Seizures are a period of disorganised brain activity where there is overstimulation of the central nervous system and random involuntary muscles spasms. From the author's experience, the presentation of patients suffering with seizures is common in an emergency practice, but can also be a regular occurrence in general practice, referral hospitals or in the home environment. Patients can present in a normal condition with the owners reporting seizure activity being witnessed at home; examples of clinical signs associated with seizure activity are discussed in Table 1. Patients can present in pre-ictal (also known as prodrome) and post-ictal states, they can suffer focal and cluster seizures and thus require treatment, or most seriously they can present in status epilepticus (Table 1). Some potential underlying causes of seizure activity in animals are detailed in Table 2, and are typically categorised as being extra-cranial or intra-cranial in origin.
| Seizure type | Definition | Clinical signs |
|---|---|---|
| Pre-ictal (prodrome) | Time period before the onset of seizure activity | Abnormal behavioural activity that the owner might notice. |
| Can last several hours to several days | ||
| Post-ictal | Time period following the seizure activity | Restlessness |
| Increased appetite/thirst | ||
| Disorientation | ||
| Blindness | ||
| Aggression | ||
| Can last several minutes to hours — occasionally days | ||
| Focal (partial) seizure | Elementary motor seizures which may progress into a generalised seizure. | Facial muscle twitching |
| Neurons in a region of the cerebral cortex are affected | Neck/shoulder/limb muscle involvement | |
| Impaired consciousness | ||
| Bizarre behavioural activity | ||
| Cluster seizures | Two or more seizures within a 24 hour period | Both cluster and SE seizures can be further classified as focal or generalised (which are both types of seizures in their own right, but can manifest as clusters or SE) |
| Focal — as well as the aforementioned clinical signs, dogs may ‘fly-bite’, become aggressive without provocation, howl and become restless. Cats may salivate, display hippus, vocalise excessively or perform random running behaviours (at home) | ||
| Generalised — are subdivided into tonic-clonic, clonic, myoclonic, atonic or absence types. The patient may suffer unconscious collapse and display signs associated with these subdivisions, including symmetrical abnormal involuntary muscle actions, urination and defecation | ||
| Status epilepticus (SE) | A state of continuous seizure activity lasting for 30 minutes or longer. Longer or repeated seizures with failure to return to normal within 30 minutes |
| Extra-cranial | Intra-cranial |
|---|---|
| Toxic, such as mycotoxins/metaldehyde/lead/ organophosphates/rodenticides | Cerebrovascular accident (CVA) |
| Electrolyte imbalances | Infections |
| Uraemic encephalopathy | Iatrogenic (insulin) |
| Hepatic encephalopathy | Trauma |
| Hyperosmolality | Metabolic storage disease |
| Hypoglycaemia | Neoplasia |
| Hypocalcaemia | Inflammation |
| Hyperviscosity | Idiopathic epilepsy |
| Congenital | |
| Lissencephaly | |
| Degenerative |
Clinical history
In spite of the underlying cause of the seizure activity, consent to treat the patient must be obtained from the owner along with a thorough clinical history. As soon as consent is obtained a team can be working on the patient while a colleague gathers information, including:
The person gathering this information must question the owner carefully to ensure all relevant and important information is extracted from them, while not giving them the opportunity to provide an irrelevant and often very detailed life-history of their pet. All information must be clearly and concisely reported to the veterinary surgeon (VS) in charge of the case to inform their treatment choices for the patient through the stabilisation period, and guide their ongoing management plans.
Stabilisation
On presentation, the VS and veterinary nurse (VN) should perform a rapid, thorough assessment of the patient, initially checking the patient's airway, breathing and circulation, accurately recording basic but essential parameters such as core temperature, pulse and respiration (TPR) (Cortellini and De Risio, 2010). The assessment method should be logical and systematic, and all members of the practice team should be familiar with the protocol to ensure there is consistency of care for all seizuring patients. The VS will also perform some form of neurological assessment on presentation, in order to help them potentially determine the origin of the seizure and obtain a baseline measurement of neurological function (Podell, 2009). It is often useful to dim the lighting when dealing with a seizuring patient, however the team still needs to be able to see what they are trying to do to the patient. Consider dimming the ward lighting when the patient is transferred to the intensive care ward to minimise stimulation, and try to ensure there are no noisy patients housed nearby and turn radios off as recommended by Polton and Brabscombe (2008) as these patients are hypersensitive to stimuli.
An intravenous (IV) cannula must be placed promptly to facilitate the administration of anti-epileptic medications and intravenous fluids (Feliu-Pascaul, 2008), which can be challenging in a moving target such as a seizuring patient. The VS may administer rectal diazepam to try and reduce the seizure activity at this point to facilitate IV cannula placement, but with good restraint of the patient it is not usually necessary. The attachment of a primed extension set is advised at this point so the team can administer medications easily should the patient continue or resume their seizure activity, if IV fluids are not being administered immediately.
It is essential to measure the patient's blood glucose (BG) levels, so having a glucometer in veterinary practice is advised or a blood gas analysis machine (Figure 1); normal laboratory biochemistry machines can be used to assess the BG levels, but in these cases a rapid assessment of the levels is warranted. Whether the patient is hypoglycaemic due to the underlying cause or due to the intense muscular activity during the seizure, hypoglycaemia is a common finding (Cochrane, 2007) and must be corrected to ensure nervous tissues, for example the brain, are receiving sufficient supplies to survive. As stipulated by Cochrane (2007), glucose supplementation should only be administered to patients if hypoglycaemia has actually been documented as it may otherwise contribute to lactic acidosis.

Anti-epileptic and other medications will be administered having established patent IV access, and some examples of the types of medications administered to seizuring patients are outlined in Table 3.
| Drug | Why used? | Dose |
|---|---|---|
| Glucose | If the patient is hypoglycaemic glucose diluted in saline must be administered at the direction of the VS | Dextrose 50% (5 mg/ml) at 1 mg/kg diluted at least 1:2 given as a bolus over 10 minutes |
| Diazepam | Benzodiazepine — potent, fast-acting anti-epileptic drug | 0.2-0.5 mg/kg IV or 0.5-1 mg/kg PR repeated two to three times over 5-10 minutes Constant rate infusion (CRI) at 0.1-0.5 mg/ kg/hour diluted in either 5% dextrose or 0.9% saline |
| Care if origin of seizure is liver related | ||
| Propofol | Propyl phenol — this is an anaesthetic induction agent | 1-2 mg/kg IV boluses to effect (up to 6 mg/ kg), then 0.1-0.2 mg/kg/min by CRI |
| Phenobarbital | This drug increases the seizure threshold required for seizure discharge. It helps to decrease the spread of the discharge to surrounding neurons | 12-24 mg/kg IV for immediate therapeutic concentrations (can cause a stupor and cardiovascular and respiratory depression at this dose) |
| 2-3 mg/kg IV, 15-30 minutes apart to effect Dose should not exceed 15 mg/kg/24 hours | ||
| Midazolam | Benzodiazepine like diazepam with a wide margin of safety and broad therapeutic index. Has shown to be safer and more effective in humans for the control of seizures than comparable diazepam doses | 0.066-0.3 mg/kg IV or IM |
| Can be mixed with glucose or saline solutions | ||
| Care if origin of seizure is liver related | ||
| Levitiracetam | Its action against seizures is not fully understood. It seems to decrease the onset of seizures and has been documented as the most well tolerated anti-epileptic drug in humans | 60 mg/kg IV bolus for rapid therapeutic levels 5-25 mg/kg every 8-12 hours PO — generally three times daily |
| Mannitol | Osmotic diuretic and mild renal vasodilator. If status epilepticus is severe and cerebral oedema is suspected then mannitol can be used. Immediate plasma expanding effect, reducing blood viscosity and increases cerebral blood flow | 0.25-1.5 g/kg IV over 15-20 minutes |
| Should be followed with IV crystalloids | ||
| Is contraindicated in dehydrated patients |
Having administered the medications as per the VS' instructions, the VN must continue to monitor the patient's core temperature and take action appropriately. Typically patients will be hyperthermic on presentation due to the intense muscular activity, so active cooling methods must be used if the temperature is greater than 40.5°C (Cochrane, 2007), such as wrapping the IV line around an ice pack, putting a fan on the patient, administering cool IV fluids and applying surgical spirit to the foot pads (Figure 2). Many practices use cold, wet towels over the patient in an effort to cool them down, however this should be avoided because they can warm up quite rapidly and thus start warming the patient instead by insulating them. Other more invasive methods of achieving rapid cooling could be used if indicated, such as bladder lavage and cold water enema. The VN must be acutely aware that when employing active cooling methods the patient's core temperature must be monitored very closely, such as every 15 minutes initially, to avoid rebound hypothermia; cooling methods should be discontinued when the temperature reaches around 39.5°C with continued monitoring (Cochrane, 2007). If they have suffered a degree of brain damage, either confirmed or unconfirmed at this point, the thermoregulatory centres in the brain may be affected, and along with the physiological cooling side effects of anaesthetic drugs such as propofol it could mean the patient becomes readily hypothermic; this is another reason why very regular monitoring is essential.

Seizuring patients should receive 100% oxygen therapy to ensure optimal tissue per-fusion is maintained, and the efficacy of oxygen therapy can be assessed most accurately via blood gas anaylsis. The method of oxygen delivery will differ according to the patient's status, for example if the patient is conscious a mask, nasal prongs or nasal cannula may be indicated or if they are unconscious delivery via an endotracheal tube is most appropriate (Cortellini and De Risio, 2010) (Figure 3). The method of oxygen delivery should be decided on having assessed the patient to decipher which method will cause the least distress. For example, some patients tolerate nasal prongs and catheters very well, while others are irritated by them and try to remove them physically or via the sneezing reflex. Sneezing and stress should be avoided to ensure the patient's intra-cranial pressure does not increase, so the VN must be mindful of this and able to provide oxygen in a variety of ways. Oxygen therapy should automatically be one of the first interventions the VN provides the patient with on arrival, and hopefully with the aid of colleagues many of these interventions will be happening simultaneously.

When the patient is relatively stable, i.e. when the seizure activity has been stopped and patent IV access has been achieved, the VS will perform a secondary survey including another full physical examination and neurological examination; when treating emergency patients such as seizuring patients it is essential the VS has goals or end-points to work towards, against which they can assess the efficacy of their initial treatment interventions. Neurological assessment will involve the assessment of reflexes and responses to stimuli, and an objective scoring system can be useful to monitor neurological status at least twice daily, such as the Modified Glasgow Coma Scale (MGCS) (Holowaychuk et al. 2007). Alongside this, the VN should be aware of the Cushing reflex and its associated signs, which may be indicative of increased or increasing intra-cranial pressure. The classic signs associated with the Cushing reflex include:
As discussed by Holowaychuk et al (2007), evidence of bradycardia along with hypertension should suggest to the VN that the intracranial pressure is increasing and should be reported to the VS immediately as this situation is life threatening.
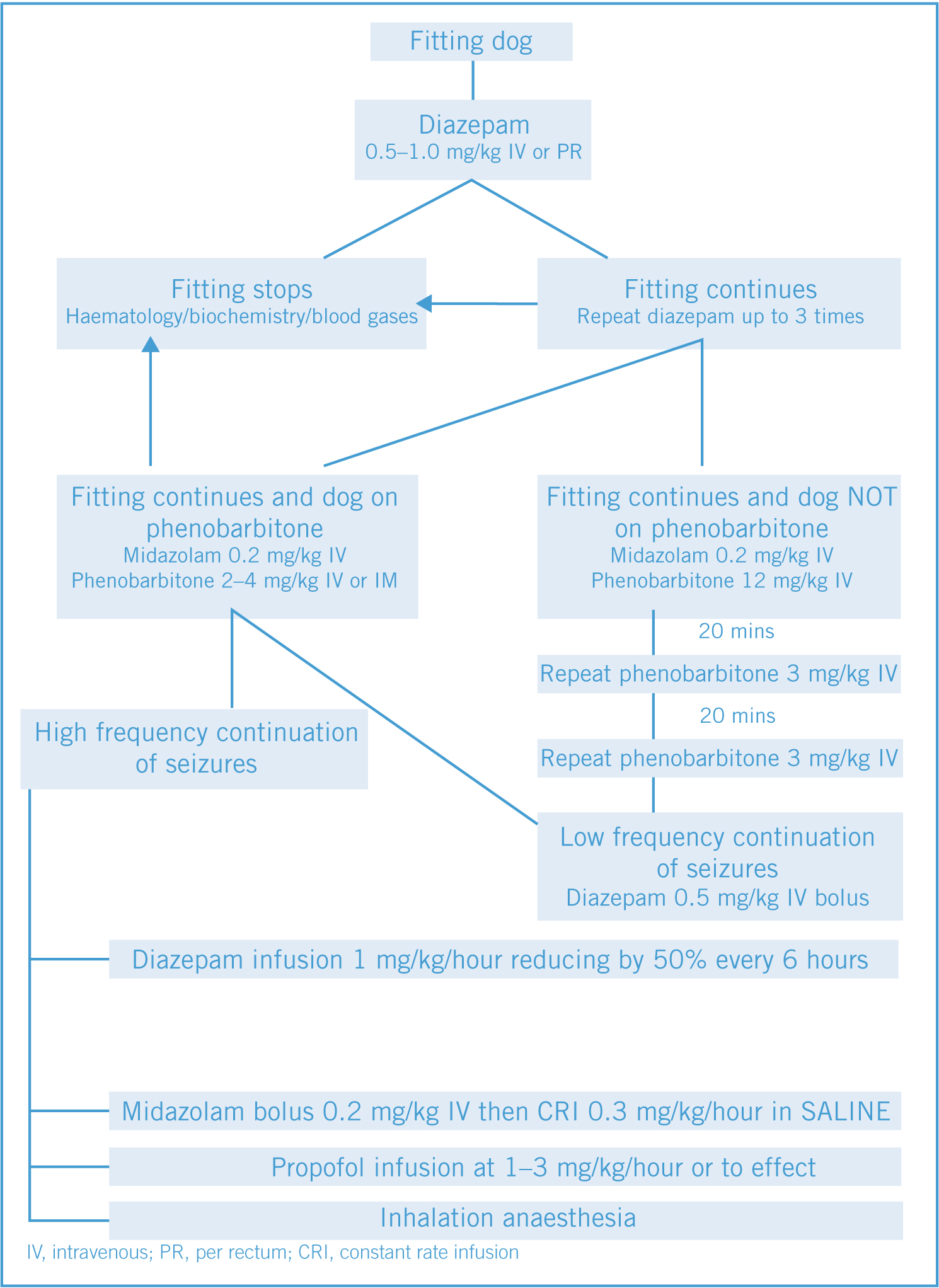
Most practices will have an algorithm in their practice protocol to guide team members in the treatment and decision making when dealing with seizuring patients. An example of such an algorithm can be seen in Figure 4, which would be suitable to following if a dog presented in practice suffering a seizure.
Ongoing treatment and monitoring
Having controlled the seizures according to the algorithm in Figure 4, individual patients can have very different ongoing needs and monitoring requirements. Some patients will recover from seizure activity and be hospitalised for observation of further or subsequent seizures. These patients will require ongoing temperature monitoring until normothermia is achieved and maintained, should be fed and given water, and they may be on IV fluids until they are haemodynamically stable.
Some patients do not recover from the seizure activity, and as the effects of the anti-epileptic medications wane seizure activity may resume. In these cases the patient will be set up on some form of constant rate infusion (CRI) as per the algorithm; propofol infusions are typically used (King and Boag, 2007), delivered using an infusion pump or syringe driver for accurate dosing (Figure 5). A simple calculation to use to mix an appropriate propofol infusion is: dilute 1 part propofol: 4 parts saline, deliver at three times maintenance infusion rate initially reducing to one times maintenance (maintenance fluid rate is 50 ml/kg/24 hours) as required according to the patient's clinical condition and vital signs. This ratio of propofol to saline has been used successfully in numerous patients in a practice the author is familiar with; other VS may have their own preference for mixing propofol infusions for their patients, or may use undiluted propofol via a syringe driver. This choice of delivery is the remit of the prescribing VS only.

Patients that are being maintained on CRIs must be closely monitored by the VN, who should be familiar with the drugs being administered in this way so they can identify any expected or unexpected side effects (Bell, 2009). The following should be checked or performed regularly in addition to the maintenance of IV fluid therapy, active cooling or warming and administration of oxygen therapy:
Seizuring cats
In veterinary practice the majority of the seizuring patients admitted for treatment are dogs; cats are presented due to seizuring much less frequently, and tend to exhibit partial seizures rather than generalised seizures (Garosi, 2009). The main causes for seizure activity in cats include:
Cats will present with symptoms outlined in Table 1 depending on the seizure type, but they can also display signs such as growling, rage, running in circles, floor licking, tail chasing and unprovoked aggression (Garosi, 2009) (Figure 6).

The treatment of a seizuring cat is symptomatic as it is in dogs, and commonly used anti-epileptic medications include phenobarbitone and levetiracetam (Garosi, 2009). Baseline bloods to include a complete blood count, biochemistry analysis, thyroid profile and bile acids are essential, along with blood pressure measurements and urinalysis to determine if there are any underlying medical conditions (Garosi, 2009). They will require patent IV access, oxygen therapy, active cooling and anti-epileptic medications such as diazepam to control their initial seizures, but their ongoing management and prognosis will be dictated by the underlying cause.
Cats that are seizuring due to permethrin intoxication are a common scenario in emergency veterinary practice (Sutton et al. 2007; McLean and Hansen, 2012). Such cases are starting to be treated with intralipid therapy, which is a 20% IV lipid solution typically used as a fraction of total parenteral nutrition (Gwaltney-Brant and Meadows, 2012)(Figure 7). It was discovered in humans that the lipids would attract and bind with lipophilic drugs, such as permethrin, and process them out of the body as any other lipid would be (Michigan Veterinary Specialists 2012). They have recently been successfully used in veterinary practice to treat permethrin overdose in cats, reversing the central nervous system clinical signs of toxicity, reversing associated cardiac arrhythmias and ultimately decreasing a patient's hospitalisation while promoting a favourable prognosis (Gwaltney-Brant and Meadows, 2012).
Conclusion
The prognosis for seizuring patients is very much an individual phenomenon. Some patients that one would not expect to survive make a fantastic recovery, whereas others never recover and have to be euthanised. Their survival depends on the underlying cause of the seizure activity, the type or severity of seizure activity, how quickly the owners sought veterinary attention and the appropriateness of the treatment regimen devised and provided by the veterinary team.
