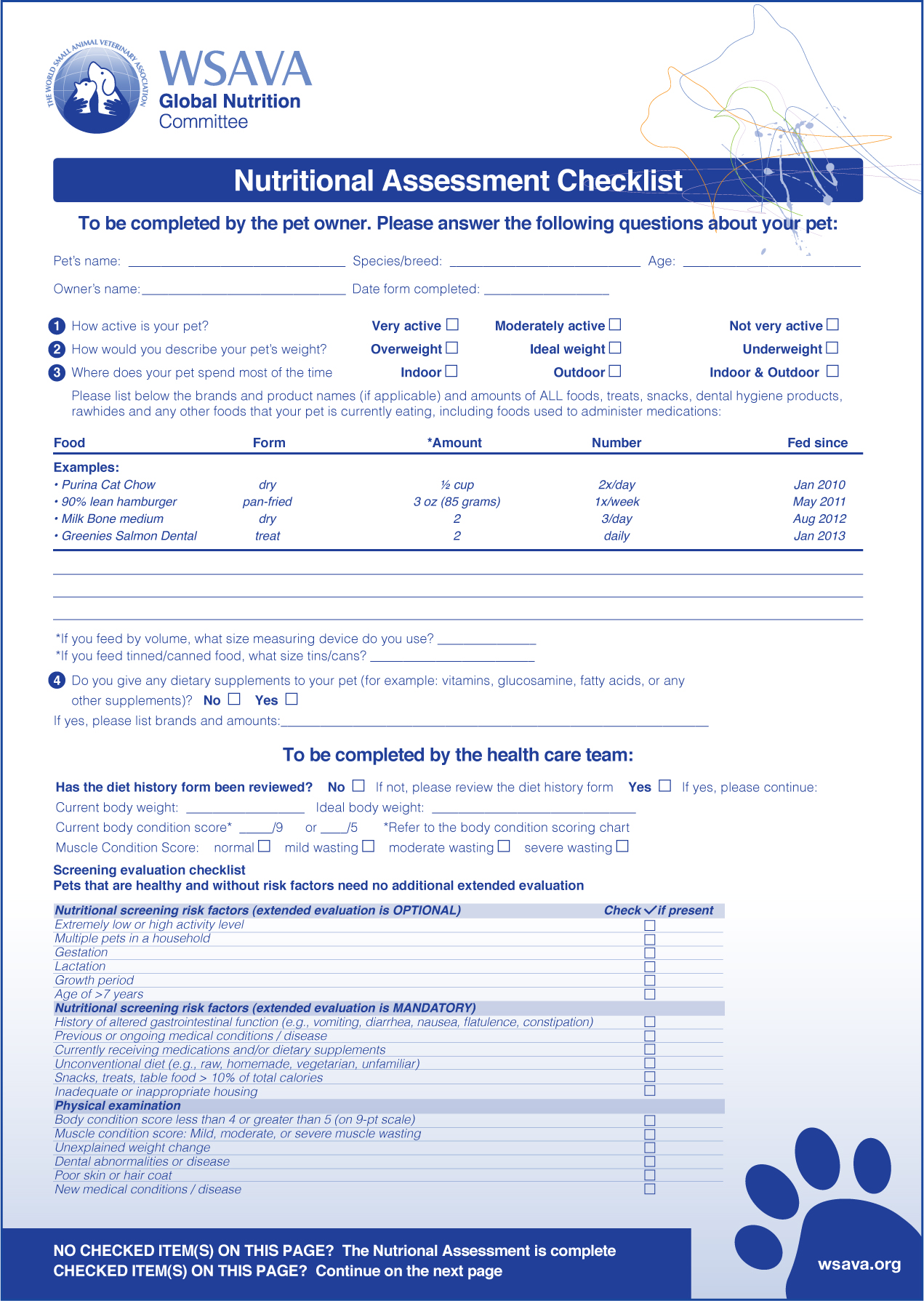
The World Small Animal Veterinary Association (WSAVA) nutritional guidelines recommend including nutritional assessment into the five vital signs of patient assessment, along-side temperature, pulse, respiration and pain (Freeman et al, 2011). Nutritional assessment involves a multi-faceted approach, including duration of anorexia/hyporexia, ability to eat voluntarily, body and muscle condition scoring and risk factors. See Figure 1 for a downloadable checklist available from the WSAVA. Nutrition is often in the back of veterinary professionals' minds with many patients, not only critical patients. While they carry out stabilisation and investigations into the patient's current condition and presentation, they will rigorously investigate inappetence and treat the underlying cause, but implementing a nutritional plan and methods of assisted feeding generally comes much later.
What is nutrition and why is it important
Nutrition is described as the processes of food utilisation by a plant or animal (Merriam-Webster, 2020). The terms macro and micronutrients refer to the volume of each that is required. Macronutrients include protein, carbohydrates and fats, and they are predominantly responsible for energy provision. Protein is responsible for metabolic regulation, tissue growth, function and repair; carbohydrates are mostly converted to glucose and used for energy; fatty acids omega-3 and omega-6 are essential and significant in immunosuppression and inflammation (McCune and Girling, 2007). Micronutrients are the vitamins and minerals required to maintain healthy function and immunity; minerals are often collectively known as ash.
Malnutrition
Simple starvation is described as the absence of nutrition in the otherwise healthy animal, and involves the utilisation of glycogen stores to meet energy requirements (Chan and Freeman, 2006; Chan, 2013). Stressed starvation is the term used to describe a metabolic response to trauma, inflammation or disease triggering changes in cytokine and hormone concentrations leading to catabolism of lean muscle and preservation of fat stores in the absence of adequate nutrition (Chan and Freeman, 2006; Chan, 2013). Catabolism of muscle is more pronounced in cats, as glycogen stores are rapidly depleted in the strict carnivore, and as gluconeogenesis is a constant process in cats, amino acids (specifically alanine and glutamine) are mobilised early from muscle stores to fuel enterocytes and macrophages in the immune system (Saker, 2006; Chan, 2013). Starvation will also result in gastrointestinal (GI) mucosal atrophy and subsequent increase in permeability (Sigalet et al, 2004).
Illness in many forms induces biochemical, metabolic and pathological abnormalities which influence nutrient use (Saker, 2006). The term critically ill could refer to instabilities of the cardiovascular, respiratory or neurological systems, or any patient experiencing hypermetabolic derangements. Chan (2013) states that critically ill patients or those recovering from surgery are often reluctant or unable to ingest adequate nutrition, and with an increased nutritional demand as a result of metabolic changes they are at an increased risk of malnutrition. Protein-calorie malnutrition (PCM) is associated with reduced production of immunoglobulins, secretory antibodies and complement components, as well as atrophy of the thymus and lymphoid tissue, atrophy of the skin and GI mucosa, neutropenia, reduced neutrophil function and subsequent reduction in the capacity to neutralise phagocytosed bacteria (Saker, 2006). Compromised immunity is detectable in cats by day 4 of anorexia, and metabolic changes in dogs by day 3, therefore it is argued that nutritional support should be implemented by day 3 (Chan, 2013). Often the period of anorexia at home is disregarded, and nutrition is implemented on day 3 of hospitalisation, but this can be day 6 of anorexia for the patient and close attention should be paid to the patient's history. Hyporexia (reduction in appetite) should also be considered, as inadequate nutritional intake may result in the same complications, such as infection, sepsis, organ failure and poor wound healing (Saker, 2006).
When to implement nutrition in critical care
Cardiovascular, respiratory, urogenital and neurological stability will always require priority attention in emergency and critical care medicine, however implementation of nutrition is often overlooked once stability is achieved. In any kind of malperfusion associated with unstable presentation, splanchnic perfusion will be compromised, and feeding the patient in this unstable condition could increase the risk of intestinal ischaemia (Sigalet et al, 2004). Nutrition should be implemented as soon as possible after restoring haemodynamic stability, electrolyte and acid–base disturbances, and hydration status (Delaney, 2006; Chan, 2013).
In some diseases, it has been the historical approach to starve the patient on purpose, this view was also seen in human medicine in the care of the elderly (Chan, 2013). In human medicine, however, the effects of malnutrition were found to have an impact on morbidity and mortality, and implementation of nutrition was prioritised (Chan, 2013). Veterinary medicine has been delayed in following this approach, and it is not unheard of to see the parvoviral puppy starved early in its care, as well as patients with haemorrhagic gastroenteritis or pancreatitis, in favour of emptying the stomach to allow rest time. Mohr et al (2003) reported several studies highlighting the occurrence of bacteraemia in canine parvovirus, considered likely as a result of the breakdown of gut barrier function leading to bacterial translocation. The small bowel contains gut associated lymphoid tissue (GALT) with lymphocytes and macrophages on the intestinal wall (Saker, 2006). This, alongside immunoglobulins secreted into the GI lumen minimises pathological translocation. Translocation is promoted by bacterial overgrowth, impaired defences, protein-calorie malnutrition, trauma, critical illness and mucosal atrophy, as well as a change in luminal nutritional supply (Saker, 2006). In a review of several studies in human medicine Sigalet et al (2004) found that the implications of starvation included mucosal atrophy and increased intestinal permeability. A study by Hadfield et al (1995) found that implementation of enteral nutrition can reverse the impairment to GI tract mucosal lining associated with critical illness in humans. Historically treating pancreatitis with starvation has been a common approach considered necessary in order to rest the pancreas and avoid autodigestion; however, this theory is not proven, and studies have in fact suggested little to no negative feedback from the pancreas in the presence of nutrition in the intestinal tract (Harris et al, 2017). A study by Harris et al (2017) found reduced GI intolerances (defined in the study as vomiting and regurgitation) when enteral feeding was implemented within 48 hours of admission, compared with delayed nutrition. This study also found early assisted feeding reduced the time to voluntary feeding, and any GI intolerances seen were predominantly in the non-assisted feed period.
Some patients are at an increased risk of delayed nutrition, such as obese cats at risk of hepatic lipidosis, a condition where cats mobilise peripheral fat stores in the absence of food and hepatocytes overwhelm with triglycerides, or young growing animals (Chan, 2013). Conversely, recumbent patients, or those with obtunded mentation, are at risk of aspiration where there is risk of regurgitation, such as if fed orally or by upper GI feeding tubes. Patients with ileus are at an increased risk for feeding complications, as are patients on systemic opioids and anaesthetised patients, such as ventilated patients (Chan, 2013). Pain should be assessed as a painful patient is unlikely to eat voluntarily regardless of the underlying condition; however, opioids can slow gut motility and exacerbate anorexia (Delaney, 2006). Alternative analgesic options should be considered, such as multi-modal analgesia, and constant rate infusion (CRI) combinations that can facilitate decreased bolus opiate doses.
How to implement nutrition
Enteral vs parenteral
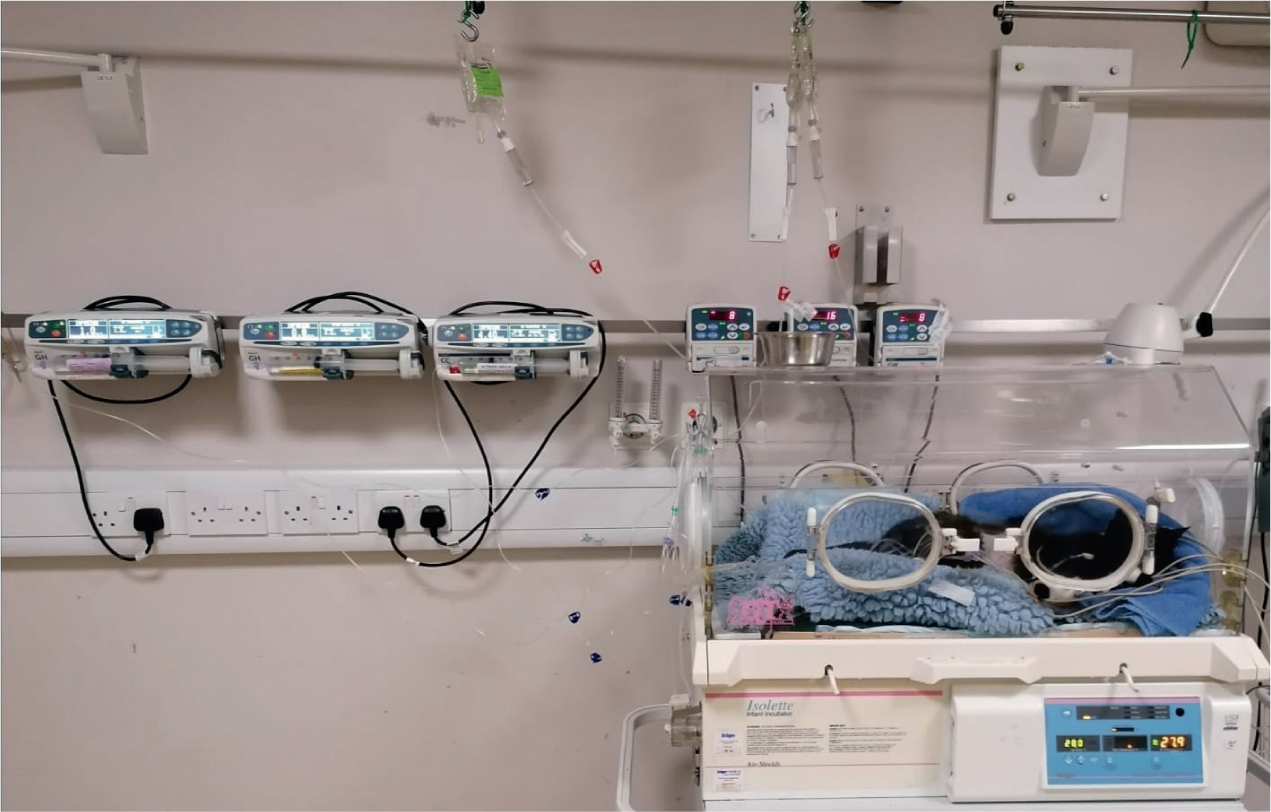
Parenteral nutrition (PN) is the administration of nutrition intravenously via a central catheter, or intraosseous catheter in neonates or very small patients. PN should only be chosen if there is an inability to feed enterally or if the patient is at an increased risk of aspiration, such as depressed mentation (Michel and Eirmann, 2015). It can be used to supplement enteral nutrition if the patient is unable to meet 50% of its requirement via the digestive tract, a method that has proven successful in improving outcome in small animals (Freeman et al, 2011; Chan, 2013; Michel and Eirmann, 2015). There are now PN bags commercially available containing amino acids, dextrose, electrolytes and lipids (Kabiven, Fresenius Kabi). There are many complications associated with PN including but not limited to: thrombophlebitis because of hyperosmolarity (therefore use should be limited to a central line); hyperglycaemia; hypertriglyceridaemia; hyperammonaemia (Chan, 2013). The catheter (or central venous port) and line used should be handled aseptically, and dedicated to the PN only, as there is an increased risk of sepsis (Michel and Eirmann, 2015). In the author's practice, PN is prepared with sterile gloves and the ports and connections are sealed with tape to avoid accidental disconnection and prevent use for sampling or medications. PN adversely affects immunoglobulins in GALT, but also affects mucosal affected lymphoid tissue such as found in the respiratory system (Sigalet et al, 2004).
Enteral nutrition is important in maintaining the enteral immune barrier (Sigalet et al, 2004). Sigalet et al (2004) reviewed many studies in human medicine on enteral nutrition versus PN in surgical and trauma patients, and found that overall patients receiving PN were more likely to develop significant infections, and that enteral feeding reduced not only the risk of infection, but also the length of hospitalisation and mortality.
Tube options
Assisted feeding should be implemented if the patient is not voluntarily meeting 75% of its resting energy requirements (RER) (Freeman et al, 2011; Chan, 2013). There are many components to tube selection, such as anticipated duration of support, disease affecting the alimentary tract, cost and whether or not anaesthesia or sedation is required. Feeding tubes allow the opportunity to administer feed by CRI. This may be preferred if the patient is not tolerating large volumes in the stomach, or if the patient has a jejunostomy tube, where bolus feeds are not tolerated (Chan, 2013). There are many tube options, such as naso-oesophageal (NO), naso-gastric (NG), oesophagostomy, jejunostomy and percutaneous endoscopic gastrostomy (PEG) (Figure 2). The advantages and disadvantages of each method should be considered.

Tube placement should be confirmed by aspiration of gastric content, or imaging, preferably radiographic. An alternative tube placement check uses capnography — placement into the airway will cause a capnograph trace and reading, placement into the alimentary tract should not give any capnographic reading and thus can be used as confirmation of correct placement.
Patients can be discharged with feeding tubes indwelling for management at home (Eirmann and Michel, 2015). This should also be considered in tube choices, as NO or NG tubes are generally not suitable for long-term use because of patient interference and tube blockage. To avoid the risk of confusion between enteral feeding ports and central line ports, there are commercially available connectors and tubing reversing the male-female connection (Nutrisafe, Vygon), therefore feeding lines cannot be accidentally connected to a venous port. Alternatively and additionally, feeding lines and ports should be clearly labelled to avoid any mishaps. This is particularly pertinent where there are concurrent O tubes and central venous catheters, as the insertion sites are wrapped in the same neck dressing.
Resting energy requirements
Canine and feline adults
Canine and feline adults Nutritional requirement is calculated as a resting energy requirement (RER), as the calories required per day to maintain homeostasis in a thermoneutral environment (Eirmann and Michel, 2015). Any energetic exertion would increase the requirement, such as in a working dog. Historically, illness factors were used to increase the calorific calculation, with a range of 1.0-1.5 x RER to account for increases in metabolic demand associated with disease and wound healing. This method is less favoured now because of the risk of overfeeding, which is associated with complications such as gastrointestinal intolerance, hepatic dysfunction, increased carbon dioxide production and hyperglycaemia, among other metabolic complications (Chan, 2013). Instead, the recommendation is to feed the calculated RER and monitor the patient for signs of inadequate intake, increasing in increments of 25% per 24 hours as required (Chan, 2013). This method may well exceed 100% of the calculated RER; in the author's experience, it is common to feed 200% and more to tetanic patients with a markedly increased metabolic demand. If the patient is not tolerating the quantities of food required, then supplementation with PN should be considered. Despite the guidelines of feeding the standard RER, some disease processes are expected to exceed these requirements, such as thermal burns or tetanus.
While aiming to achieve 100% RER intake, this can be achieved gradually over 3 days, starting at approximately 30% RER. This method may be preferable in patients with prolonged anorexia, metabolic instabilities and GI disease, and is subject to daily reassessment (Eirmann and Michel, 2015). Nutrition specific monitoring charts are available from the WSAVA (Figure 3).
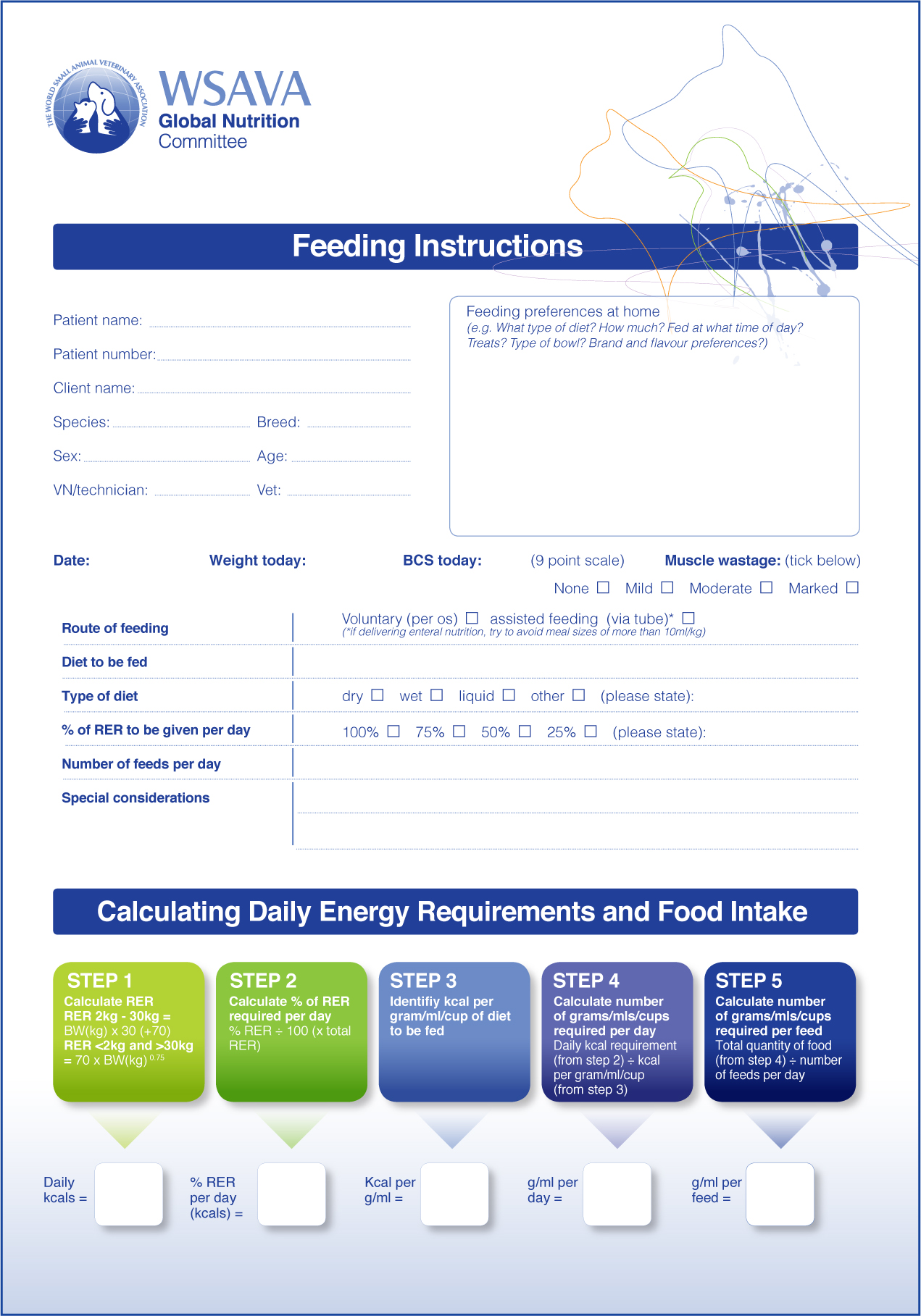
The RER can be calculated using:
Bodyweight (BW) <2 kg or >30 kg
RER = 70 x BW0.75 = k/cal per 24 hours
BW 2–30 kg
RER = (30 x BW [kg]) + 70 = k/cal per 24 hours
Young canines and felines
Hospitalised growing puppies and kittens should initially be fed the percentage of RER they will tolerate, aiming for 100%, subject to frequent reassessment. Regular assessment should determine early if the patient has an increased calorie demand and the patient should be fed to meet this (Eirmann and Michel, 2015). Growing animals are at an increased risk of hypoglycaemia if nutrition is delayed.
Considerations in hospital
Nutritional assessment, according to the WSAVA and American Animal Hospital Association (AAHA) guidelines should include environmental factors, such as location, environmental stimulation and surroundings, as these are all factors that may impact the likelihood of a patient eating in the hospital environment, and at home (Baldwin et al, 2010; Freeman et al, 2011). Other considerations should include feed timings and frequency, method of feeding and poor husbandry (Baldwin et al, 2010; Freeman et al, 2011). For example, a food bowl next to a soiled litter tray is unlikely to stimulate the appetite of a hyporexic cat (Delaney, 2006). Similarly, grooming the patient if they enjoy it, or otherwise simply fussing them, may encourage eating, or the inclusion of feeding toys may stimulate interest in food (Baldwin et al, 2010; Freeman et al, 2011). Raised feed bowls should be considered for cats as well as large breed dogs. Attention should be paid to the environment: an anorexic cat is unlikely to begin eating in the presence of a noisy dog (Delaney, 2006). A patient assessment questionnaire may be useful in determining normal feeding routines, such as bowl type and environments, favourite food types and flavours. An anorexic dog may prefer to eat in the clinic kitchen area than its own kennel, as it more closely mimics a home environment. The patient may be more inclined to eat if it is fed by someone it does not associate with stress, therefore the person that examines, restrains and carries out procedures most often on the patient may incite an aversion to that meal and may not be the best person to feed that patient (Delaney, 2006).
Chan (2013) suggests that strategies such as warming foods and flavour enhancers are typically ineffective, and that syringe or force feeding should not be used. Syringe feeding is a high risk for aspiration and can induce food aversion (Freeman et al, 2011), as well as being difficult to accurately record due to spillage with poor patient cooperation. Other commonly used tempting strategies include using wet foods, high fat and high protein diets (Delaney, 2006).
Monitoring and complications
Patients should be assessed daily to see if they are receiving the prescribed RER voluntarily, and if they are being supported sufficiently by tube, or if they require intervention (Eirmann and Michel, 2015). A study by Brunetto et al (2010) found a direct association between patients fed <33% RER and a poor hospital discharge rate. All hospitalised patients should be weighed daily, particularly patients receiving nutritional support (Chan, 2013). Weight changes should be assessed alongside other clinical parameters, such as fluid balance; body condition scoring (BCS) may help distinguish changes between the two (Chan, 2013). BCS is commonly seen and used in practice, using a visual comparison of waist, neck and shoulder width and abdominal tuck, as well as palpation of fat cover over the ribs, spine and pelvic bones (Freeman et al, 2011). Muscle condition scoring (MCS) systems are less well known. These involve palpation of bony areas which should have adequate muscular cover, such as the temporal bones, vertebrae and pelvis, and is scored as mild, moderate or marked muscle wasting (Freeman et al, 2011). WSAVA recommendations are to use MCS in chronic and acute disease, as muscle loss is greater in patients with stressed starvation (Freeman et al, 2011). A study by Michel et al (2011) validated the use of a palpable four point muscle mass scoring system in cats. It found differentiating between normal and severe muscle wasting accurate when compared with dual-energy x-ray absorptiometry, but that determining mild to moderate wasting was less reproducible. Regular monitoring should also include blood tests such as glucose, total solids, triglycerides, blood urea nitrogen and electrolytes to assess the effects of nutritional intervention, both positive and negative (Eirmann and Michel, 2015).
Refeeding syndrome is a complication whereby a malnourished patient undergoes metabolic derangements on implementation of feeding, resulting in depletion of phosphorus, magnesium and potassium, which can lead to cardiac arrhythmias and respiratory failure (Chan, 2015). This complication is generally associated with prolonged starvation and severely malnourished patients. Regular monitoring of bodyweight, urine output and electrolytes should be carried out in all patients with recently implemented nutritional support, specifically patients identified as at increased risk, and particularly cats (Figure 4).
Other complications associated with assisted enteral nutrition include GI intolerances, such as vomiting, diarrhoea and abdominal pain (Chan, 2013).
Conclusion
A nutritional plan should be made for every patient. Nutritional assessment on admission should highlight areas of concern, and the requirement for restricted calorie intake, restricted diet factors and interventions that may be required, with a rigid timeframe. The latest guidelines advocate early enteral nutrition where feasible, with parenteral nutritional support as required.
Patient assessment questionnaires can be helpful in determining patient preferences, such as favourite flavours, food bowl types and normal environment, however this is not a requirement. Developing a calorie cheat sheet with the caloric value of each commonly used diet and tempt food helps to quantify exactly how much of the patient's RER they are achieving voluntarily, otherwise hyporexia can be easily missed. Hospitalised human patients fed enterally rather than parenterally were found to often be significantly underfed, a risk that the veterinary nurse should be aware of (Sigalet et al, 2004). Nutrition-specific monitoring charts are available from the WSAVA and can play a pivotal role in early identification of inadequate nutritional intake, allowing prompt intervention.
KEY POINTS
- Early enteral nutrition is recommended as soon as the patient is stable.
- Parenteral nutrition is an option for patients that cannot tolerate enteral nutrition, or need extra support.
- Feeding tubes are advocated for patients that are not voluntarily eating a sufficient amount.
- Nutrition plays an important role in wound healing, immunity and health.


