References
Pruritus in dogs and cats part 2: allergic causes of pruritus and the allergic patient
Abstract
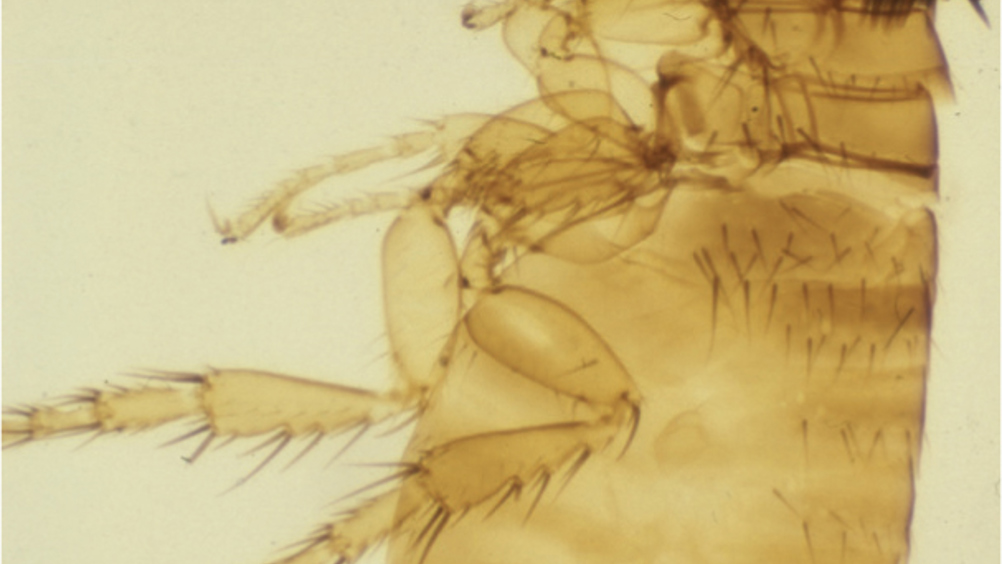
There are many causes of pruritus in domesticated dogs and cats and in this article, the second part of three papers devoted to the subject, the major allergic (hypersensitive) causes are discussed. Despite the tempting tendency to consider ectoparasites a major cause of pruritus in pets, the advent of a number of reliable, safe, effective and long-lasting ectoparasiticides into the veterinary market in recent decades, has meant that the average dog and cat, treated regularly and prophylactically for fleas, ticks and mites, is far less likely to become infested by such parasites. Consequently, allergic causes of itching have become relatively more likely to be seen in general practice. It is therefore important for both veterinary surgeons and nurses to recognise the historical and clinical features of these skin diseases, to allow an appropriate diagnostic and treatment plan to be discussed by the veterinary team and with the client.
In part 1 of this three-part article on pruritus in dogs and cats, pruritus was defined and the general approach to the itchy canine and feline patient was discussed (Curtis, 2022). This second part discusses the allergic causes of pruritus in small animal patients, the approach to these patients, and how a diagnosis of allergic skin disease is made.
The word ‘allergy’ (aka ‘hypersensitivity’) originates from the Greek word ‘allos’, which means ‘other’, pertaining to the pathological process resulting from an aberrant immune response in an allergic individual, following exposure to non-self (‘other’) ‘allergens’. In dogs and cats, as in humans, the commonest allergens that have been described are proteins derived from insects (e.g. flea bite or midge bite hypersensitivity, respectively), the environment (e.g. housedust, dust mites and pollens) and food (e.g. animal or plant proteins) (Miller et al, 2013). These broad groups will be dealt with in turn, and their various historical and clinical manifestations, plus diagnostic and management methods, will be discussed.
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

