References
The highs and lows of electrolytes part 1: sodium, chloride and potassium
Abstract
There are six electrolytes that are important in maintaining homeostasis within the body. They play vital roles in regulating neurological, myocardial, muscular and cellular functions and are involved in fluid and acid–base balance. Recognising and treating electrolyte derangements is an important role for veterinary nurses especially in emergency and critical care patients. This series of two articles will discuss the physiology behind each of the six major electrolytes and discuss how to monitor and treat any abnormalities.
An electrolyte is a substance that dissociates into ions in solution and is capable of transporting an electric charge. Electrolytes can be positively or negatively charged and are balanced within the body. Positively charged ions are cations and negatively charged are anions.
The major electrolytes in the body include:
Electrolytes help regulate fluid balance, nerve and muscle function and maintain blood pH. Concentrations of electrolytes are closely controlled by the action of different hormones and the kidneys. Derangements can affect many body functions including cardiac, skeletal muscle function and the nervous system. The first part of this two part series will look at sodium, chloride and potassium.
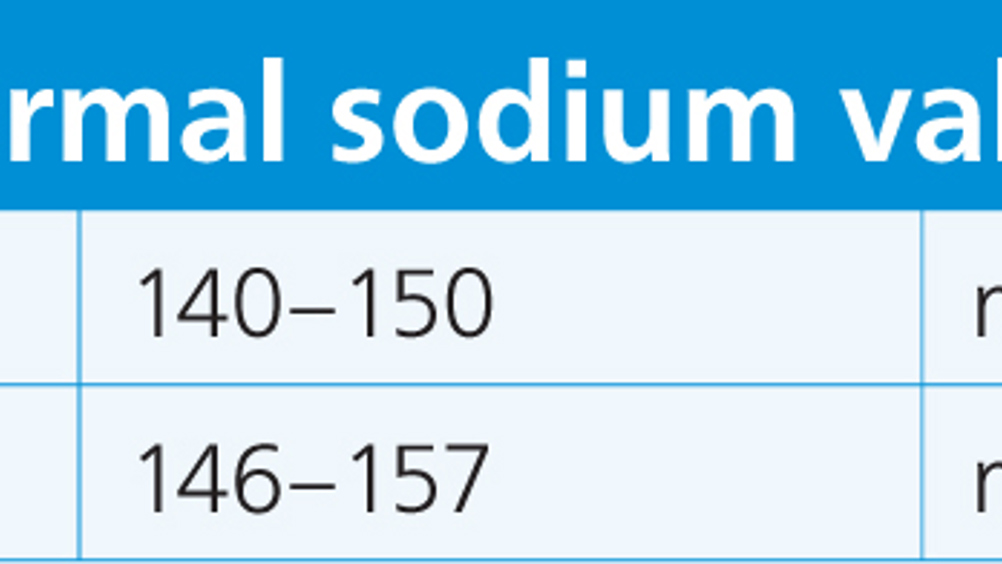
Sodium is the major body extracellular cation and maintains the osmolality of extracellular fluid. Normal values are around 140 milliequivalents (mEq)/litre in extracellular fluid and 10–12 mEq/litre in intracellular fluid (Scalf, 2014).
Most sodium concentration disturbances are caused by abnormalities in water handling rather than a change in the number of sodium molecules.
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

