References
How to get the most from blood samples: a guide to producing diagnostic blood smears
Abstract
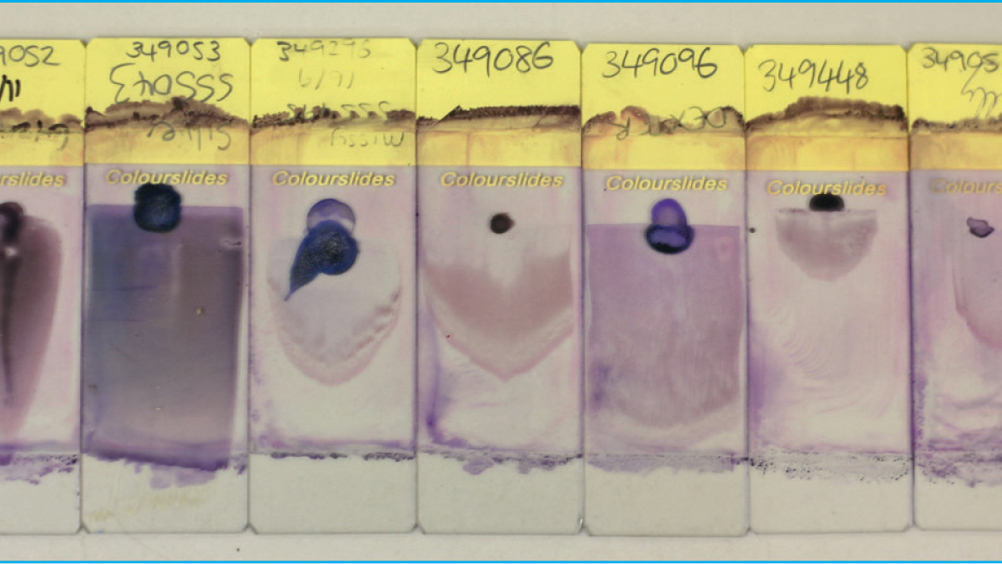
The production of high-quality diagnostic blood smears is a skill often overlooked in first opinion veterinary practices despite their usefulness in providing diagnostic information that would otherwise be omitted from results generated from automated analysers. Well made, well stained diagnostic blood smears can instantly provide vital information regarding the health of the patient and even provide a diagnosis. However, making quality blood smears is open to intraspecific and interspecific observer error and therefore this article aims to provide best practice guidelines along with a comprehensive troubleshooting guide to aid veterinary clinicians, nurses, technicians and students in the production of diagnostic blood smears.
The blood smear is a thin layer of blood smeared on a microscope slide which is a simple but highly informative haematological tool in the screening, diagnosis and monitoring of disease progression (Adewoyin and Nwogoh, 2014).
Significant advances in technology and the advent of sophisticated automated haematology analysers both in-house (e.g. IDEXX LaserCyte Dx) and diagnostic laboratories have not eliminated the need for microscopic evaluation of a well prepared, well stained peripheral blood smear which still forms the cornerstone of diagnostic veterinary haematology. Examination of a diagnostic blood smear by a skilled laboratory technician is an invaluable tool (Park and Shafer, 2014) and often yields significant information regarding the health and diagnosis of a patient that would otherwise be missed. In the authors' experience, it is not uncommon for an unhealthy patient to have automated haematology values which fall within the reference intervals, and yet have significant pathology obvious on evaluation of a blood smear.
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

