On 1 May, Albert, a 6-year-old male neutered whippet, presented after a road traffic accident, with a degloving injury to the medial right metacarpus and lameness of the right foreleg (Figure 1). The patient was triaged by the registered veterinary nurse on duty. This assessment found no severe detriment to the airways, raised respiration rate and normal function of circulatory system, although an obvious leg wound had the potential to cause haemorrhage if managed incorrectly. Further assessment of the major body systems found no neurological or mentation deficits or deviations from normothermia, although gait was severely affected by the injured forelimb. Once this limb was radiographed conscious, it was determined by the on duty veterinary surgeon to have a fracture of the radius and digit 1 metacarpus. Owing to the location of the island clinic and availability of sea or air transport to a veterinary surgeon for theatre time, a Robert Jones bandage was applied over a hydrogel non-medicated wound gel (Intrasite) and hydrocellular conforming dressing with moisture retaining properties (Allevyn). This dressing type was chosen as the decision of limb salvage versus amputation surgery had not been made at this stage. Pain relief was given using buprenorphine at a dose of 0.02 mg/kg intramuscularly, meloxicam at a dose of 0.2 mg/kg subcutaneously and Synulox at a dose of 8.75 mg/kg subcutaneously. Air transport to the closest clinic with a veterinary surgeon was arranged for the following day, with amputation surgery scheduled 2 days post-road traffic accident. Pain relief was scheduled immediately before transport so Albert would have sufficient analgesia until admission at the receiving clinic.

Albert was accompanied on the flight (Figure 2) with one of the clinic registered veterinary nurses rather than the owner. This was because of the concern that witnessing the road traffic accident and associated injuries would be traumatic for the client (Fekadu et al, 2019; Priya et al, 2021; Lebimoyo and Olibamoyo, 2023), and allowed the registered veterinary nurse to continually monitor the patient throughout travel.

Surgical options
When considering the metacarpal fracture, either surgical or conservative management techniques could have been used with similar results, as digit 1 was affected, which is not weight-bearing (Kapatkin et al, 2000; Rosselló et al, 2022). However, this was superseded by the consideration of the radius fracture.
Woods and Perry (2017a) discussed the limb salvaging techniques used when fixing a radial and ulna fracture, alongside their numerous complications and varied prognosis, which is affected by preoperative planning of both the surgery itself and the postoperative plan to follow. Failure to consider these long-term cases thoroughly increases the incidence of failure of limb salvaging surgery (Woods and Perry, 2017b). One option for salvaging surgery would be a T locking plate or traditional bone plate at the site of the distal radial fracture (Namreen et al, 2022). A number of limb salvaging techniques can result in later amputation surgery, particularly if the patient experiences a surgical site infection, or is of an older age (Wustefeld-Janssens et al, 2020), where the incidence of fracture repair failures can be high (Menghini et al, 2023).
An alternative would have been to amputate the distal limb but not the scapula. This could create further gait abnormalities and elephant leg as a result of oedema (Basnet and Aryal, 2019), although it may provide a site for a prosthesis. Some fixed prosthesis studies show good results short term; however, insufficient long-term data are available (Fitzpatrick et al, 2011). In this case, the management of a prosthesis was deemed unsuitable for the home care situation. Additionally, salvage of the scapula would lead to muscle wastage around the scapular spine, whereas total scapular removal prevents this (Basnet and Aryal, 2019). This was the reasoning behind the limb amputation with total scapulectomy in this patient's case.
In contrast with limb salvaging surgery, Smith (2020) highlighted how ‘patients generally deal well with limb amputation and can begin to ambulate within hours of surgery’, which in this case was an important consideration, as the patient's home situation was not suitable for long-term crate rest, immobilisation or the repeated veterinary visits likely to be required post-limb salvaging surgery. Additionally, postoperative amputation complications are deemed low incidence and usually minor (Raske et al, 2015).
In studies, owner satisfaction of limb amputation has been fair to good, with the minority who would not elect for amputation had the same scenario occurred again, having experienced death of the pet within 183 days of amputation surgery (Wagner et al, 2022).
Menchetti et al (2017; 2022) discussed the potential of ‘phantom limb’ pain as seen in human amputees in both cats and dogs, although in both studies the time between pre-amputation diagnosis and amputation surgery was a risk factor which increased the likelihood of the patient experiencing post-amputation pain typical of the phantom complex. Additionally, phantom complex is considered to be more severe when the preoperative pain is chronic, severe and without sufficient analgesia before surgery (West et al, 2009). In Albert's case, the time between diagnosis and amputation was very short, and analgesia was provided throughout the preoperative period, so this is unlikely to be an issue, although this is something that nurses should monitor for. Signs of phantom complex are similar to normal post-surgery pain symptoms (Menchetti et al, 2022) including stump pain, phantom limb pain and phantom limb sensation (Menchetti et al, 2017), as well as residual limb sensation, any of which may express as restlessness, sleep disturbances, sudden vocalisation, panic or anxiety or compulsive grooming (Boesch et al, 2021).
Right forelimb amputation surgery was opted to include scapulectomy, as in the case of Basnet and Aryal (2019), because of the extensive damage to the metacarpal bones. The patient had both subcutaneous and tension relieving Vicryl sutures (2/0 and 3/0) and PDS (2/0) skin sutures. Bradycardia during surgery prompted the use of atropine and the patient crashed twice immediately following surgery, but was quickly recovered with efficient cardiopulmonary resuscitation, although recovery from anaesthesia was unusually prolonged (45 minutes). The patient was hospitalised for 2 days for monitoring. He remained stable throughout, with initial anorexia resolving with metoclopramide 0.25 mg/kg once daily subcutaneously and omeprazole at 10 mg/15kg once daily orally. Pain relief was continued with buprenorphine at a dose of 0.06 mg/kg three times daily and antibiotic cover continued as marbofloxacin (Marbocyl) at 2 mg/kg once daily and Synulox injections once daily as admission dose because of the dirty nature of the traumatic injury. Billas et al (2022) found the incidence of surgical site infections increased with traumatic wounds requiring amputation, which supports the use of prophylactic antibiotic cover as in this patient's case.
Analgesia
Smith (2020) discussed the importance of analgesia perioperatively, highlighting the allodynia and hyperalgesia encountered with insufficient pain management, as well as the prolonged recovery period and unsatisfactory welfare of the patient in these cases. Appropriate analgesia uses multimodal combinations to give an anaesthetic-sparing effect during surgery. Lower doses of medications required reduces or negates their side effects (Walsh, 2020) and perioperatively leads to a pain-free recovery (West et al, 2009; Smith, 2020). This should include a combination of opioids, non-steroidal anti-inflammatory drugs (NSAIDs), supplementary medications such as an alpha agonist or anxiolytic (Hoad, 2014) and local analgesia (Walsh, 2020). Ketamine or fentanyl are reasonable choices for opioids after orthopaedic surgery (Monkman, 2016), or a morphine-lidocaine-ketamine infusion alternative avoids the ‘peaks and troughs’ that intramuscular injections may cause, although this infusion has not been validated in dogs (West et al, 2009). In this case both buprenorphine and meloxicam were used perioperatively, with gabapentin for neuropathic pain after discharge once buprenorphine was discontinued. Some new research is taking place into the use of cannabidiol, and its inclusion in multimodal pain relief is promising, although one study with good results was not conducted double blind to remove bias (Brioschi et al, 2020; Mocholi, 2021). Owing to this lack of evidence and prescribing under the cascade, it was not considered an option for this case.
An analgesia not used in this case was locoregional blocks. These work to block transmission of nociception to decrease postoperative pain, and have been found to reduce hospital stays and provide superior pain relief for human patients. However, the success of the block is dependent on the experience, technique and drug doses used; in this case a paravertebral brachial plexus block would have been required to include the scapulectomy site (Hoad, 2014) which is described as utilising a more difficult technique and with more associated complications. The methods for performing a locoregional block include electro-stimulated, ultrasound guided and blind, the latter being the least accurate, and damage from poor technique can include nerve, tissue or blood vessel damage, infection and incorrect dosing (Parkin, 2022).
Pain scoring is a useful tool for hospitalised cases where care will be transferred between clinics and with treatment provided by different members of the team to allow for standardised care, although it can be subject to operator bias (West et al, 2009). Although pain scoring was not used in this case, Albert's recovery proceeded well, and he was ambulatory within 48 hours of surgery. If this had not been the case, then the patient may have benefited from a validated pain scoring system such as a Colorado State University canine and feline acute pain scale (Hoad, 2014) or the Glasgow Composite Measure Pain Scale (Thurston, 2020). Pain scoring for symptoms specific to amputees has been proposed by Boesch et al (2021), although this is yet to be quantified, but remained a viable alternative if post-surgical pain was detected.
Post-surgery, the surgical site is still susceptible to contaminants from the environment or infections, this continues until the body creates a seal at 6–12 hours post-surgery (Smith, 2020). For this reason a non-adherent, perforated polyurethane membrane (Melolin) was applied to the surgical site to absorb any exudate, protect sutures and prevent contamination. Additionally, a medical suit with padding over the surgery site was worn by Albert to prevent trauma from knocking the area while he was unsteady in his ambulation. The kennel was lined with both a padded vet bed and mattress to give further protection to the surgery site, and prevent trauma from recumbent periods.
Post-surgery, several additional therapies could have been used, which were not used in this case, but without any detrimental effect on the patient's welfare.
Cryotherapy in the form of ice packs, wrapped in towels, could be used for 10–20 minute periods throughout the day to reduce pain, inflammation and swelling (Smith, 2020). Later on, physiotherapy could have been used to encourage further vascularisation and vasodilation, circulation and to reduce inflammation (Smith, 2020). This could be done alongside the laser sessions, and while massage techniques were used, and Albert was quickly ambulatory, if he had been less ambulatory this would have been used.
Air transport was then arranged back to the local clinic 4 days post-road traffic accident (Figure 3), with an immediate laser session arranged the same day as arrival, followed by an overnight stay for observations and oral pain relief with gabapentin at a dose of 20 mg/kg three times a day and meloxicam 0.04 ml/kg once daily, Synulox at 16.7 mg/kg twice daily orally, and for monitoring of seroma. The owners were adequately informed and the patient was sent home 5 days post-road traffic accident, 3 days post-surgery, with a medical pet shirt (Figure 4) and meloxicam pain medication, Synulox antibiotics and omeprazole gastroprotectants at the above doses orally.


Laser light therapy
Low-level laser light therapy, or photobiomodulation, involves directing light of specific wavelengths of the infrared or near red electromagnetic spectrum to tissues of the body (Summer, 2021), in order to create a photochemical reaction. Laser classes are ranked according to the potential to damage healthy tissues, with class 1 being the least damaging and class 3b and 4 most commonly used therapeutically (Summer, 2021). The photochemical reaction affects the chromophores in the mitochondria, which are stimulated to increase adenosine triphosphate (ATP) production through aerobic metabolism (Suárez Redondo, 2015). This creates a cellular change to stimulate the production of ATP, increasing cellular oxygenation and speeding up healing times (Summer, 2021). Ultimately, this reduces oedema, has an analgesic effect, causes vasodilation and angiogenesis, fibroblast proliferation and collagen synthesis (Mancinelli, 2016; Summer, 2020; 2021), aides nerve regrowth (Summer, 2020) and has an antimicrobial effect through enhancement of macrophage function and modulation of immune responses, as well as endorphin release (Suárez Redondo, 2015); which are all beneficial in wound healing postoperatively, as well as in cases which may be actively infected (Suárez Redondo, 2015).
The wavelength of the laser determines the targeted chromophores, and the amount of scatter, reflection, transmission or absorption; only the photons absorbed by the cells are utilised in the mitochondria. Depending on the wavelength used, some is absorbed by haemoglobin, melanin and water. Therapeutic wavelengths are between 600–1100 nm (Summer, 2021). Shorter wavelengths are absorbed more superficially, whereas longer wavelengths will have a deeper penetration of tissues (Mancinelli, 2016). For this reason, the manufacturer's instructions on safety and protocol settings must be followed.
The dose range of photobiomodulation is from 1–5 J/cm2 in acute wound cases, and up to 20–30 Jcm2 in chronic cases, this intensity and depth is altered by factors including hair density, skin colour and weight, and is controlled by varying both the power output of the device and using the correct wavelength for the depth and type of tissue targeted. For this to be possible in a clinical setting, where long periods of treatment are not practical, a class IV system is recommended as the output of this class of lasers is over 0.5 W (Suárez Redondo, 2015).
There are contraindications and safety protocols for the use of photobiomodulation therapy; use during pregnancy and with juvenile animals on long bones should be avoided as it may cause premature closing of the growth plates. Neoplasia patients are considered unsuitable as the laser may increase tumour cellular growth (Mancinelli, 2016). Endocrine glands and gonad organs should always be avoided. Metal implants should be avoided because of their potential to heat up under therapy. Patients with photosensitive epilepsy may be unsuitable (Summer, 2021), and the eyes should be protected to prevent retinal damage (Mancinelli, 2016; Summer, 2020). Appropriately filtered goggles for patients, and glasses for operators, should always be worn to avoid damage by photons which have been scattered, reflected or transmitted (Summer, 2020).
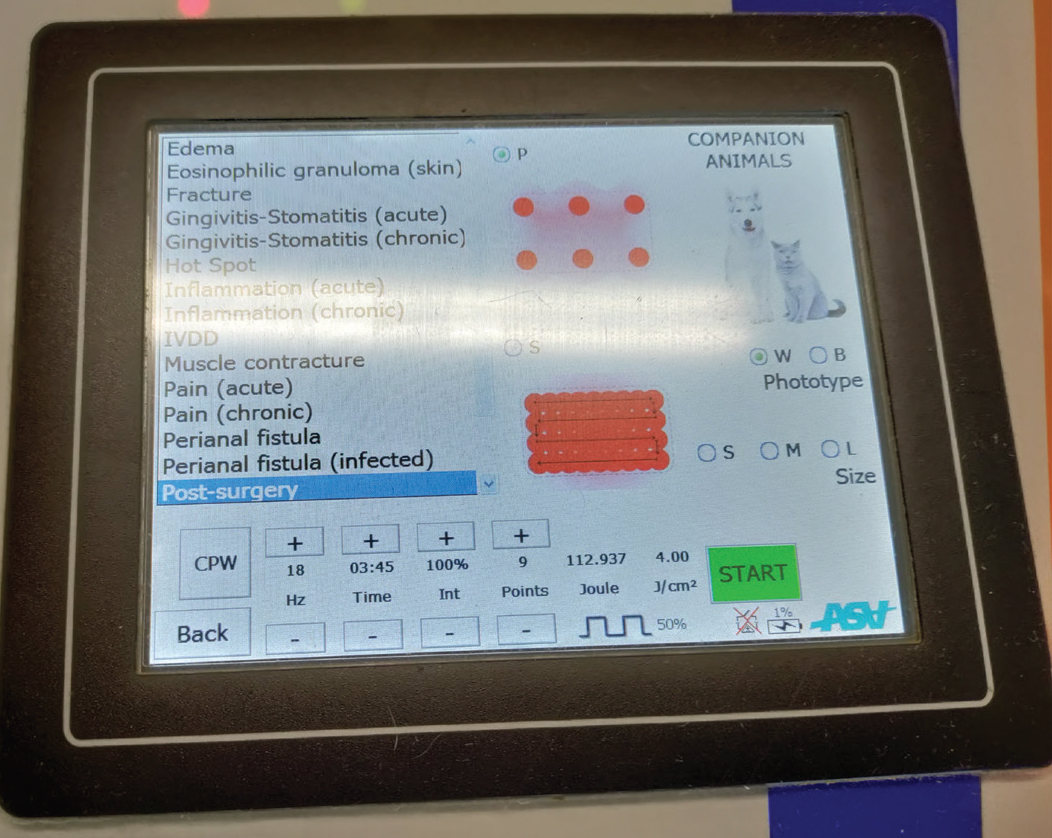
The laser in the clinic is the MLS orange laser. This is a class IV laser using a multiwave system of both nanosecond pulsed 905 nm waves and continuous 808 nm waves to deliver up to 4 cm depth of penetration, and treat both pain and inflammation simultaneously. In this case, point mode was used as the wound area was relatively narrow, and the massaging technique was used with the laser probe. Settings were alternated between post-surgical and oedema settings, to both reduce the seroma present at the time of arrival in the clinic post-surgery and to potentially speed up wound healing.
During laser session 1, at 4 days post-surgery, the post-operative settings, at 9 points and white skin was used on point mode, ventral thorax, cranio-ventral to wound margin, and caudo-dorsal to wound margin (Figures 5–7). This saw an almost immediate reduction of oedema overnight, although as expected, redness and ecchymosis from both surgery as well as resuscitation was clearly evident. This was expected to deepen before it resolved.



During the laser session the patient remained recumbent and showed no reaction to the laser, and was settled and relaxed.
At day 6 post surgery, the second laser session (Figure 8) was completed at the same anatomical locations as session 1, using the oedema setting, as there was a small build-up of fluid present, particularly at the ventral site of the wound. At this stage the ecchymosis previously present had all dissipated, there was no irritation and the wound edges were opposed nicely. Exercise was still very much restricted to toileting access but the patient was ambulatory and managing well.

At day 9 post-surgery, the antibiotic course had completed and the third laser session (Figure 9) was performed using the post-operative settings and 9 points running directly 1 cm cranially and caudally to the suture line to encourage healing speed. At this stage there was very minor oedema at the xiphoid, which was likely the result of the new uneven gait the patient had, and additionally because the patient was so comfortable that he was sleeping on his right side, and needing to swing his body to stand after recumbency. There was minor puckering of the wound edges caudally, and it was agreed the skin sutures would be removed at the next examination. Five-minute lead walks were recommended to encourage muscle mass, although it was warned that he may tire quickly.
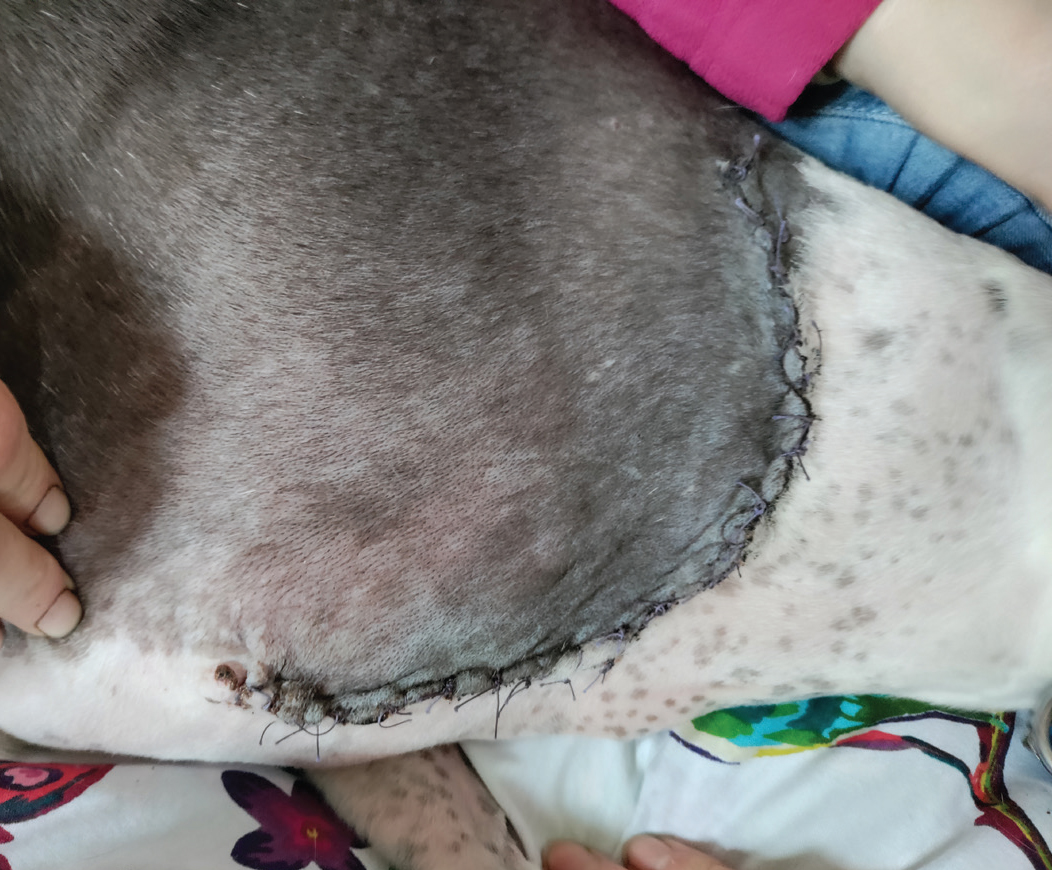
At 13 days post-surgery, the patient was found to have no oedema or inflammation and the PDS skin sutures were removed, walks were going well, and the owners were encouraged to continue to build muscle mass through regular, controlled exercise.
Further examinations were completed at days 21 and 33 post-surgery (Figure 10). There have been no complications, infections or pain behaviours, and return to normal activity levels has been steady.

Conclusions
This case used the MLS laser technology (Figure 11) to support wound healing, reduce oedema and resolve ecchymosis. The author uses the laser for other acute and chronic cases, and looks forward to continuing to support patients with its benefits. This has also been an excellent case to promote registered veterinary nurse empowerment and community nursing. A home assessment has been completed to ensure the environment was safe for the patient's disability, as the portable laser allows the sessions to be done in the patient's home, and the collaboration between the veterinary surgeons and registered veterinary nurses allowed a complex case to be managed efficiently and to a high standard.
- Appropriate team collaboration can facilitate a prompt and accurate diagnosis along with nursing empowerment in clinics where a veterinary surgeon is not present at the time the registered veterinary nurse receives an emergency case.
- Limb salvaging or amputation surgery options should be considered in cases of severe trauma, alongside the owner's capabilities both financially and physically in caring for the patient, as well as providing the correct environmental support and aftercare.
- Timely and appropriate analgesia can prevent phantom limb complex, allodynia and hyperalgesia when amputation may be neccessary.
- Low-level laser light therapy or photobiomodulation can be utilised to potentially improve the outcome of healing post surgery and trauma.
- Team collaboration including supervised transport and community nursing can be used to give excellent outcomes in post surgery cases, including multimodal therapies in owners’ own homes.


