensure survival (as is the case with skin grafts). They are particularly useful in areas where padding and skin durability are necessary. Skin grafting requires a graft bed that has sufficient blood supply to sustain it and they should not be placed over contaminated or infected surfaces (Demitriou and Stein, 2011).
Omentalisation
Chronic non-healing wounds in cats and dogs can be treated with omentalisation, which is used to obliterate dead space, provide blood supply and control infection. In veterinary surgery, omentum can be used: to aid reconstruction of wounded tissue; to provide drainage of lymphoedema; to seal abdominal (and thoracic) viscera (Hosgood, 1990); and to aid in the management of prostatic abscesses (White and Williams, 1995) and retention cysts (Bray et al, 1997). Omentalisation involves passing the created omental pedicle (of a suitable length to reach the wound) through the ventral or lateral abdominal wall into the wound via a subcutaneous tunnel (Figure 13). This technique has been used successfully for non-healing axillary wounds where previous attempts to close the wound failed. An omental flap can be combined with skin flaps (e.g. omocervical skin or superficial cervical or thoracodorsal axial pattern flaps). Possible complications include intestinal herniation, or seroma or abscess formation (Demitriou and Stein, 2011).

Novel approaches
Laser irradiation
Low-level laser therapy at a 632 nm wavelength shows promise in stimulating chronic and hard to heal wounds as it has a biostimulative and wound healing effect. There is evidence that laser therapy at or near this wavelength stimulates wound healing by inducing cellular proliferation, collagen synthesis, growth factor release, DNA synthesis, and stimulates vasodilation and lymph drainage (Demitriou and Stein, 2011). At this wavelength, the therapy is rapid and painless. There are varieties of veterinary and human products available that offer this modality.
Negative pressure wound therapy (NPWT)/vacuum-assisted closure (VAC)
NPWT or VAC is still a fairly new technique in veterinary medicine and is a useful, easily applicable procedure for managing open and grafted wounds (Figure 14). It involves applying controlled subatmospheric (intermittent or continuous) pressure via an open-pore foam dressing. This accelerates debridement, stimulates cell proliferation, promotes early resolution of infection and angiogenesis, increases wound contraction and improves healing (Demitriou and Stein, 2011). The use of NPWT/VAC has been described for the treatment of patients with various wounds or different aetiologies, including in dogs for traumatic, distal extremity shearing injuries and in cats for traumatic dorsal and large thigh wounds (Owen et al, 2009).

Antimicrobial dressings
Whenever dealing with difficult to heal wounds it is vitally important to select an appropriate dressing. Dressing selection needs to take into account numerous factors including patient history, systemic health, wound aetiology and wound location, in order to ascertain the reason why the wound is not healing or has not healed properly. For wounds where infection is a concern the use of a dressing designed to control, and/or prevent infection, is useful. Wound infection has been well recognised as a factor involved in prolonged wound healing. Wound infection is seen to prolong the inflammatory phase of wound healing, resulting in pain and discomfort to the patient, and unless correctly treated can lead to serious and potentially fatal systemic sepsis. Such dressings can include antimicrobial dressings, for example AMD Foam (Covidien) which is impregnated with polyhexamethylene biguanide (PHMB), manuka honey, e.g. Activon, (Dechra) or Kruuse manuka honey dressings, or silver impregnated dressings, e.g. Acticoat (Smith and Nephew).
Conclusion
The process of wound healing commences immediately following injury, and comprises a complex, finely tubed continuum of stages (i.e. inflammatory, debridement, repair, maturation). These stages involve a synchronised process of molecular and biochemical events at the cellular level, which will cumulate in a healed wound. If any component of the healing process does not occur as it should this can result in delayed healing and chronic or indolent wounds. It is vital the clinician can identify potential agents, which may contribute to this delayed wound healing, and understand how they can be overcome in order to gain a successful outcome.

