References
Investigating the use of non-contact infrared thermometers in cats and dogs
Abstract
Background:
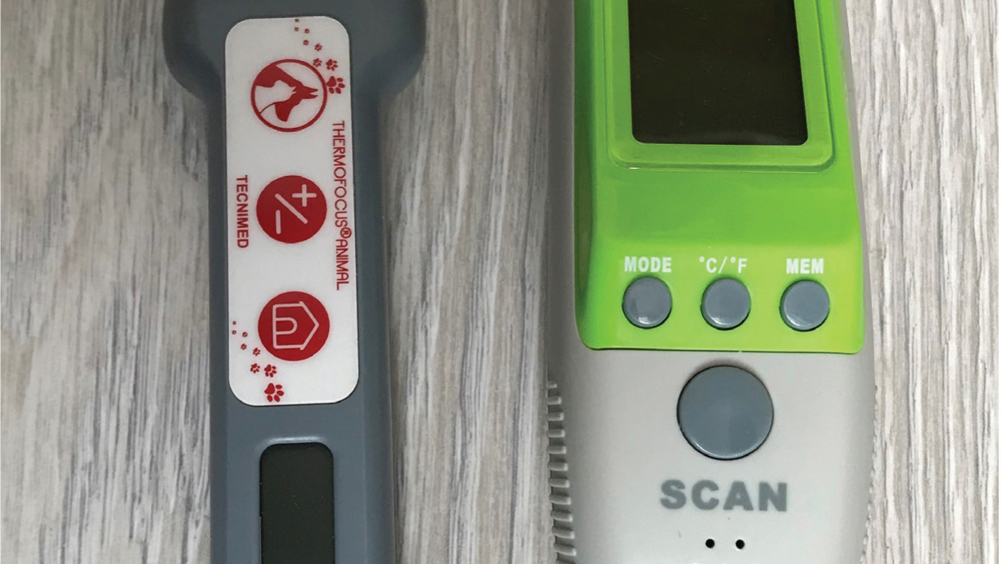
Non-contact infrared thermometers (NCIT) provide a quick, hands off method of monitoring patients' body temperature. There are now animal specific NCIT devices available, however evidence for their use is currently lacking.
Aims:
To evaluate the accuracy of two animal NCIT devices when compared with rectal temperature in anaesthetised cats, and ear temperatures in exercising dogs.
Methods:
27 cats undergoing routine neutering under anaesthetic, and 30 dogs competing in cross country races were recruited to the study. Ocular surface temperature was measured with each of the NCIT devices and compared with rectal temperature (in cats) or ear temperature (in dogs).
Findings:
Less than a third of the readings from both NCIT devices reported temperatures within 0.5°C of rectal temperature (in cats) and ear temperature (in dogs).
Conclusion:
The animal specific NCIT devices do not accurately report body temperature in cats or dogs, so their use in clinical situations cannot be recommended.
Assessment of body temperature forms an essential part of patient evaluation in both veterinary clinics and field situations. Current best practice involves the measurement of rectal temperature (RT) to estimate core body temperature, however this method is not well tolerated in all patients (Lamb and McBrearty, 2013; Gomart et al, 2014; Smith et al, 2015). Repeated RT measurements can result in patient stress, aversion to clinical assessment and require additional patient restraint making nursing care challenging. This has led to increasing interest in alternative, less invasive methods of measuring body temperature including tympanic membrane thermometers, infrared thermography and non-contact infrared thermometers (NCITs).
In theory, NCITs offer a means of measuring body temperature with no risk to the patient (from either physical contact or transmission of infection), together with reduced risk for the operator as it can be performed from a distance and should be less likely to cause a negative response from the animal which could lead to bites or scratches. NCIT measurements can be taken using either thermographic cameras or hand-held thermometers. To date, only human NCITs have been evaluated in cats and dogs (Kreissl and Neiger, 2015; Nutt et al, 2016; Rizzo et al, 2017). In both veterinary studies, the human NCIT devices were found to show poor correlation with RT and failed to reliably detect hypo- or hyperthermia (Kreissl and Neiger 2015; Nutt et al, 2016). Rizzo et al (2017) compared both NCIT and thermography with RT in exercising dogs, finding a correlation between surface temperature measured on both the eye and inner thigh with RT. However no direct comparisons between the NCIT and RT were reported, meaning the reliability of the devices to detect hyperthermia is unknown.
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

