References
How to accurately measure blood pressure
Abstract
One very important clinical skill for every veterinary nurse is the accurate measurement of arterial blood pressure in both conscious and anaesthetised patients. These readings are useful for a wide variety of monitoring as well as diagnostic purposes. It is critical to produce accurate results so that patients may receive the best care and treatment as soon as possible. If blood pressure measurement is not performed correctly there is the possibility of an error, which can negatively impact patient management. Blood pressure measurements are sensitive: their accuracy can be affected by the environment the patient is in, the patient's behaviour, measurement procedures, devices used for the measurement and the nurse or clinician carrying out the measurement. To minimise errors in blood pressure measurement, a detailed, standardised measurement protocol is necessary with adequate training. This allows for accurate, repeatable and reliable measurement of blood pressure to be achieved each time.
Arterial blood pressure is a common parameter assessed in both conscious and anesthetised patients for numerous reasons. These include monitoring disorders, such as renal disease, cardiovascular disease and endocrine disease, and, most commonly, as a parameter to monitor the cardiovascular status of an animal under anaesthesia. Measuring blood pressure is a widely recognised element in patient care because both hypertension and hypotension can significantly affect the health of patients (Sturgess, 2016).
This article summarises both invasive and non-invasive blood pressure (NIBP) techniques available to measure arterial blood pressure in patients and discusses the causes of potential errors that may lead to inaccurate measurements. It describes the proper use of blood pressure measurement devices and interpretation of the measurements obtained from them.
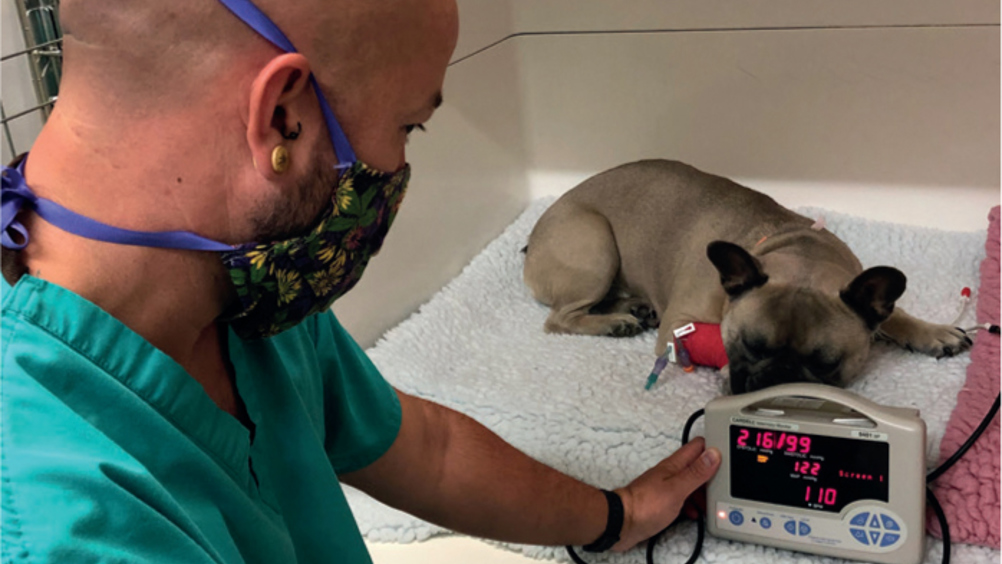
Blood pressure, or more accurately intravascular pressure, is the pressure that blood physically exerts on a vessel wall. This pressure is important because the difference in intravascular pressure at any two points in the vascular network is the driving force for blood circulation. The pressure found at the root of an aorta is much more than the vena cava pressure, ensuring blood will flow from the arterial side to the venous side, delivering nutrients and oxygen to cells located along this path. The most common intravascular pressure measured in small animals is the peripheral arterial blood pressure. This is most commonly measured indirectly via a surface-applied pressure cuff around a limb or tail base using flow detection methods such as oscillometry (Figure 1) or Doppler ultrasound (Figure 2) (Clarke et al, 2015; Haskins, 2015).
Register now to continue reading
Thank you for visiting The Veterinary Nurse and reading some of our peer-reviewed content for veterinary professionals. To continue reading this article, please register today.

