The role of a registered veterinary nurse (RVN), involves nursing patients to a high standard of care, which requires the understanding and awareness of a patient's level of comfort and wellbeing. RVNs have an ethical responsibility to ensure patients are not suffering and an understanding of analgesics is required for RVNs to be able to assist in alleviating pain. Pain is now well recognised as something that animals feel (Owen, 2011), probably in much the same way as humans. It is no longer accepted that pain is beneficial by preventing any further injury, and it is understood that it may in fact be detrimental to long-term wellbeing (Hoad, 2013). RVNs therefore play an integral role in recognising pain and its symptoms, whether it be through the use of pain scoring charts or observation of behaviour.
RVNs play an important role in anaesthesia; although the veterinary surgeon (VS) is by law solely responsible for administration of anaesthetics, RVNs may act on behalf of the VS. Currently, under Schedule 3 of the Veterinary Surgeon's Act 1966 RVNs may administer a specific quantity of a drug to induce or maintain anaesthesia, but incremental dosing or dosing to effect must be done by the VS. However, the adjustment of a volatile agents by the VS would be difficult in practice as they would usually be aseptically involved in an operation, therefore RVNs are able to perform this adjustment on behalf of the VS. By monitoring physiological parameters of a patient under anaesthetic, the RVN can compile information that helps them assess the depth of anaesthesia and the amount of volatile agent needed to maintain an anaesthesia to an adequate depth. It is important that where multimodal analgesia is used, RVNs recognise that an effect on the patient's physiology will be produced, and the amount of other drugs required for a balanced anaesthesia may change.
Pain and nociception
Pain can be described as an awareness of an unpleasant sensation associated with actual or potential physical trauma and tissue damage (Merskey and Bogduk, 1994). The term pain refers to the conscious perception of a noxious stimuli. Nociception is the term used to describe the electrical impulses that trigger the physiological response to the noxious stimuli. When tissue damage occurs in-flammatory mediators are released and these excite the surrounding nociceptors, which are free nerve endings involved in the pain pathway (Flaherty, 2009a). The pain pathway, or nociception, consists of four stages; transduction, transmission, modulation and perception (Thompson, 2004).
The transduction stage is when a noxious stimulus causes inflammatory mediators, such as prostaglandins, to be released by damaged tissues. These substances are converted to electrical energy by nociceptors (Self, 2012). Pain can be inhibited at this stage by the use of non-steroidal anti-inflammatory drugs (NSAIDs), opioids and local anaesthetics (Thompson, 2004).
At the transmission stage energy travels via peripheral nerve fibres to the spinal cord where local anaesthetics and alpha-2 agonists can be used (Thompson, 2004). At the dorsal horn of the spinal cord the pain is modulated and can be enhanced or inhibited at this stage by the use of local anaesthetics, opioids, alpha-2 agonists, N-methyl-D-aspartate (NMDA) antagonists, NSAIDs and glucocorticoids (Thompson, 2004). The energy then transmits to the cerebral cortex in the brain where perception occurs leading to the conscious feeling of pain, this is where general anaesthesia, opioids and alpha-2 agonists are effective (Thompson, 2004), as although the pain signals are still travelling up to the brain, the anaesthetised patient does not perceive it; therefore this is known as nociception.
‘Wind up’
‘Wind up’ is the term used when central hypersensitivity develops in response to a repeatedly painful stimulus (Grape and Tramer, 2007). Hyperaesthesia is an exaggerated response to a noxious stimuli and can progress to a state where pain is perceived even by an innocuous stimulus, known as allodynia (Challis and Seymour, 2008), and includes a state of hyperalgesia where a painful stimulus is amplified (Flaherty, 2009b). Grape and Tramer (2007), outlined that peripheral neurons become excited for longer due to a prolonged stimulus and the pain threshold is lowered. Modulation occurs in CNS pathways from minor nociceptive stimuli and sensitisation occurs in the dorsal horn of the spinal cord, where NMDA receptors are found (Self, 2012), and in higher structures. Neurons develop a ‘memory’, and begin a rapid and exaggerated response to a small stimulus, known as central sensitisation (Hamilton, 2003). Pain can become chronic and pathological or maladaptive (Hellyer et al, 2007; Epstein et al, 2015), leading to a much more complex consideration of the use of analgesia (see Table 1 for pain definitions).
| Description | ||
|---|---|---|
| Nociception | A response by the peripheral neurons to a noxious stimulus | |
| Inflammatory pain | A response by the immune system in response to injury or infection | |
| Pathological pain: | ||
| Peripheral and central hypersentisization | Subgroup: Hyperalgesia Allodynia Neuropathic | Exaggerated response to noxious stimulus |
The effect of pain and nociception
Pain and nociception causes a stress response by the body led by the endocrine system contributing to the release of corticosteroids (Hellyer et al, 2007), such as cortisol. Cortisol can cause delayed wound healing at a cellular level (Hoad, 2013) and increase recovery times, prolonging hospitalisation. Pain and nociception causes the release of inflammatory mediators reducing gut motility and causing sleep deprivation (Hellyer et al, 2007). Catecholamines are released in the stress response to nociception and affect the stability of the heart by causing vasoconstriction leading to hypertension and tachycardia (Hellyer et al, 2007), both of which are undesirable during anaesthesia. If surgery involves the thorax or cranial abdomen nociception may impede ventilation leading to hypoxia, hypercapnia and respiratory acidosis (Bell, 2009). Pain can also lead to delayed recovery, a reduced appetite leading to weight loss, and cause behavioural changes such as depression and aggression (Roberts, 2008). Analgesia is defined as the abolishment of the sensation of pain (Owen, 2011); analgesics are commonly used within the veterinary industry, although completely abolishing pain is difficult. The aim for veterinary nurses is therefore to recognise and understand pain and nociception in order to help reduce them.
Pre-emptive and multimodal analgesia
Pre-emptive analgesia is given before a painful procedure is performed in an attempt to reduce the nociceptive response and reduce the amount of postoperative analgesia required (Flahery, 2009b). The use of pre-emptive analgesia can also reduce the length of hospital stay times, hasten recovery times and promote a more comfortable and favourable result (Owen, 2011). Multimodal analgesia could be described as balanced analgesia (Hoad, 2013), in which two or more drugs that act on different pain pathways are used symbiotically. The outcome of the use of these different classes of drugs is a better control of pain (Owen, 2011). Multimodal analgesia is beneficial in lowering the therapeutic doses required of some of the drugs involved, consequently reducing the risk of their side effects (Slingsby, 2008).
Ketamine
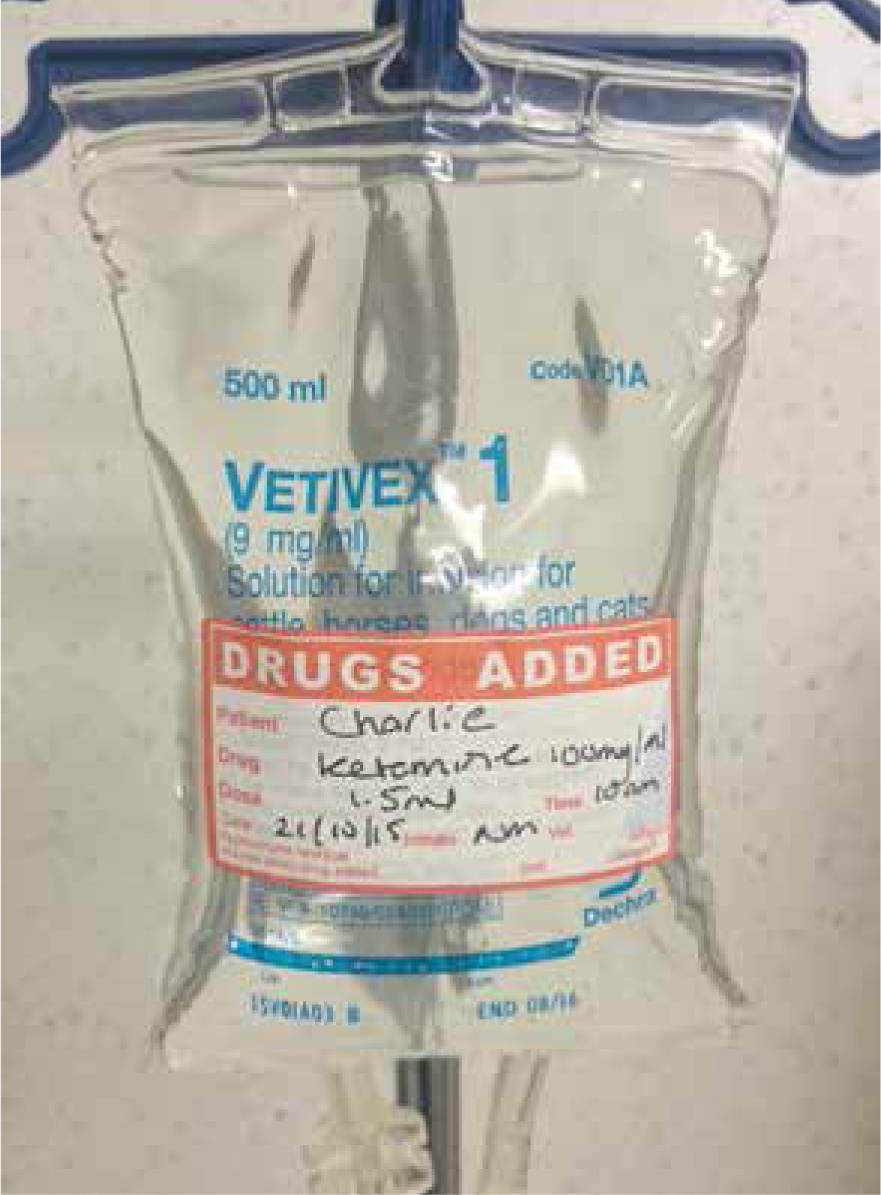
Ketamine is a dissociative anaesthetic that has been used for many years, known more commonly for its use in feline and equine patients as part of an anaesthetic protocol (Figure 1). It is a cyclohexamine derivative that affects the central nervous system (CNS) inducing superficial sleep and amnesia, its side effects include seizures, cardiovascular stimulation and muscle hypertonicity. In recent years the use of ketamine in subanaesthetic doses in canines has become more common as part of multimodal analgesia (Bergadano et al, 2009). Ketamine is a non-competitive NMDA receptor antagonist that can prevent and treat central hypersensitivity (Schmid et al, 1999; Hamilton, 2003; Gurney, 2012; Self, 2012). NMDA receptors play an important role in modulating the perception of pain, and links have been made from these excitatory receptors to the development of pain ‘wind up’, central sensitisation and pathological pain (De Kock et al, 2001; Grape and Tramer, 2007). Ketamine behaves similarly to opiates and some alpha-2-adrenoceptor agonists exerting its analgesic effect by activating the monoaminergic descending inhibitory system, which plays a role in modulating nociceptive information (De Kock and Lavand'homme, 2007). Ketamine can bind to some opioid receptor sites stimulating them, interfering directly in the inflammatory reaction (De Kock and Lavand'homme, 2007). De Kock and Lavand'homme (2007) and Bergadano et al (2009) suggested that treatment and prevention of postoperative hyperalgesia may reduce the incidence of chronic pain. Ketamine improves the antinociceptive properties of opioids and alpha-2 agonists by increasing the sensitivity of the receptors (Bromley, 2013). The use of keta-mine in subanaesthetic or low dose constant rate infusions (CRIs) provides analgesia (Figure 2) without dysphoria or other unwanted side effects such as cardiovascular stimulation, muscle hypertonicity and CNS stimulation (Schmid et al, 1999, De Kock and Lavand'homme, 2007, Flaherty, 2009a, Hadi et al, 2013).

The benefits of the use of ketamine
De Kock et al (2001) investigated mechanical wound hyperalgesia which was reduced by the use of a subanaesthetic dose of ketamine given intravenously and reduced early morphine consumption. Residual pain was not evident until the sixth postoperative month, which suggested that ketamine may play a role in chronic pain management, and reduces the need for ‘rescue’ pain medication. Also keta-mine can reduce the perception of pain in the postoperative period when administered pre-emptively (Wagner, 2002; Buvanendran and Kroin, 2007).
Pain can induce anorexia (Bell, 2009), and Sarrau and Jourdan (2007) found a link between the administration of ketamine post-operatively and the feeding behaviour in dogs. They suggested that its use may augment their appetites following surgery due to the decreased amount of pain felt compared with patients that had not received keta-mine. This could reduce hospitalisation time which is beneficial to the dog's stress levels and potentially contribute to wound healing due to the energy received from eating food. A study by Wagner (2002) found that peri-operative ketamine improved dog's activity levels and reduced pain scores in the postoperative period, indicating comfort. The patient's mobility level is one of the activities of living discussed by Orpet (2011) and is regularly included in care plans produced by RVNs, as impaired mobility can lead to oedema, thromboembolism, constipation and urine retention (Bell, 2009), and is linked to decreased quality of life. Therefore, the use of ketamine should be considered both peri and post-operatively to prevent anorexia and aid mobility.
Research conducted by Love et al (2011) outlined that the use of ketamine as part of a multimodal analgesia regimen during intraoperative anaesthesia, may facilitate the reduction of the volatile agent being administered. It is important that RVNs understand why this is and how it affects the patient physiologically. Some volatile agents cause vasodilation and hypotension (Flaherty, 2009a), and other undesirable traits, therefore, if it is possible to reduce the severity of these effects by reducing the dose of the volatile agent, a RVN should aim to do this under the direction of the VS.
Ketamine may exert an opioid sparing effect (Schmid, 1999, De Kock et al, 2001, Visser and Schug, 2006; Bonnet and Marret, 2007; Buvanendran and Kroin, 2007; Hadi, 2013) although this may be difficult to determine in animals given they cannot self-administer analgesics like humans using a patient controlled analgesia (PCA) device; instead RVNs must use pain scoring tools and observe behaviour.
The nurse's role in pain management
As the main carer of inpatients, RVNs are best placed to assess pain, but this is difficult as it is not objectively quantifiable and differs greatly amongst patients (Clapham, 2012). Pain assessment tools should be standardised and made to be measurable in a clear and concise format. An anthropomorphic approach can be taken by assuming that what would be painful to a human would probably be painful to an animal, given the anatomical similarity of pain pathways in humans, dogs and cats (Hellyer, 2007). Observation of behaviours, general demeanour, posture and appetite are just some of the signs used to assess pain levels, but are not an accurate measurement (Roberts, 2008). Animals need to be assessed as individuals as what one animal may find painful another may not, or they may be better at hiding their pain symptoms (Vedpathak et al, 2009) particularly in different species. The use of a validated pain scale chart, such as the Glasgow short form composite pain scale, to objectify pain and give a clear indication of whether the level of analgesia is adequate or not should be used to enable RVNs to assess their patients correctly and implement nursing procedures. Bell (2009) suggested that a positive response to the administration of an analgesic could be considered ‘gold standard’. Perhaps pain scoring should be included in hospitalisation charts in practice as some authors have referred to it as the fourth vital sign (Clapham, 2012). A study using multimodal analgesia alongside a nursing care plan could be done to assess whether its use had a direct effect on the daily activities of living according to Orpet and Jeffery's (2007) model. Human paediatric pain scoring methods should be investigated as communication problems are similar from a pain scoring perspective; RVNs could look at the behavioural measurement tools used in human nursing such as the VAS and translate them into a form of veterinary pain assessment.
Conclusion
Multimodal analgesia affects the perioperative period allowing the RVN to use a lower dose of volatile agent to achieve an adequate surgical plane (Love, 2011), while at the same time reducing undesirable side effects from these agents such as hypotension and vasodilation, perhaps making the anaesthetic period safer and smoother. During the monitoring of a general anaesthetic if the patient is showing signs of nociception there is a temptation to increase the volatile agent, RVNs must explore the use of additional analgesia in these cases, such as administering ketamine, and discuss this with their VS. Multimodal analgesia with the use of ketamine can make the postoperative period more comfortable for the animal as well as potentially reducing long-term wound hyperalgesia (Bromley, 2013) and chronic pain (Schmid et al, 1999, Bergadano et al, 2009). Procedures such as orthopaedics, celiotomies, total ear canal ablations and bulla osteotomies, thoracic surgeries, anal sac removal and even ‘routine’ procedures such as ovariohys-terectomies are just a few surgeries that could be considered eligible for multimodal analgesia (Figure 3). In addition, multi-modal analgesia may be beneficial to medical patients with conditions such as pancreatitis, burns, ophthal-mologic, neuropathic and oncological problems to name a few. It is important that the RVN has an understanding of the pharmacology of the drugs used and their side effects in order for them to care appropriately for their patients. To relieve pain and suffering gives the RVN greater job satisfaction and peace of mind that morally and ethically they have performed their duty to the best of their ability.


