Dental and oral health conditions are common in veterinary patients with periodontal disease — affecting around 80% of dogs and 70% of cats over the age of 3 years (Wiggs and Lobprise, 1997; Lund et al, 1999). A survey by Kyllar and Witter (2005) found that only 7% of the dogs examined could be considered orally healthy. Registered veterinary nurses (RVNs) — especially those involved with nurse-led consultations — require the ability to identify oral health conditions and explain the consequences and necessary treatment options to pet owners. Advising clients on effective dental home-care options and products is an important component of this. The benefits and limitations of each oral healthcare treatment or product should be evaluated thoroughly before discussion or recommendation.
Dental home-care products and diets are designed to reduce the accumulation of plaque or calculus on the tooth's surface. It is important to determine the credibility of a manufacturer's claims by assessing the available research or evidence. The current article will focus on dental hygiene for canine and feline patients, and preventing periodontal disease, although other dental conditions will be mentioned. Discussing dental treatment and adjunctive perioperative dental products is beyond the scope of the article.
Background
A daily oral hygiene regimen should be part of every dog and cat's routine, and advising owners on suitable options, and helping them implement these, is an important aspect of the RVN's role. Regular review appointments can help with compliance. As outlined by Holmstrom et al (2013), it is a current recommendation that canine and feline patients attend their veterinary clinic for an oral examination every 6–12 months. Patients with established disease or those predisposed to oral health conditions will require more regular reviews approximately every 1–3 months. Applying plaque disclosing solution to the patient's mouth at these review appointments will highlight the plaque and calculus present. Performing this at postoperative rechecks — 7–10 days post dental treatment — can prove a huge motivator for clients to implement toothbrushing and effective oral hygiene as it demonstrates how quickly plaque will establish following professional cleaning.
Most veterinary dental home-care products are not classified as medicinal products and, as such, scientific research is not always a requirement. Reputable companies will carry out controlled trials to check the efficacy and safety of the product. Along with personal experience, using evidence-based veterinary medicine (EBVM) can help veterinary professionals to form clinical judgements on the products to recommend (Roudebush et al, 2005). Products that claim to remove tartar either manually or chemically should be treated with caution as the claims are likely to be exaggerated and these objects may be too hard, resulting in tooth damage. Objects that are too hard to pit with a finger nail or do not flex easily by hand should be avoided.
The Veterinary Oral Health Council (VOHC) was developed to provide a seal of acceptance for oral hygiene products that meet their criteria. A manufacturer will submit statistical data from two clinical trials (to ensure repeatability of results), which demonstrate a product's efficacy at controlling plaque and/or calculus. Only data from parallel group or cross-over trials and products without safety concerns are considered. The VOHC board will review data and information for a product or product line. If this meets all of the requirements, the product will be awarded the VOHC seal of acceptance which can be displayed on the product's packaging (Figure 1). Although submitting data to attain a VOHC seal is entirely voluntary, it does provide some assurance of a product's efficacy if used in accordance with the manufacturer's guidelines. Further information and a list of approved products can be obtained at www.vohc.org. Some VOHC products may be difficult to source outside of North America, or be branded under a different name in other countries.

Periodontal disease and its prevention
Periodontal disease or periodontitis is the most common infectious disease in dogs and cats, and is linked to systemic effects and disease of multiple body organs. Although dated, a seminal paper by DeBowes et al (1996) demonstrated a significant link between an increase in systemic disease of multiple body organs with increasing severity of periodontal disease. If left untreated, the pain and infection caused by periodontal disease will have a negative impact on quality of life. Periodontitis is caused by the accumulation of plaque and bacteria on the tooth's surface and the surrounding gingiva. Plaque is described as a biofilm mainly consisting of salivary proteins, debris and bacterial flora found in the oral cavity. If plaque is not removed daily from the tooth's surface, it begins to organise, calcify and form calculus (tartar). Calculus itself does not cause periodontal disease but provides a larger, rough, surface area to further facilitate plaque accumulation and maturation.
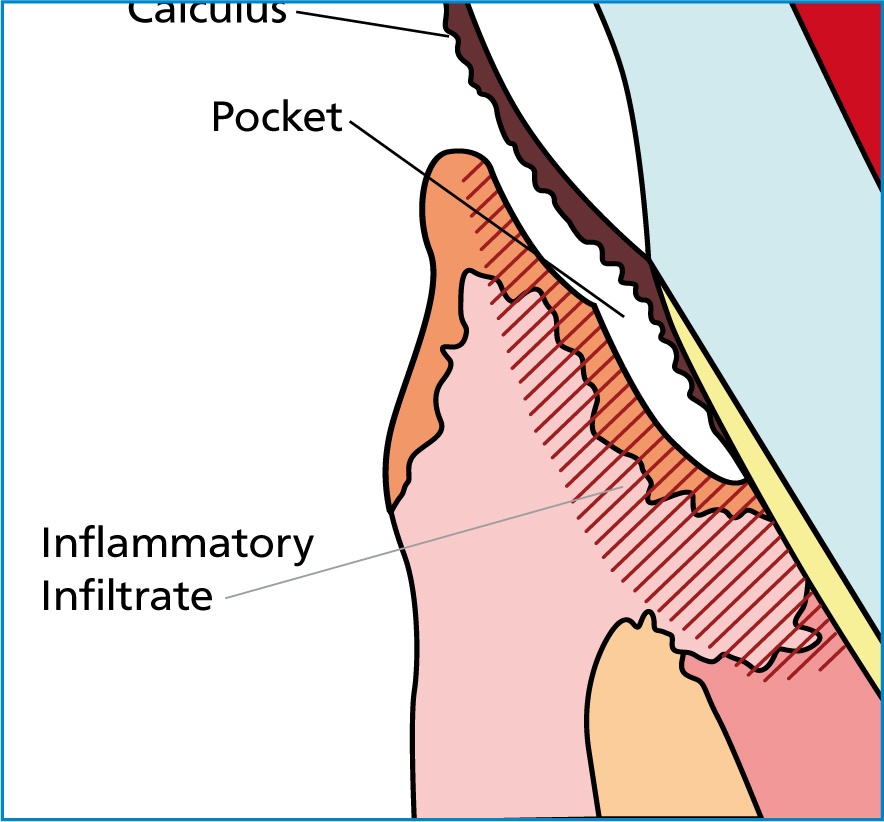
As plaque and calculus gathers around the gingival margin and sulcus, disease-causing anaerobic bacteria thrive in this oxygen-deprived environment (Boyce et al, 1995). Mature plaque is bacteria-laden. Once this infiltrates the gingival sulcus, it leads to inflammation (gingivitis) and eventual destruction of the periodontium — the supportive structures of the tooth which can be seen in Figure 2. Without treatment, progressive attachment loss will eventually result in tooth loss. The severity of periodontal disease is staged according to the percentage of attachment loss to the periodontium (Table 1).
| Stage | Description | Presentation |
|---|---|---|
| Stage 0 | Normal periodontium | Normal, healthy gingiva with little or no calculus visible |
| Stage 1 | Gingivitis | Redness and inflammation of the gingiva is present but no attachment loss has occurred |
| Stage 2 | Mild periodontitis | Up to 25% attachment loss of the periodontium is present. This is visible on dental radiographs |
| Stage 3 | Moderate periodontitis | Between 25 and 50% attachment loss of the periodontium is present. This is visible on dental radiographs |
| Stage 4 | Severe periodontitis | Over 50% attachment loss of the periodontium is present. This is visible on dental radiographs |
With effective treatment, gingivitis (stage 1) is a reversible condition (Figure 3). If calculus and a substantial amount of plaque is present, a professional dental cleaning is required to remove the calculus and plaque from the gingival margin and sulcus. This will provide pet owners with the opportunity to begin or restart effective dental home care. However, periodontitis (stage 2 or beyond) is generally not reversible without technically challenging periodontal surgical procedures. Tooth extraction is often appropriate in moderate-to-severe cases. Pavlica et al (2008) found small body size, breed signalment and increasing age are among the risk factors for periodontitis (Figure 4). General anaesthesia is required to allow dental procedures to be performed safely and effectively. Identification and treatment of pathology, effective cleaning of the gingival sulcus and protection of the patient's airway cannot be ensured without general anaesthesia. Position statements on the detrimental effects of non-anaesthesia dentistry (NAD) are available from leading veterinary dental organisations (European Veterinary Dental Society (EVDS), 2013; American Veterinary Dental College (AVDC), 2017) and, in the UK, the governing veterinary body provides regulation on this animal welfare issue (Royal College of Veterinary Surgeons (RCVS), 2014). The World Small Animal Veterinary Association Global dental guidelines also describe NAD as a major animal welfare concern (Niemiec et al, 2017).


The provision of an oral hygiene regimen is an important component following professional dental treatment. It is beneficial to assess an owner's willingness to provide dental home care prior to the procedure as this can impact the treatment plan. For example, an effective toothbrushing regimen following professional cleaning and treatment could reduce the future number of extractions in patients with mild-to-moderate periodontitis. If the owner is not motivated to implement home care, tooth extraction may be in the patient's best interest. The veterinary nurse can inform the veterinary surgeon of the owner's thoughts, helping them to make clinical decisions regarding treatment.
An oral hygiene regimen will not treat or reverse established periodontal disease or remove calculus. However, following professional treatment, it can prevent the condition from deteriorating so it is important for home care to begin soon after treatment (Figure 5). In many cases, it can increase the intervals between future dental procedures but will not prevent them altogether. Starting oral and dental care at the puppy and kitten stage can help prevent gingivitis by removing plaque and reducing calculus accumulation, keeping the oral cavity healthier for longer. Young animals will often readily accept toothbrushing, making it easier to establish than in adult animals.

Toothbrushing
Daily toothbrushing is considered the most effective measure for plaque and calculus reduction. Owner and patient compliance is the main factor in its success or failure. Research has demonstrated that for highly motivated cat and dog owners, compliance rates are approximately 40–50% after 6 months (Miller and Harvey, 1994; Theyse et al, 2003). Long term, this will be even less in the typical pet-owning population. If a correct technique is used, the mechanical action will disrupt plaque accumulation, which is likely the most important factor.
Many dentifrices (toothpastes) for dogs and cats contain either abrasive particles or active enzymes that claim to disrupt plaque accumulation (Figure 6). Their efficacy is questionable as brushing with a soft bristled brush and water alone has been shown to be just as effective (Tenuvuo et al, 2000). However, pastes and gels are given palatable flavours, which usually helps acceptance of tooth-brushing, allowing for the establishment of a good routine. Use of an anti-plaque gel with daily toothbrushing demonstrated a significant reduction in plaque at the gingival segment (Milella et al, 2014). It is also important to consider that pastes containing abrasive particles could cause gradual wear to tooth enamel. Toothpastes developed for human use are not safe for veterinary patients as they contain fluoride and foaming agents which are unsuitable for swallowing.

Toothbrushing should be performed frequently. Many veterinary dental professionals recommend daily toothbrushing so it becomes routine and optimal plaque removal is achieved. Harvey et al (2015) demonstrated that toothbrushing daily or every other day produced statistically improved results compared with brushing once weekly.
Due to the level of evidence to support the efficacy of toothbrushing, all other home-care options should be compared to this gold standard. However, it is not always an appropriate option owing to owner compliance and brushing technique issues, or reluctance from the animal towards accepting brushing. Therefore, other oral hygiene options should be considered in these cases despite them being best reserved as adjunctive methods. Oral hygiene wipes are another option available to owners who are reluctant to brush their pet's teeth. These wipes are impregnated with antimicrobial or plaque and calculus retarding properties such as chlorhexidine, zinc and sodium hexametaphosphate. Although not as effective as brushing they are beginning to be discussed anecdotally at veterinary dental conferences.
Chlorhexidine
Chlorhexidine gluconate 0.12% added to oral hygiene products in the form of toothpastes, gels and rinses provide effective antiseptic properties (Figure 7). They are particularly useful in patients suffering with gingivitis and stomatitis conditions, as they are particularly reactive to plaque and bacteria in the oral cavity. A short-term study of a chlorhexidine oral gel significantly reduced plaque accumulation; therefore, it may be beneficial at reducing gingivitis and associated periodontal disease if administered on a long-term basis (Hennet, 2002). A chlorhexidine rinse can be a useful immediate post-operative dental treatment following surgery as owners will be unable to implement toothbrushing, or feed dry food and chews until healing of the tooth extraction sites is complete.

Dental diets and nutrition
A complete, balanced diet appropriate to life stage is essential for the wellbeing of all cats and dogs. Therefore, providing pets with food that has added dental benefits seems a sensible option. The composition of an animal's food appears to have more impact on oral health than its nutritional content. It would be expected that feeding a wet food would allow for more plaque accumulation than a dry diet due to more sticky food debris in the mouth. However, some research suggests that there is little difference in plaque and calculus levels in dogs fed a standard dry food diet compared with those on a wet food diet (Harvey et al, 1996). However, a large study on dogs and cats performed by Gawor et al (2006) suggested the opposite effect; dental deposits and periodontal disease were significantly less when fed dried food compared with a mixed diet.
There are a number of complete and balanced ‘dental diets’ available on the pet food market and several have VOHC approval for calculus control (Figure 8). Most dry diet kibble will crumble easily during initial contact with the tooth surface, so they do not have the characteristics to perform adequate plaque removal. Dental diets have texturised kibble which prevent it from breaking down as easily, creating an abrasive action on the crown of the tooth. The combination of increased fibre content, kibble size and the patterned texture maximises contact with teeth, and promotes chewing to enhance plaque removal. A study demonstrated that diets with textured kibble can provide plaque and calculus control in cats when used after a professional dental cleaning. Research was carried out under controlled laboratory conditions but as use of a dental diet often begins after dental treatment, the circumstances are similar to those found in a clinical setting (Boyce, 1992).

The addition of polyphosphates such as hexametaphosphate (HMP) has varying results. HMP has been added to the surface of some diets and chews, as they bind to salivary calcium, helping to reduce calculus formation from residual plaque. There are several diets containing polyphosphates which have VOHC approval for calculus control; however, published studies have been performed over short-term periods and not demonstrated clinically significant results for plaque and gingivitis control (Warrick and Stookey, 2004). This suggests that although the teeth may appear clean, these diets may not be effective in controlling causative factors of periodontitis.
Dental diets have several limitations that may reduce their effectiveness, and will not be suitable for patients with health conditions that require other special diets. Large breed dogs, in particular, are prone to swallowing dry food whole; they may therefore not even chew the dental diets but the increased kibble size has been developed to combat this. However, dental diets are safe to use in the majority of cats and dogs, and are unlikely to cause trauma to teeth.
The majority of dental diets and dental products for consumption will be considered food stuffs. Therefore, they are subject to distribution regulations in each country such as those of the European Food Safety Authority or the Food Standards Agency in the UK. These ensure clear labelling of the contents and ingredients, hygiene during production, and assurance that they are safe for consumption.
Raw meaty bone diets
Credible data comparing the use of raw meaty bone (RMB) diets in comparison with commercially prepared diets and the impact raw diets have on dental health is lacking (van Veggel and Armstrong, 2017). Some owners choose to feed RMB and there is increasing popularity for fresh tailored diets which are safe for feeding and nutritionally balanced. Owners must be aware that bones, no matter the size, can be damaging to the teeth, soft tissues and alimentary system. In the United States, the Food and Drugs Administration (FDA) has released consumer information advising against feeding bones to pets (U.S. FDA, 2015). A small study found dogs fed an RMB diet had an increased incidence of dental fractures (Robinson and Gorrel, 1997). Harmful bacteria found in raw meat is also a concern as is the nutritional balance due to a lack of testing. Some relevant literature is available detailing the risks and benefits of using raw meat diets and the current understanding of these (Schlesinger and Joffe, 2011; Freeman et al, 2013).
Oral hygiene treats and chew toys
There are many oral hygiene chews and treats available on the pet product market (Figure 9). They are generally designed to reduce plaque or calculus accumulation through mechanical action. Some canine dental hygiene chews can reduce plaque, calculus and stain accumulation, as well as improve gingival health if given daily (Gorrel and Bierer, 1999; Quest, 2013). Ingham et al (2002) demonstrated similar findings in cats.

Some feline dental treats containing polyphosphates or enzymes claim to control calculus accumulation in cats. A small study demonstrated a reduction in dental substrate accumulation in cats fed an enzyme-coated chew (Warrick and Stookey, 2004). However, it is unclear if this due is to the abrasive action of the chew, the enzymatic activity or both.
A relatively new addition to the product market for dogs is a daily dental chew containing the chemical agent, delmopinol hydrochloride, to soften the plaque, disrupt the bacteria and reduce halitosis. The unique texture of the chew promotes removal of the dental substrates. As saliva dissolves the chew, the active agent coats the tooth's surface; this helps to form a preventative barrier against the plaque pellicle (www.oravet.com/Pages/about.aspx). The product has gained VOHC acceptance, and the product claims to reduce halitosis, plaque and calculus by approximately 50%.
Recommending dental chews and toys
When recommending dental chews or toys, their safety must be carefully considered. Owners should be advised to avoid anything which could potentially damage the teeth and mouth, or which could be dangerous if swallowed. Currently, there is no published research on the types of chews and toys that cause dental fractures or damage. However, it is sensible to recommend only using products that can be pitted with a thumb nail and are easily flexed by hand, such as rubber balls, or rubber bones and safe sticks.
In the author's experience, products such as nylon and antler-type chews are responsible for a high incidence of dental fractures in dogs (Figure 10). The British Veterinary Dental Association (BVDA) released a position statement after a notable increase in the popularity of antler chews (BVDA, 2017). Dried red deer antlers need considerably more force than wet bone to bend or fracture (Currey et al, 2009). This suggests that a tooth would become damaged before an antler chew. Tennis balls also cause chronic abrasion wear (Figure 11) which, over time, can lead to pulp exposure. Tug-of-war play with frisbees and rope tug toys can result in non-vital teeth and pulp necrosis.


Water additives and rinses
Water additives are a relatively new addition to the veterinary dental market and most claim to benefit oral hygiene by reducing plaque accumulation. One company has achieved VOHC seals for plaque reduction for its feline and canine product range of water additives, oral gels, and rinses. The products contain human-grade naturally derived ingredients, and papain enzymes reduce the accumulation of salivary glycoproteins. The addition of zinc acts as an antimicrobial agent. The manufacturer's clinical trials suggest that it retards plaque and softens the plaque already established, making removal easier (Healthymouth, 2017a, b).
Some water additives contain xylitol, a sugar derivative from hardwood trees. It is known to have an antimicrobial effect and help prevent dental caries (tooth decay) in humans, and other studies have suggested it can reduce dental substrates. A study by Clarke (2006) found that a xylitol containing water additive provided an effective reduction in plaque and calculus accumulation in cats. During the study the drinking water was treated with 0.005% each day. Xylitol is a known toxin if consumed in large quantities and products containing 100% xylitol should be of concern to pet owners. The small amount contained in water additives is unharmful. However, the accumulative effects of xylitol are unknown. The Veterinary Poisons Information Service provides current information on this (www.vpisglobal.com).
Conclusion
There are several factors to consider when helping owners with the selection of an oral hygiene option for their pets. Owner motivation and the animal's temperament will determine if toothbrushing is possible, and some owners might be physically unable to brush their pet's teeth. There is considerable evidence to support the efficacy of toothbrushing but the results seen in clinical practice vary, mainly as a result of compliance issues. A tier system could be adopted for advising owners on an oral hygiene regimen; factors such as the owner's willingness, time and financial situation, as well as the pet's demeanour and general and oral health status, will all impact product selection.
Some dental diets and treated chews can reduce either plaque and/or calculus accumulation. They can be beneficial in helping to maintain oral health, and could be used in addition to toothbrushing, or as a poorer alternative. The calorie content of dental chews and diets is of concern to many veterinary professionals, and with the prevalence of obesity in the canine and feline population, this factor needs to be carefully considered. Reducing daily caloric intake to factor in the addition of a dental treat chew or diet, and weighing the animal at their review appointments will help to monitor this.
The safety of a product is as important as its efficacy. Published research on the effects of bones in the diet or hard chews would be beneficial to support the anecdotal consensus that they are harmful. Periodontitis cannot be resolved with home care alone and professional treatment will always be required in these cases. It is important to note that the RCVS (2014) requires dental procedures to be performed under a full general anaesthetic with endotracheal intubation. Veterinary nurses can be advocates for veterinary oral health care in practice, helping to develop homecare protocols and supporting owners while implementing oral hygiene care.

