Assessment of body temperature forms an essential part of patient evaluation in both veterinary clinics and field situations. Current best practice involves the measurement of rectal temperature (RT) to estimate core body temperature, however this method is not well tolerated in all patients (Lamb and McBrearty, 2013; Gomart et al, 2014; Smith et al, 2015). Repeated RT measurements can result in patient stress, aversion to clinical assessment and require additional patient restraint making nursing care challenging. This has led to increasing interest in alternative, less invasive methods of measuring body temperature including tympanic membrane thermometers, infrared thermography and non-contact infrared thermometers (NCITs).
In theory, NCITs offer a means of measuring body temperature with no risk to the patient (from either physical contact or transmission of infection), together with reduced risk for the operator as it can be performed from a distance and should be less likely to cause a negative response from the animal which could lead to bites or scratches. NCIT measurements can be taken using either thermographic cameras or hand-held thermometers. To date, only human NCITs have been evaluated in cats and dogs (Kreissl and Neiger, 2015; Nutt et al, 2016; Rizzo et al, 2017). In both veterinary studies, the human NCIT devices were found to show poor correlation with RT and failed to reliably detect hypo- or hyperthermia (Kreissl and Neiger 2015; Nutt et al, 2016). Rizzo et al (2017) compared both NCIT and thermography with RT in exercising dogs, finding a correlation between surface temperature measured on both the eye and inner thigh with RT. However no direct comparisons between the NCIT and RT were reported, meaning the reliability of the devices to detect hyperthermia is unknown.
Two animal specific NCITs are now available for both veterinary and pet owner use (Figure 1). The aim of this research study was to evaluate the use of two animal specific NCITs in both cats and dogs, across a range of body temperatures.

Methods
The research study was approved by the Nottingham Trent University's School of Animal, Rural and Environmental Science's ethics approval group.
The project comprised two separate studies measuring body temperature in cats and in dogs. Healthy, anaesthetised cats were used to evaluate a range of normal and hypothermic temperatures. Exercising dogs were used to assess normal and hyperthermic temperatures.
Recruitment of cats and assessment of body temperature
Cats were opportunistically recruited from those under-going routine neutering at two first opinion veterinary practices between December 2016 and June 2017. Owners gave written informed consent for inclusion in the study. Each cat was assessed as clinically normal by the treating veterinary surgeon. 27 cats were recruited, ten males and 17 females, three British short hair and 24 domestic short hair, ranging in ages from 3 months to 4 years.
Specific anaesthetic protocols were determined by the veterinary surgeon responsible for each case and were not standardised for this study. RT was monitored throughout the surgical procedures as part of routine anaesthetic monitoring by veterinary nurses (VNs) who volunteered to assist with data collection. RT was measured using a V966F Vicks Comfortflex Digital Thermometer (KAZ Incorporated, New York, USA), which alarms once a stable peak temperature is reached. The Comfortflex Digital Thermometer measures temperatures between 32.0–42.9°C with an accuracy of ±0.2°C at room temperature. The normal feline temperature range established by Levy et al (2015) of 36.7–38.9°C was used to interpret RT readings.
Recruitment of dogs and assessment of body temperature
Dogs were recruited opportunistically at canicross (canine cross country) races taking place in the Midlands, UK, between December 2016 and April 2017. On consenting to their dogs' participation in the study, owners were required to confirm that their dogs were fit and healthy and not undergoing veterinary treatment. 30 dogs, 18 males and 12 females, were recruited, representing 13 breed types, including seven crossbreeds, four Labrador Retrievers, four Cocker Spaniels and three Springer Spaniels. Ages ranged from 6 months to 12 years.
Body temperature was measured using ear thermometers, as they are quicker and better tolerated by the dogs in field conditions than rectal thermometers (Hall and Carter, 2017a; Carter and Hall, 2018). Tympanic membrane temperature (TMT) was recorded using a Vet-Temp VT-150 Instant Ear Thermometer (Advanced Monitors Corporation, San Diego, CA, USA), covered by a single use VetTemp DPC 500 probe cover (Advanced Monitors Corporation). The Vet-Temp thermometer measures temperatures between 32.2–43.3°C, with an accuracy of ±0.2°C. The thermometer was used as per the manufacturer's instructions, with no lubrication and a reading being obtained following the audible alarm. If a reading reported an error code, the probe cover was changed, and the process repeated. TMT was measured at rest before the race where possible (some dogs were too excitable pre-race to examine), then immediately after crossing the finish line. When required, dogs were lightly restrained by their owner or an assistant. Left or right ear was selected at random depending on the positioning of the dog following restraint. The normal TMT temperature range established by Hall and Carter (2017b) of 36.8–38.8°C was used to interpret TMT readings. One investigator (EH) recorded all TMT readings to ensure consistency.
NCIT measurement site selection
Both animal NCIT thermometers state they can be used on a variety of anatomical locations. However, variability in coat colour, type and length can impact infrared detection of surface temperature measurements in dogs and cats if haired locations are used for measurement. Measuring corneal surface temperature minimises variability and has been reported to correlate well with RT (Rizzo et al, 2017).
Measuring eye temperature using NCITs
Eye temperature (ET) was measured using two animal specific NCIT devices, the Thermofocus Animal non-contact thermometer (Technimed, Vedano, Italy), and the Rycom non-contact infrared thermometer for pets model RC004T (Guangzhou Jinxinbao Electronic Co. Ltd, Guangzhou, China). The Thermofocus thermometer uses LED light guides to indicate the ideal distance for temperature measurement (Figure 2), the Rycom thermometer should be held between 2–5 cm away from the surface being measured (Figure 3). A ‘lo’ reading is given when the NCIT devices records a temperature below 32.0°C. In the event of a ‘lo’ reading, the measurement was repeated, if the subsequent reading was also ‘lo’, this was recorded as a missing data point due to ‘lo’ reading. Both devices require calibrating for 30 minutes following any changes in ambient temperature. For the feline study, the thermometers were stored in theatre to ensure no sudden changes in conditions. For the canine study the thermometers were taken out of the car 30 minutes prior to any temperature readings to allow calibration. For both studies ET was measured once, on the eye most readily accessible to the operator.


ET was measured in the cats following induction of anaesthesia once the patient was stable, and at the end of the procedure prior to recovery immediately after RT was measured. The cat's ET was measured by the VN monitoring the anaesthetic, following training in the use of both devices. Left or right eye was determined by the patient's position for the surgical procedure.
ET was measured in the dogs immediately after TMT was recorded by the same investigator. The Rycom thermometer was used first, as this does not emit any light sources so was believed to be less likely to cause aversion. Left eye was primarily used for ET measurement as the investigator is right handed, but this depended on the positioning of the dog following light restraint by the owner. If the dog did not tolerate the NCIT device (resisted light restraint or held the eye closed (demonstrated with a cat in Figure 4) this was recorded as a missing data point due to intolerance.

Data analysis
Sample size was estimated using previously published average temperatures to detect a 0.6°C difference between the NCIT temperature and the comparator (Kreissl and Neiger, 2015; Levy et al, 2015). At least 26 animals were needed to achieve a study power of 95%, with 0.05% confidence. As multiple readings from the same animal were taken under different conditions, induction versus recovery from anaesthesia for cats, and pre and post-race under a variety of environmental conditions, each replicate was treated as an individual data point for analysis.
Statistics were calculated using SPSS 24.0 (SPSS Inc., Chicago, IL, USA). Data were tested for normality using the Shapiro-Wilk test. As data were not normally distributed, a Spearman's rho correlation was used to assess correlation between TMT and ET measured by each device in dogs. In cats, a Spearman's rho correlation was used to assess correlation between RT and ET measured by each device.
As correlation does not necessarily reflect clinical accuracy, the agreement between each thermometer was also examined. The NCIT reading was subtracted from the comparator, in line with previous studies an acceptable limit of difference between the two thermometers was set at ±0.5°C. A scatter plot of RT or TMT against the difference in RT/TMT versus ET readings was used to provide a visual assessment of the difference between the two sites. Significance was indicated at p<0.05 for all tests.
Results
Cats
A total of 54 paired measurements were recorded for cats, two paired measurements per cat. RT readings ranged from 36.1 to 39.2°C (median=37.6°C). ET measured with the Thermofocus NCIT ranged from 31.0 to 38.8°C (median=36.4°C). ET measured with the Rycom NCIT ranged from 32.1 to 38.2°C (median=35.5°C) with one reading reported as ‘lo’. The difference between RT and ET ranged from -1.2 to 7.0°C (median=1.4°C) for the Thermofocus device, and -1.0 to 5.8°C (median=1.3°C) for the Rycom device.
Eight cats were hypothermic as measured by RT, with one hyperthermic reading, the NCIT devices’ sensitivity and specificity results for detecting hypothermia are displayed in Table 1. Both NCIT devices reported a hypothermic temperature for the one cat with a hyperthermic RT.
| Test sensitivity | Test specificity | Positive predictive value | Negative predictive value | |
|---|---|---|---|---|
| Thermofocus detecting hypothermia in cats | 50% | 47.8% | 14.3% | 84.6% |
| Rycom detecting hypothermia in cats | 62.5% | 32.6% | 13.9% | 83.3% |
| Thermofocus detecting hyperthermia in dogs | 42.9% | 87.5% | 75% | 63.7% |
| Rycom detecting hyperthermia in dogs | 3.2% | 100% | 100% | 58.3% |
NCIT, non-contact infrared thermometer
When measured with the Thermofocus NCIT, 27.8% of ET readings measured within 0.5°C of RT (Figure 5). The Rycom NCIT measured 13.2% of ET readings within 0.5°C of RT, visually demonstrated
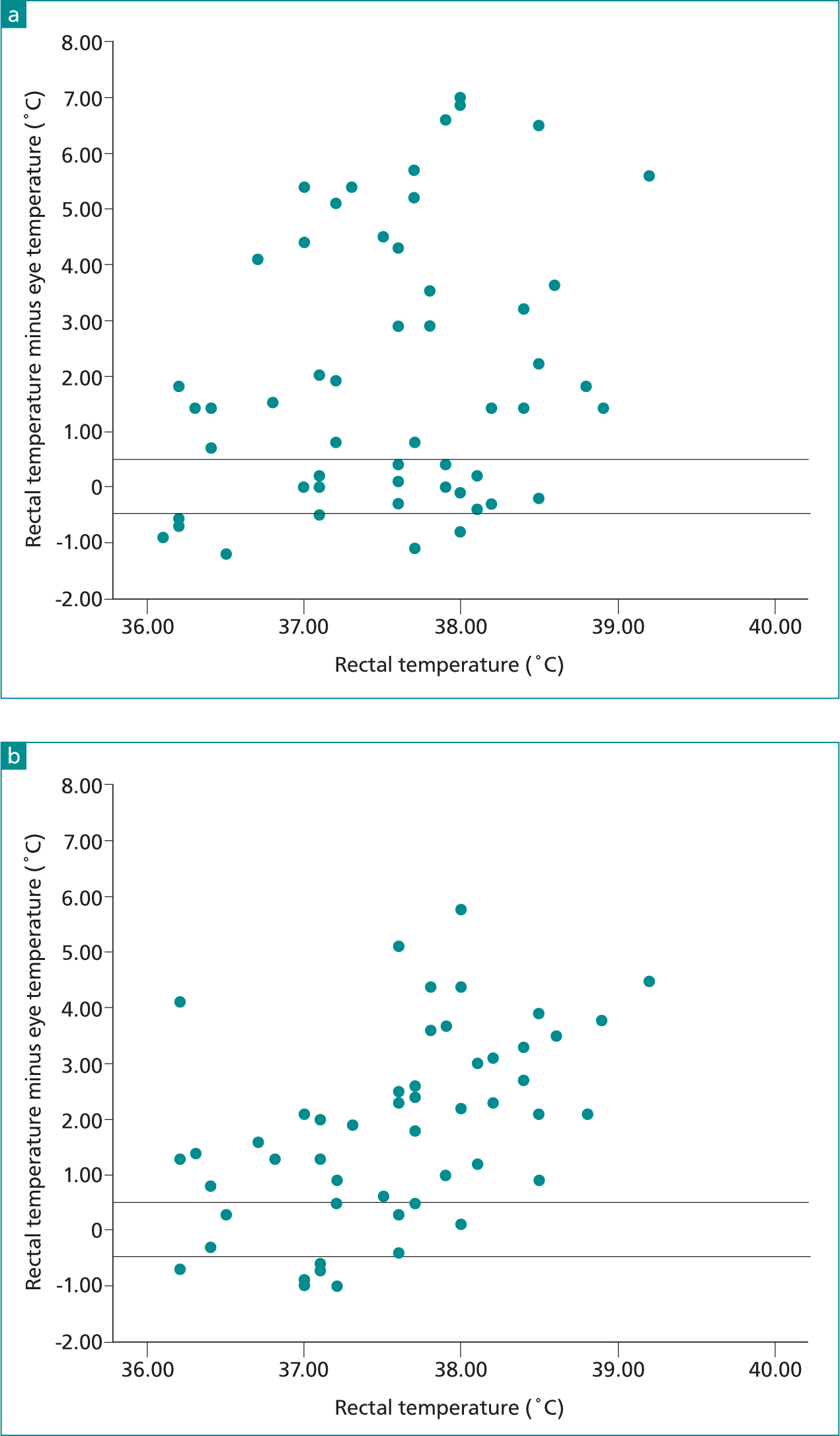
No correlation was found between RT and ET measured by the Thermofocus NCIT (Rs=0.149, p=0.283), or RT and ET measured by the Rycom NCIT (Rs=-0.145, p=0.301) (Figure 5).
Dogs
A total of 78 paired temperature readings were taken for dogs, ranging from one to eight paired measurements per dog (median=2). TMT readings ranged from 36.3 to 42.2°C (median=38.6°C). The Thermofocus device measured ETs ranging from 34.0 to 41.6°C (median=38.1°C), returned one ‘lo’ reading and was not tolerated on two occasions, resulting in 75 paired readings. The Rycom device measured ETs ranging from 32.1 to 39.1°C (median=37.4 °C), returned one ‘lo’ reading and was not tolerated on four occasions, resulting in 73 paired readings. The difference between the TMT and ET ranged from -2.7 to 5.5°C (median = 0.7°C) for the Thermofocus device, and -1.1 to 7.2°C (median=1.5°C) for the Rycom device.
36 dogs were hyperthermic as measured by TMT, the NCIT devices' sensitivity and specificity results for detecting hyperthermia are displayed in Table 1. The Thermofocus device identified 15/35 dogs with hyperthermia, the Rycom device identified 1/31 dogs with hyperthermia. Both devices reported a ‘lo’ (<32.0°C) temperature for at least one hyperthermic dog.
When measured with the Thermofocus NCIT, 30.7% of ET readings measured within 0.5°C of RT. The Rycom NCIT measured 27.4% of ET readings within 0.5°C of RT (Figure 6).
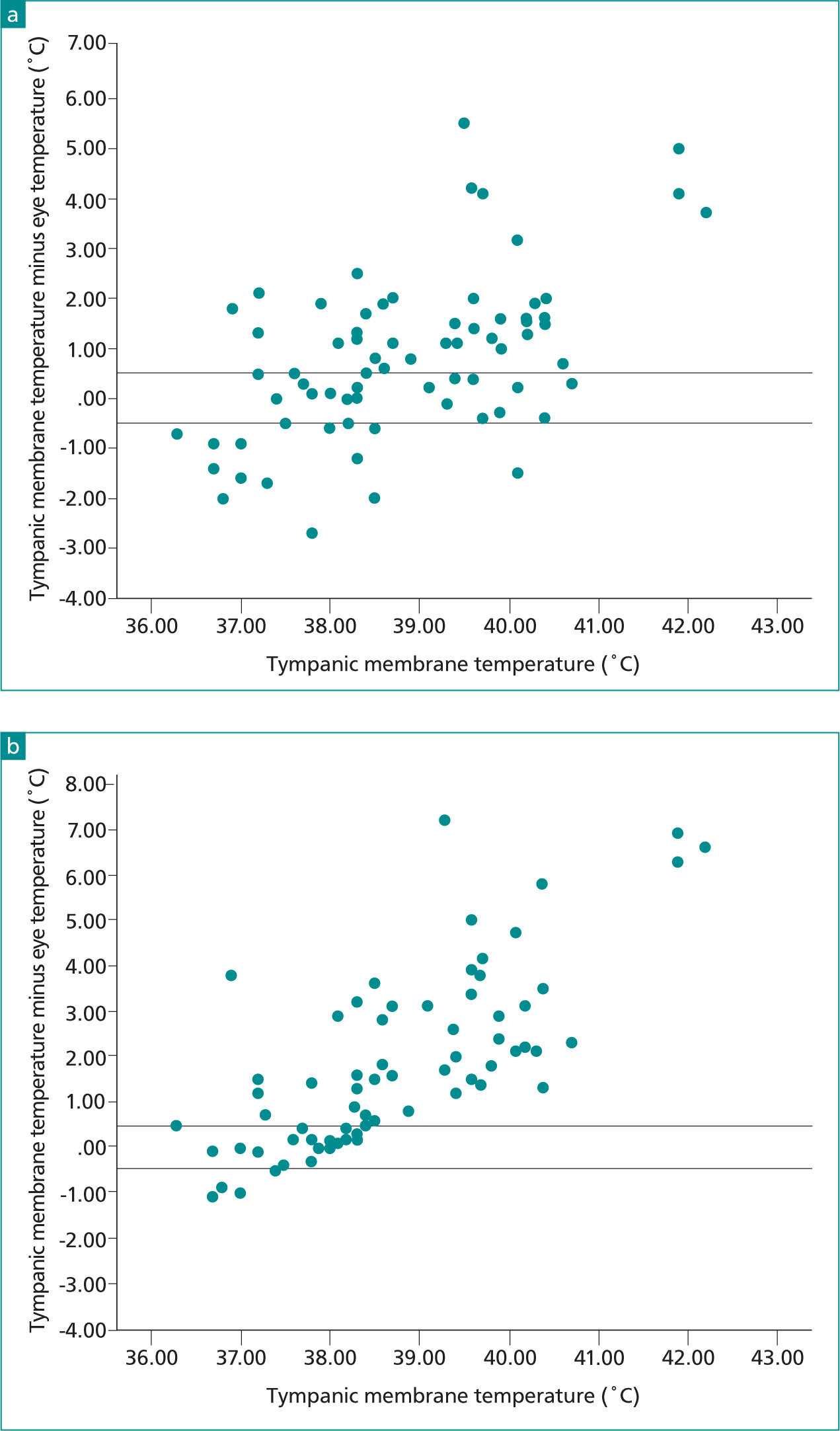
There was a weak positive correlation between TMT and ET measured with the Thermofocus NCIT (Rs=0.391, p=0.001), no correlation was found between TMT and ET measured with the Rycom NCIT (Rs=-0.013, p=0.913).
Discussion
In line with previous studies evaluating human NCIT devices in cats and dogs, this study found poor agreement between the animal NCIT devices and body temperature measured with rectal and ear thermometers.
Within the wider veterinary literature, the clinically acceptable temperature difference between thermometers is commonly stated to be ±0.5°C (Greer et al, 2007; Lamb and McBrearty, 2013; Smith et al, 2015; Watson et al, 2015). While some have argued even a ±0.5°C difference could negatively influence clinical decision making, many veterinary thermometers have an inherent accuracy of ±0.2°C and different operators and techniques for measuring RT have been shown to differ by up to 0.5°C in the same animal (Naylor et al, 2012). In this study, less than a third of all readings measured with the NCIT devices were within ±0.5°C of the RT or TMT measurements, which renders the devices unsuitable for clinical use.
If there is a consistent difference between temperature measuring devices, or anatomical locations this can be accommodated with specific temperature reference ranges. Several studies have found TMT to read 0.4–0.6°C below RT in dogs (Gomart et al, 2014; Zanghi, 2016; Hall and Carter, 2017a), therefore a TMT specific canine temperature range has been established (Hall and Carter, 2017b). Figures 5 and 6 show there is no consistent difference between ET and RT or TMT in cats or dogs. The figures demonstrate that as body temperature decreases ET increasingly over-estimates body temperature, meaning hypothermia can go undetected. Likewise, as body temperature increases, ET increasingly underestimates body temperature leaving hyperthermia undetected.
As the feline ET measurements were performed under anaesthesia, their altered eye position and physiology may have affected the temperature readings. As eye position alters with depth of anaesthesia, varying degrees of corneal covering from the third eyelid could have contributed to the variation in temperatures. Corneal surface temperature also decreases following opening of the eyelids after blinking (Tan et al, 2009), as the anaesthetised cats would not have been blinking this could have further contributed to the poor agreement between RT and ET.
It must also be noted that a key benefit of non-contact thermometry should be improved patient tolerance and yet dogs did not tolerate either device on multiple occasions. As demonstrated in Figure 4, some animals simply refused to open their eyes when the thermometer approached.
Limitations
A major limitation of this study is the use of two different anatomical sites for reference temperature measurement. Ideally, the NCIT devices would have been compared with RT, or a measure of core body temperature (such as oesophageal temperature) in both species. As the feline patients were anaesthetised during temperature monitoring, there were no ethical concerns about repeated RT measurements being performed. To ensure a range of body temperatures including hyperthermia were included in the study, exercising healthy dogs were recruited rather than veterinary patients. ET measurements were taken opportunistically during another project measuring body temperature in racing dogs using TMT. As the dogs were accustomed to having their ear temperatures monitored, it was felt introducing both the NCIT devices and rectal thermometers could negatively impact the dogs, so TMT was used to determine body temperature.
Another limitation is that the feline temperature measurements were performed by five different individuals. While all temperatures were taken by experienced veterinary staff following training with the NCIT devices, this has the potential to introduce operator variation. This does however, reflect the more normal clinical setting with multiple veterinary team members providing patient care, and clinicians basing decisions on parameters measured by several different people.
Conclusion
An ideal thermometer is quick, well tolerated by the patient and accurate. While the non-contact thermometers provide a temperature reading in seconds, they were not always tolerated by dogs and cannot be considered accurate enough for clinical use in either dogs or cats. Eye temperature measured with animal specific NCITs underestimated body temperature in both normothermic cats and hyperthermic dogs. There was poor agreement between both ET and RT in cats, and between TMT and ET in dogs, meaning both hypothermia and hyperthermia could go undetected in clinical patients. Further studies using the non-contact thermometers following calibration against core temperature could be carried out to determine if this improves accuracy.


