Intraveous fluid therapy (IVFT) is an essential pharmacological intervention for many patients in veterinary practice, and is prescribed by the veterinary surgeon (VS). Patients generally require IVFT if the following disturbances are detected:
Patients with medical conditions and emergency patients are the ones that people tend to associate the most with absolutely needing IVFT to aid their recovery, however it is also important to remember that perianaesthetic IVFT is also advisable. Davis et al (2013) highlighted the importance of IVFT for patients under anaesthetic, and outlined the key ways in which IVFT does help these patients:
Whatever the indication is for IVFT, the registered veterinary nurse (RVN) must be knowledgeable regarding patient assessment, fluid choices, goals associated with administration, how to monitor the efficacy of the infusions and how to prepare, administer and maintain an infusion correctly and safely.
Patient assessment and fluid selection
The VS will initially assess the patient by taking a history from the animal's owner, considering the main complaint or reason for presentation. A full physical clinical examination will be performed to identify some differential diagnoses, or indeed the definitive diagnosis, and establish the effectiveness of the patient's cardiovascular functioning and tissue perfusion.
Having gathered this information, the VS will make a decision regarding the need for additional diagnostic investigations, for example blood sampling and testing. It is recommended and considered good practice to obtain a baseline database for all patients with obvious or suspected fluid disturbances to facilitate effective progress monitoring.
There are many different types of fluid available for administration, which are different pharmacodynamically, and their effects on the body must be considered by the VS and what they hope to achieve for the patient. The two main types of fluids are crystalloids and colloids:
The VS will decide on the fluid type according to all laboratory data gathered and their findings from initial patient assessment. The choice will be the most appropriate fluid, or fluids, considering the patient's needs regarding circulating volume and tissue perfusion, the type of disturbance evident, and ultimately where the patient needs fluid replacement and maintenance: intravascularly or extravascularly (Clark, 2009).
Goals for IVFT
It is important for the VS to set goals for fluid administration and communicate these to the RVN. A patient receiving IVFT should receive regular reassessments to evaluate the efficacy of the infusion (Gurney, 2008). This will help to create an individualised IVFT treatment plan which is dynamic, meaning it is responsive to the changing needs of the patient. When setting goals and planning reassessment times, the VS will be mindful of: the nature of the fluid disturbance, whether it is acute or chronic; the pathology of the disturbance, whether there is an acid-base, oncotic or electrolyte problem; any comorbid conditions, so the presence of one or more additional disorders or diseases alongside the primary underlying disease condition (Davis et al, 2013).
Having established issues with hydration, tissue perfusion and fluid volume or loss, the VS will set and prioritise goals, select the most appropriate fluid, determine an administration rate and decide on the most appropriate route for administration. For example, in a hypovolaemic patient, there is a high risk of the patient developing shock due to the low circulating volume and subsequent cellular hypoxia. Reduced perfusion is a life-threatening situation (Sigrist, 2011), therefore, the VS may decide to administer crystalloid boluses to the patient to increase circulating volume.
Administration rates
Table 1 indicates bolus volumes for dogs and cats, and it must be noted these are maximum bolus volumes. A smaller dose of this total bolus volume, as determined by the VS, will be typically administered over 15 to 60 minutes, after which time the patient is reassessed to determine the efficacy of the fluid resuscitation (Aldridge and O'Dwyer, 2013). Repeat boluses can be administered and reassessed, ensuring the total doses in the table are not exceeded. When the desired effect has been achieved and circulating volume has been restored and deficits replaced, the VS will decide on a new fluid rate to maintain the patient, taking into account any ongoing losses.
| Dogs | Cats | |
|---|---|---|
| Severe hypovolaemia | 60–90 ml/kg | 40–60 ml/kg |
| Moderate hypovolaemia | 30–50 ml/kg | 10–20 ml/kg |
| Mild hypovolaemia | 10–20 ml/kg | 5–7 ml/kg |
Based on the research evidence they analysed, Davis et al (2013) recommended using the following maintenance infusion rates in dogs and cats:
They recommended calculating fluid deficit by multiplying an animal's bodyweight in kilograms by its percentage dehydration.
Aldridge and O'Dwyer (2013) suggested largely similar maintenance fluid rates for cats and dogs:
They recommended calculating fluid deficit by multiplying an animal's bodyweight in kilograms by its percentage dehydration and then by 10 (this last step is based on the estimate that 10 ml/kg of fluid is lost per 1% dehydration).
For paediatric patients, maintenance is recommended at 2–4 ml/kg/hour (Devey, 2007), but this again should be assessed according to the patient's clinical signs/physical status, bearing in mind that younger patients have higher fluid requirements.
Whichever calculation is used to determine fluid deficits and maintenance rates, the RVN must be astute to changes in a patient's clinical, physiological functioning and be able to relate these back to the provision of IVFT. In addition to the monitoring of IVFT and patient assessment considerations outlined earlier, it should be noted that central venous pressure (CVP) measurement is the most informative assessment method with regards to vascular filling, but it can only be measured if the patient has a central IV line in situ and the practice has the correct equipment (Aldridge and O'Dwyer, 2013); this negates its use in many practices, and blood pressure can be measured to assess or estimate the adequacy of tissue perfusion. The VS should always be made aware of all reassessment findings so they can decide whether the administration rate needs to be altered.
|
|
Step 1: Clarify with the veterinary surgeon their choice of fluid. |
| Step 2: Retrieve a bag of fluid and double check it is the right product, there is no precipitation, there is no damage to the packaging and that it is in date. | |
|
|
Step 3: Select a giving set. Remember to check it is the type of giving set you need, it is going to deliver the correct drops/ml you need, that the packaging is not damaged and it is in date. |
|
|
Step 4: Open the outer packaging and retrieve the bag of fluid. You may need scissors to assist with this, taking care not to puncture the bag. It is advised at this point to give the fluid bag a squeeze to check there are no leaks. |
|
|
Step 5: Hang the fluid bag on a drip stand. Some people prefer to lay the fluid bag on a table while spiking it, however this risks contaminating the port for the spike and it also risks piercing the bag (and potentially a finger) during insertion. |
|
|
Step 6: It is advisable to wash hands at this point. Open the giving set, remove any excess packaging materials and unravel it so the spike and chamber are in the dominant hand, and the rest of the giving set in the other hand. The end of the giving set should never contact the floor. |
|
|
Step 7: Fully close the regulator. |
|
|
Step 8: Remove the tab from the fluid bag insertion port, taking care not to contaminate the port post removal. |
|
|
Step 9: Remove the spike cover from the giving set, taking care not to contaminate the spike post removal. |
|
|
Step 10: Insert the spike into the insertion port of the fluid bag with a twisting motion. You may lose a few drops of fluid at this point. Aspesis must be maintained. |
|
|
Step 11: Squeeze the drip chamber until it is 1/2 to 2/3 full. The more controlled this is, the less air bubbles will be produced. |
|
|
Step 12: Using the regulator, slowly release fluid from the drip chamber into the line. The more controlled this is, the less air bubbles will be produced. |
|
|
Step 13: As the fluid runs through the line, it is advisable to invert the injection ports, i.e. turn the port so the injection bung is pointing towards the floor. Doing this, and slowing the fluid down a little, will help to avoid a large air bubble lodging in the port. Please note, it is normal for there to be a small air lock in the port. |
|
|
Step 14: The cap on the end of the giving set must not be removed until just before the line is attached to the patient's IV catheter, to maintain asepsis. It is acceptable to lose some drops of fluid from the end of the giving set as it is being primed to ensure the fluid is filling the line right to the tip. |
|
|
Step 15: The primed drip line should be checked along its entire length for significant air bubbles, i.e. those which extend across the whole diameter of the drip tubing. It is then hung over the drip stand ready to be attached to the patient — ensure the cap does not come off the end and avoid it touching any contaminated surfaces as it hangs. |
Monitoring IVFT — patient assessment
It was advised by Davis et al (2013) that the following parameters should be measured to comprehensively assess a patient and its hydration, perfusion and volume status:
Considering these recommendations, the RVN must be proficient in all of these physical checks and laboratory analyses, but also needs to ensure the practice's hospitalisation sheets are adequate for the recording of all of this information. Many of these parameters are numerical, however there should be room on the hospitalisation sheet for qualitative comments too.
Routes of administration and intravenous cannulae
The choice of route for IVFT administration is affected by many factors, and the key routes and considerations are outlined in Table 2.
| Route | Considerations |
|---|---|
| Per os (PO) | Not if the patient is vomiting |
| Subcutaneous (SC) | Isotonic fluids only |
| Intravenous (IV) or intraosseous (IO) | For hospitalised patients who are: |
| Central IV | Generally for critical care patients |
Davis et al (2013) provided guidelines for veterinary professionals regarding the use of IV catheters for IVFT, and this is a summary of their recommendations an RVN must be aware of in practice:
Additional equipment considerations, concerns and complications
Ideally, all patients receiving IVFT should have an infusion pump (Figure 1) controlling the rate. They will sound an alarm if there is high pressure and the infusion stops, or if there is air detected in the line. For every patient, the RVN should set:

There are different types of giving sets available for use which deliver different drops per ml. A standard giving set delivers 20 drops/ml, a paediatric one delivers 60 drops/ml and a blood giving set delivers 15 drops/ml. There are also giving sets available that are tinted (Figure 2), so they can be used to deliver infusions that have had light-sensitive drugs added to them, like metoclopramide. It would be prudent to change giving sets frequently if the same giving set is being used to spike multiple bags of fluid to reduce the risk of contamination.

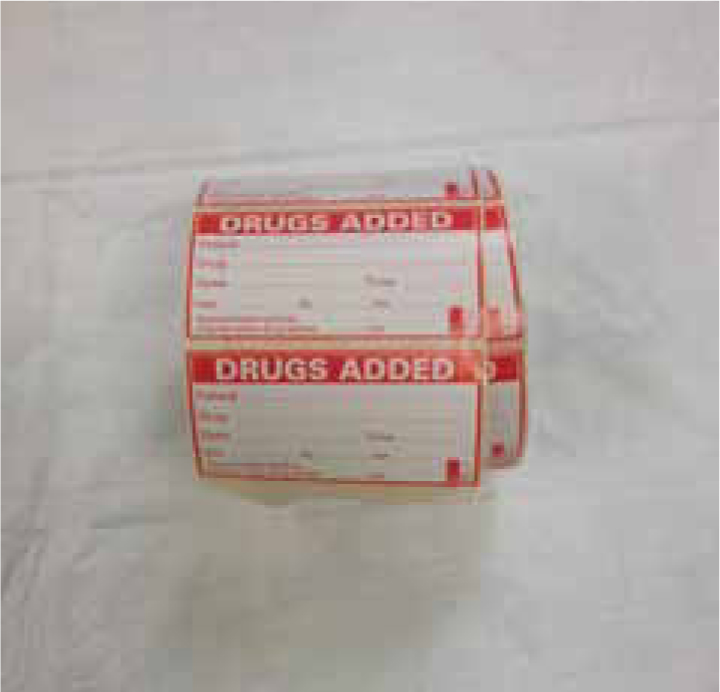
Crystalloid IV fluids can be ‘spiked’ with other drugs and administered to the patient, for example the addition of potassium for a hypokalaemic patient, or the addition of insulin for a hyperglycaemic diabetic ketoacidotic patient. In these circumstances the RVN should always affix a ‘drugs added’ label (Figure 3) to the fluid bag so everyone is aware that it is not a plain bag of fluids, and exactly how much of the drugs have been added.
There are many complications associated with the administration of IVFT which the RVN must be aware of, and early identification of problems can ensure the longevity of an IV catheter, and reduce the risks to patients. Table 3 outlines the key complications to be aware of, and advice regarding nursing actions.
| Problem | Recognition and advice |
|---|---|
| Volume overload | Tissue oedema — facial/distal limb swelling |
| Air emboli | Air embolus in the circulatory system |
| Extravasation | Swelling of tissues around/above the catheter site |
| Phlebitis | Inflammation of the vessel wall will result in erythema around the insertion site |
| Thrombosis | Blood clot forming in a vessel — associated with the catheter |
| Thrombophlebitis | Blood clot forming in a vessel secondary to phlebitis Remove and replace catheter |
Conclusion
An RVN has many responsibilities associated with the preparation and administration of IVFT in small animal patients. Davis et al (2013) stressed the importance of adequate staff training with regards to assessing a patient's fluid status, IV catheter placement and management, the use of equipment, the benefits and risks of IVFT and drug/fluid incompatibilities. It is indeed important that the RVN is knowledgeable and efficient in all of these things to ensure IVFT is effective and successful patient outcomes are achieved.

