In cats, loss of muscle mass may result from ageing (sarcopenia) or from multiple chronic conditions, including chronic kidney disease, hyperthyroidism, congestive heart failure, and cancer (Baez et al, 2007; Freeman, 2012; Santarossa et al, 2017; Santiago et al, 2020). In some cases, subtle atrophy of skeletal muscle may be one of the only physical examination manifestations of the early stages of these diseases. In addition, progressive loss of muscle mass secondary to disease, termed cachexia, may be associated with a worse prognosis (Finn et al, 2010; Freeman, 2012; Miyamoto et al, 2016; Santarossa et al, 2017; Santiago et al, 2020). However, muscle wasting in cats can be easily missed if muscle condition is not specifically evaluated. Chronic disease, and subsequent chronic inflammation, create states within the body in which muscle breakdown occurs, while fat mass may increase or remain stable (Freeman, 2012; Santarossa et al, 2017). As such, weight and overall body condition may be unchanged or even increasing, while ongoing loss of muscle tissue is occurring secondary to disease. While sarcopenic muscle loss occurs with age in the absence of disease, assuming that cats with muscle wasting are ‘just getting old’ risks missing the diagnosis of manageable chronic diseases and losing the chance to increase both quantity and quality of life for feline patients.
Unfortunately, no easy, inexpensive measurement technique yet exists that can quantify a veterinary patient's muscle mass and identify early loss, although multiple modalities are currently being evaluated for this purpose (Zanghi et al, 2013a; Freeman et al, 2018, 2019; Rayhel et al, 2020; Santarossa et al, 2017). For the time being, muscle atrophy remains a physical examination diagnosis, and an often overlooked one. Evaluation and recognition of muscle atrophy may allow for identification and management of chronic feline conditions before significant debilitation occurs. Veterinary nurses are the first line in identifying muscle atrophy, obtaining thorough diet and nutritional histories to identify areas where intervention may be possible, and communicating to clients the importance of diagnostic testing to investigate the cause of muscle atrophy before disease progression occurs.
Pathophysiology of muscle atrophy in disease
Muscle tissue is constantly undergoing both protein synthesis and protein breakdown, in both health and disease states. The balance between synthesis and breakdown processes determines whether ‘hypertrophy’ (muscle growth) or ‘atrophy’ (reduction in muscle mass) occurs overall (Schiaffino et al, 2013). Disease states shift this balance toward atrophy by downregulating protein synthesis pathways and upregulating protein breakdown and degradation pathways. In general, growth of muscle occurs via activation of the mammalian target of rapamycin complex 1 (mTORC1) cellular pathway, while degradation occurs via the ubiquitin-proteasome (UPP) and autophagy-lysosome (ALP) pathways. Briefly, inflammatory cytokines like interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and others, as well as disease- and stress-associated hormones like angiotensin II, myostatin, and cortisol, are upregulated in disease states like chronic kidney disease and cancer (Zhang et al, 2009, 2011, 2019; Miyamoto et al, 2016; Guijarro and Egido, 2001). These molecules then act at the cellular level to decrease mTORC1 signalling and increase the activities of the UPP and ALP (Zhang et al, 2009, 2011; Schiaffino et al, 2013; Miyamoto et al, 2016; Zhang et al, 2019). This in turn causes the rate of muscle protein degradation to outpace synthesis, leading to muscle atrophy. In addition, these same molecular pathways can lead to dysfunction or breakdown of mitochondria, leading to a loss of energy source for the muscle cells (Schiaffino et al, 2013; Zhang et al, 2019).
Methods to assess muscle condition in cats
Although methodologies including muscle ultrasound, computed tomography (CT) scan, magnetic resonance imaging (MRI), radiography, and others are actively being researched, there is currently no validated, quantitative assessment tool for determining or estimating overall muscle mass in feline patients (Stanton et al, 1992; Borges et al, 2012; Zanghi et al, 2013b; Santarossa et al, 2017; Freeman et al, 2018; Rayhel et al, 2019). Hopefully, one or more of these measurement tools will emerge as a reliable, inexpensive, and noninvasive measure of feline muscle condition. Until then, subjective assessment methods like tracking bodyweight, body condition scoring, and muscle condition scoring should be used for every patient, at every visit. Note that ‘body condition score’ generally refers to a cat's fat mass, while ‘muscle condition score’ refers specifically to the cat's estimated amount of skeletal muscle on physical examination. If hydration status, free fluid content, and fat mass are relatively constant, careful tracking of bodyweight through time can help identify muscle loss at its start. However, it is important to keep in mind that if fat mass increases or decreases, growth of an existing tumour occurs, or free fluid accumulates due to underlying disease, changes in bodyweight no longer reflect changes in patient muscle mass. To help determine whether muscle loss is occurring despite a static bodyweight, body condition and muscle condition should be assessed separately and noted in the patient record so that downward trends can be identified as early as possible.
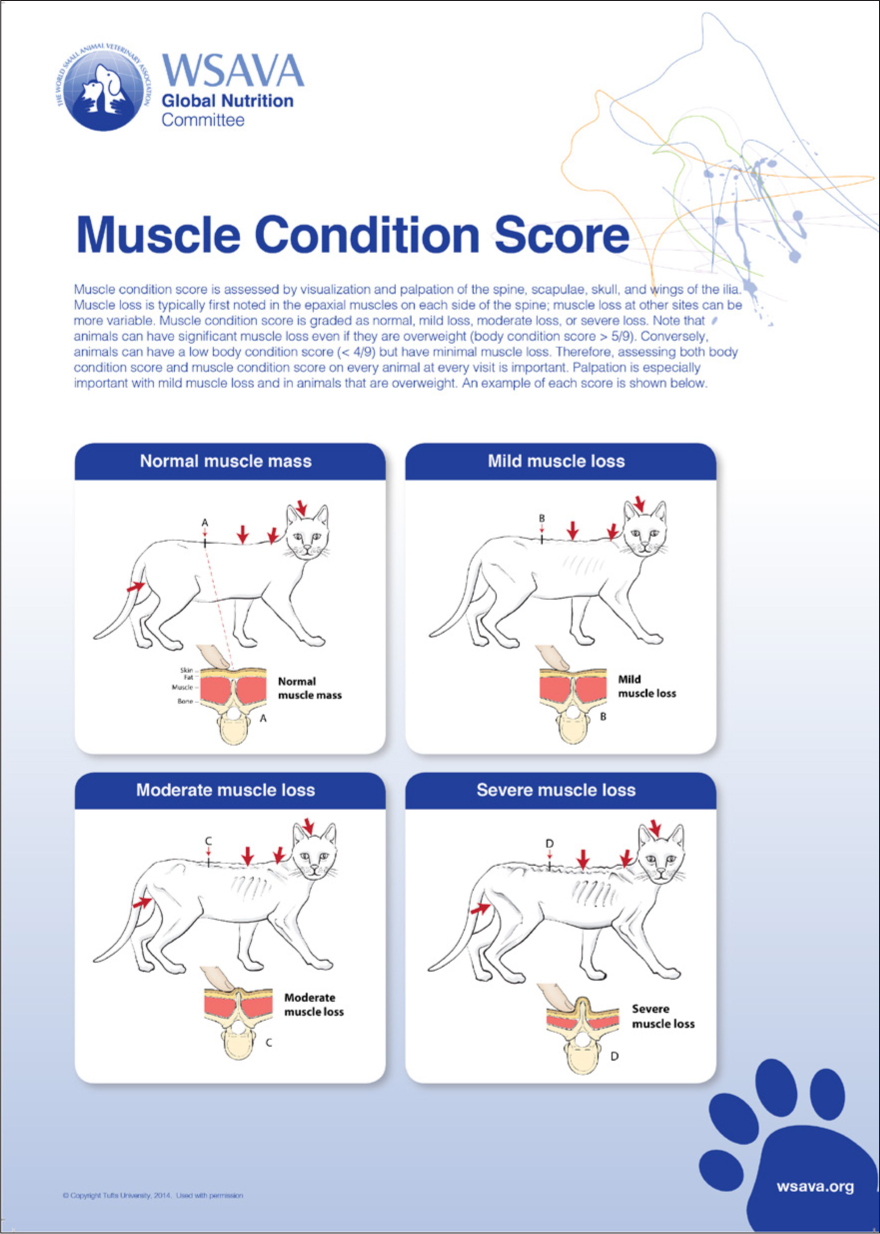
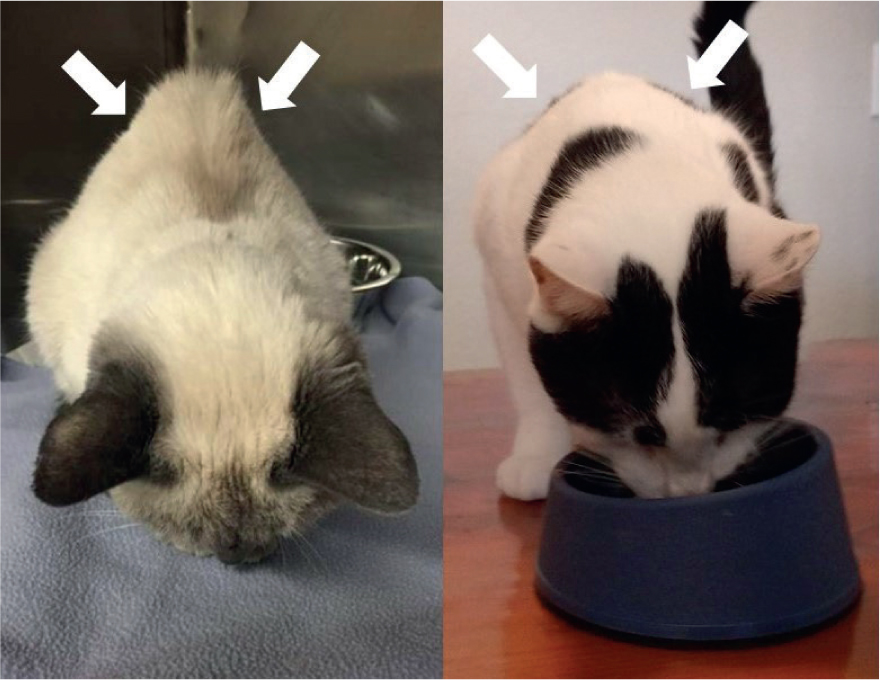
The World Small Animal Veterinary Association (WSA-VA) has published nutritional assessment guidelines which detail how to assess body condition and muscle condition in cats (Freeman et al, 2011), including instructional videos (https://wsava.org/global-guidelines/global-nutrition-guidelines/). The muscle condition score (Figures 1 and 2) is performed using visual assessment and palpation, and although subjective, is a valuable part of patient assessment (Freeman, 2012). Briefly, the temporal, scapular, epaxial, and lumbosacral muscles are palpated and their size subjectively assessed to give an overall assessment of no, mild, moderate, or severe generalised muscle atrophy. As the muscle condition score is subjective, holding training and practice sessions for all members of the veterinary care team may aid in developing consistency among team members. Additionally, posting visual aids depicting different body and muscle condition scores in clinic treatment areas may also help maintain consistency. In combination, trends in patient body-weight, body condition, and muscle condition may provide clues that early muscle loss is occurring, prompting further investigation into the underlying cause.
Diagnostic investigation and therapeutic interventions for muscle loss
If muscle loss is suspected based on downward trends in bodyweight and subjective muscle condition score, a thorough medical and nutritional history should be obtained from the owner as a first diagnostic step (Table 1), followed by a complete physical examination (Table 2). The owner should be questioned about changes in appetite, attitude, energy level, frequency of vomiting, faecal quality or frequency of bowel movements, water intake and urination amount/frequency, and respiration rate and effort. Depending on the underlying cause of the muscle atrophy, appetite may be decreased, unaffected, or increased. If the owner can precisely quantify the amount, brand, and flavour of food the cat eats voluntarily, the cat's caloric intake can be calculated. This value can be compared with the cat's estimated resting energy requirement (RER), which can be calculated as follows:RER=70 x (bodyweight in kg)0.75
Table 1. History questions for owners of cats with noted muscle atrophy
| Nutritional |
|---|
| Brand, flavour, and amount of food (in oz or g) eaten voluntarily in one dayType and amount of treats eaten voluntarily in one dayHistory of being ‘picky’ or requiring frequent diet changesWilling to eat human foods but aversive to commercial cat foodsCurrent medications being administered (dose and frequency) |
| Clinical |
| Changes in attitude, behaviour, or energy levelVomiting (including frequent ‘hairballs’)Diarrhoea or soft stool; changes to faecal consistency or colourIncreased drinking, urination volume, or urination frequencyExercise intoleranceIncreased resting respiratory rate (> 40 breaths per minute) or effortCoughing |
| Environmental |
| Number of cats in householdMeal feedings, or fed ad libitumAre cats separated for feedings? Fed together? Supervised?Ease of access to food? Location of food bowls relative to other household cats? |
Table 2. Physical examination findings to note for cats with muscle atrophy
| General |
|---|
| Bodyweight and body condition scoreMuscle atrophy (none, mild, moderate, or severe)Temperature, pulse, respiration rateAttitude (bright, quiet, dull, stuporous, obtunded, comatose)Hydration status, mucous membrane colour and capillary refill timeHair coat quality and grooming status |
| Facial, oral, cervical |
| Ocular or nasal dischargeOral ulcers or halitosisTachypnea or increased respiratory effortThyroid slip |
| Thoracic auscultation |
| Tachycardia, arrhythmia, or heart murmurMuffled heart or lung soundsCrackles or wheezes on auscultation |
| Abdominal palpation and rectal examination |
| Abdominal pain or discomfort? Vocalisation on palpation?Abdominal distention or fluid waveSize and shape of kidneys and bladderThickened intestinal loops or palpable massesFaecal or diarrhoea staining around rectumQuality of faeces on rectal thermometer |
Intact cats, cats with particularly active lifestyles, or cats in high-energy life stages (i.e. lactation, growth), may require caloric intake in excess of RER to maintain weight and muscle mass (Freeman et al, 2011). Thus, RER can be adjusted to a maintenance energy requirement (MER), considering age, life stage, activity level, comorbid conditions, and neuter status (Bermingham et al, 2010). However, the authors feel that for an adult, neutered cat with an average (low) home activity level, RER may be an appropriate initial goal for caloric intake. If, however, weight/muscle loss continues despite caloric intake that meets RER, the patient's daily caloric goal must be increased accordingly.
Muscle loss despite caloric intake that exceeds RER should increase suspicion for metabolic diseases, such as hyperthyroidism, exocrine pancreatic insufficiency (EPI), or diabetes mellitus. If appetite is decreased and caloric intake is less than RER, chronic kidney disease, chronic enteropathy, heart or liver disease, or cancer should be suspected. These differentials can be further prioritised with the help of minimum database laboratory work, including a complete blood count, chemistry panel, T4, and urinalysis. A definitive diagnosis of the underlying disease may be made on the basis of the minimum database; if not, additional diagnostics such as serum cobalamin and trypsin-like immunoreactivity (TLI) levels, thoracic radiographs, and/or abdominal ultrasound may help identify chronic enteropathy, cardiac disease, EPI, or cancer. A flowchart depicting a possible diagnostic approach to noted muscle atrophy is provided in Figure 3.
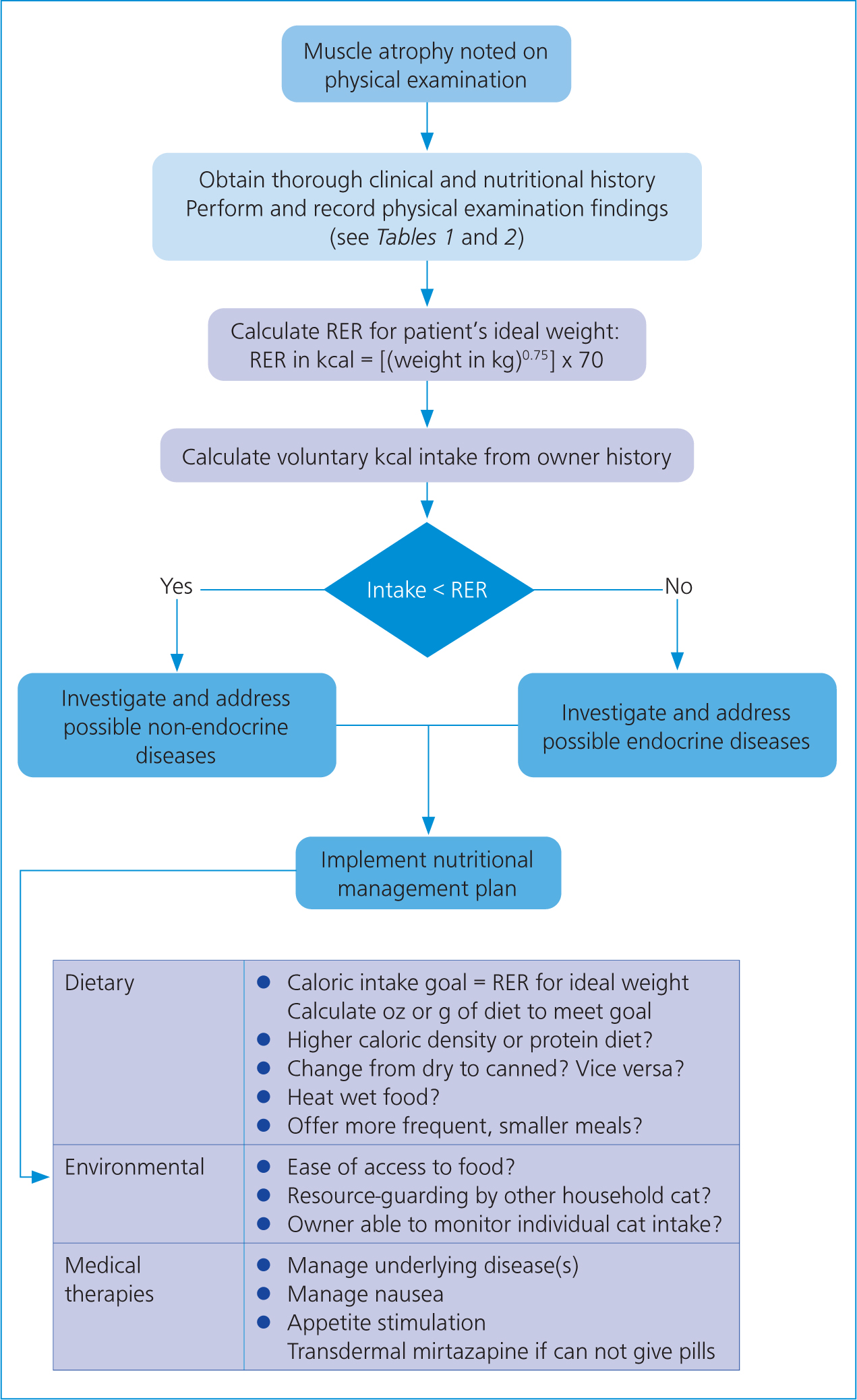
If a definitive underlying disease is identified via these diagnostics, treatment or management of the underlying cause is the best way to prevent progression of muscle atrophy and debilitation. No targeted medical interventions currently exist to prevent muscle atrophy regardless of underlying cause in veterinary patients. Unfortunately, if the underlying cause cannot be addressed, intervention to prevent further muscle atrophy is usually unsuccessful. However, even if disease management is initiated, it is essential to provide owners with a nutritional management strategy to ensure appropriate caloric and protein intake can occur. Owners should be educated on ways to quantify nutritional intake and should be given a specific daily food intake goal for their cat based on a calculation of RER for their estimated ideal bodyweight. Ideally, the owner can purchase a kitchen scale so that the goal number of grams or ounces of the cat's usual or recommended diet can be offered. Any food that the cat does not eat can then be weighed and recorded. If this cannot occur, an estimated fraction of cups of food per day can be provided to the owner.
Unless comorbid conditions exist which might benefit from protein content modification (i.e. hepatic encephalopathy, International Renal Interest Society (IRIS) III-IV chronic kidney disease, protein-losing nephropathy), higher-protein diets should be considered to help increase stimulus for muscle cell pathways which increase muscle protein synthesis. Unfortunately, evidence-based cutoffs for overall protein content and specific amino acid content of diets in patients with muscle wasting do not currently exist, particularly with regard to specific underlying conditions. One study comparing high, moderate, and low protein diets in adult, apparently healthy cats found that to maintain muscle mass, a daily protein intake greater than 5.2 g/kg bodyweight was required (Laflamme and Hannah, 2013). The high-protein diet which achieved this contained 9.5 g protein/100 kcal. For comparison, the Association of American Feed Control Officials (AAFCO) minimum requirement for dietary protein content in adult cats is 6.5 g/100 kcal; typical ‘renal diets’, considered protein-restricted, contain 5.8–7.1 g/100 kcal. Similar studies evaluating protein cutoffs for muscle maintenance in specific conditions (chronic kidney disease, heart disease, cancer, etc.) are warranted to better guide dietary protein requirements for cats at risk for cachexia. In addition, supplementation of the diet with omega-3 fatty acids (40 mg/kg eicosapentaenoic acid (EPA) and 25 mg/kg docosahexaenoic acid (DHA) per day) can also be considered to reduce inflammatory stimulus for muscle breakdown (Freeman, 2010).
Once a nutrition plan has been implemented, the cat should be weighed every 1–2 weeks until weight and muscle condition stabilise. If weight loss progresses or the cat consistently eats less than the desired amount of food, intervention to increase food intake should be implemented. Environmental enrichment, appetite stimulation (mirtazapine, cyproheptadine) and nausea control (maropitant citrate, ondansetron) should be considered to help increase voluntary food intake. In multi-cat households, feeding the affected cat separately or purchasing an ID chip feeder may help sick cats access food, and may also aid in encouraging and allowing owner recording of food intake. Feeding more frequent, small meals, heating wet food in the microwave, or offering a different diet or mix of diets may also help increase caloric intake. If environmental and medical management fail to allow the cat to meet its intake goals, enteral feeding tubes should then be considered.
Conclusion
Muscle loss is associated with multiple chronic diseases in feline patients and may be an early indicator that diagnostic testing beyond a physical examination should occur. Subtle decreases in muscle mass may be missed on physical examination; as such, bodyweight, body condition, and muscle condition should be separately evaluated in every patient at every veterinary visit. If muscle loss is suspected, diagnostic investigation including a thorough medical and nutritional history and minimum database (including T4 and urinalysis) should be recommended. Any identified underlying condition should be appropriately managed, and a detailed nutritional plan should be provided to the owner. Environmental and pharmacologic interventions should be implemented if the patient fails to meet caloric intake goals. If these interventions are also unsuccessful, enteral feeding tubes should be considered. Veterinary nurses are integral in obtaining nutritional and clinical histories that increase the likelihood that muscle atrophy will be recognised and investigated. They often obtain and record vital parameters, including patient weight, that provide valuable information on trends in patient body composition. They also have a large role in communicating the importance of a thorough diagnostic plan to evaluate for underlying diseases causing muscle wasting, and in communicating clear and concise nutritional management plans to owners. As such, veterinary nurses are the first and last line in assessing muscle condition and managing associated diseases appropriately.
KEY POINTS
- Subtle muscle loss can be an early indicator of serious, but manageable, chronic diseases.
- Muscle condition, bodyweight, and body condition should be assessed and noted in the medical record at every veterinary visit.
- Noted muscle loss should prompt nutritional assessment and investigation for common diseases associated with tissue wasting.
- Appropriate nutritional management and underlying disease treatment should be implemented in any animal with noted muscle loss.


