The patient presented with a history of rapid weight loss and lethargy. He was reported to have had hyporexia, progressing to anorexia over the past 5 to 7 days. The owner described his demeanour as poor and perceived him to be uninterested in his surroundings. He was fully vaccinated and had no previous clinical complaints.
Signalment
- Species: Canine
- Breed: Dogue De Bordeaux
- Age: 8 years 9 months
- Sex: Neutered male
- Weight: 45.05 kg
Patient assessment
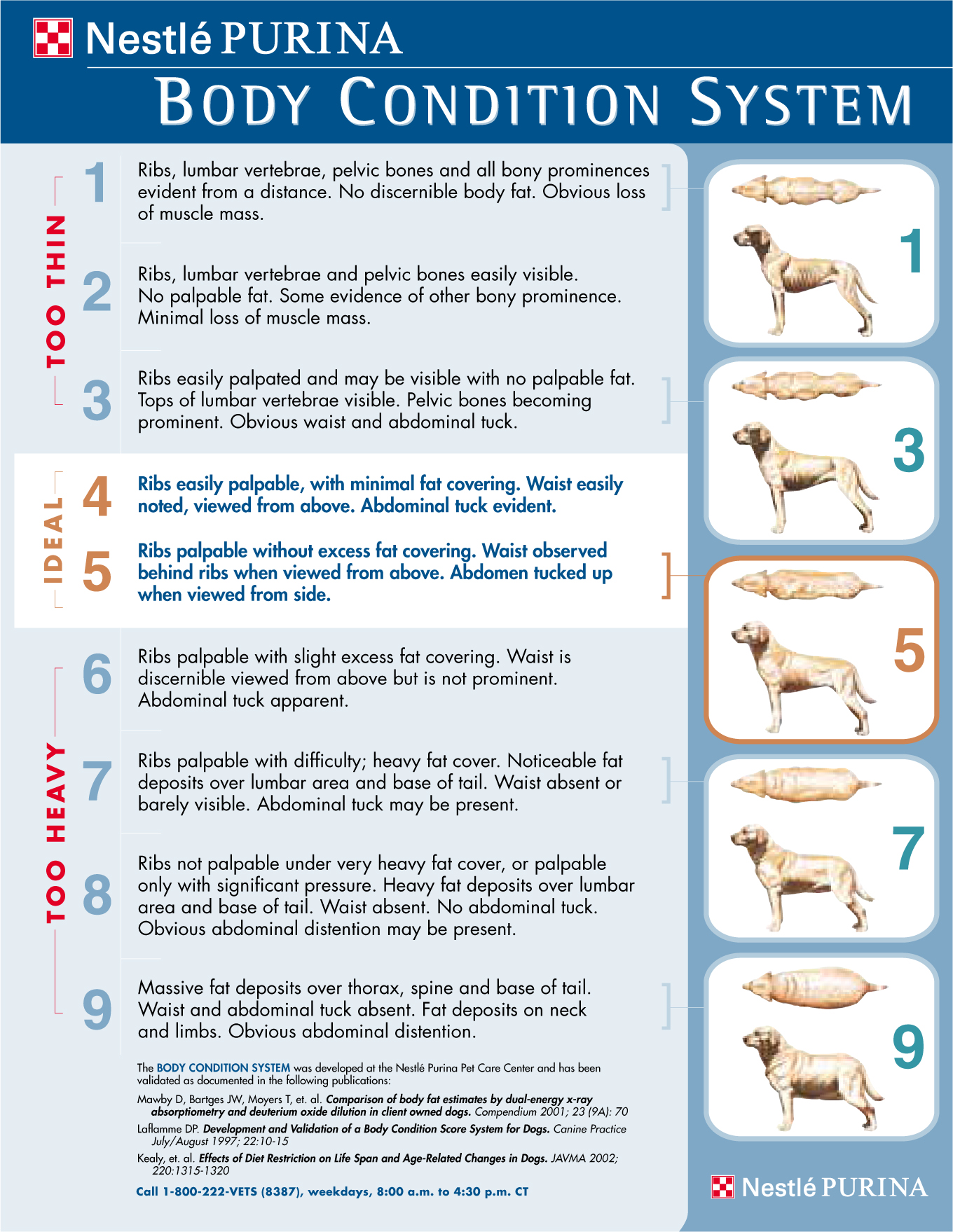
The patient had pale, tacky mucus membranes (MM) and a capillary refill time of 1–2 seconds. He had a heart rate (HR) of 224 beats per minute (bpm), with an irregular rhythm and weak peripheral pulses. He had no audible heart murmur and no pulse deficits. His respiratory rate (RR) was 30 breaths per minute (brpm) and mild audible crackles could be heard over his lung fields. He had moderately increased respiratory effort and a distended abdomen. His body condition score (BCS) was 2/9.
Initial treatment and diagnostics
Due to the presenting clinical signs of cardiovascular and respiratory compromise, congestive heart failure (CHF) was a potential differential diagnosis for this patient. CHF is characterised by clinical signs of increased tissue water retention and/or decreased tissue perfusion caused by heart disease (Jenkins and Pace, 2012).
Patients with CHF are at risk of rapid deterioration (Ware, 2014a). Therefore, oxygen was supplemented via nasal prongs immediately. On admission the patient was stable enough for an intravenous (IV) catheter to be placed by the veterinary nurse (VN), to facilitate emergency drug administration. The veterinary surgeon requested 5 mg/kg furosemide (Dimazon 5%, MSD, UK), a fast acting and potent diuretic (Pace, 2011), to be administered intravenously.
It should be noted that IV catheter placement is not always feasible in these patients as this procedure can sometimes induce stress. An increase in stress and anxiety in animals with heart failure could cause life threatening arrhythmias (Pace, 2011) and so care should be taken not to further agitate these already compromised patients. With this in mind, other routes of drug administration such as intramuscular (IM) or subcutaneous could be considered (Pace, 2011).
The patient was taken to a quiet area, in an attempt to keep him calm and he was allowed to acclimatise himself to his surroundings. As advised by Pace (2011) monitoring of his RR and respiratory effort was carried out by the VN from a distance, as excessive handling could escalate anxiety, exacerbating clinical signs. After approximately 1 hour indications of respiratory improvements were observed (i.e. RR reduced to 10–20 brpm, respiratory effort and abnormal lung sounds, such as crackles, reduced) and diagnostic evaluation was initiated.
A blood sample was collected from the cephalic vein to ascertain biochemical and haematological values, these revealed no abnormalities. At the time of writing, the author's previous practice did not have the facility to run blood gas analysis. This would have been useful to ascertain, as it is the ‘gold standard’ for assessing both ventilation and oxygenation by measuring both gaseous exchange and pulmonary function (Miller, 2007; Nelson, 2015).
Echocardiography revealed generalised atrial and ventricular dilation and reduced ventricular contractility. Abdominal ultrasonography confirmed ascites. An initial electrocardiogram (ECG) recorded a HR of 217–242 bpm and atrial fibrillation (AF) (Figure 1). Clinical presentation and diagnostic findings led to a diagnosis of left- and right-sided CHF, secondary to dilated cardiomyopathy (DCM).

Case discussion
DCM is characterised by rounded, poorly contracting ventricles, with or without arrhythmias (Ware, 2014a). DCM is the most common form of acquired myocardial disease in dogs (O'Grady et al, 2008; Jenkins and Pace, 2012; Pace, 2014; Pace, 2016) and is most prevalent in large and giant breeds (Martin et al, 2009; Ware, 2014a). It is a progressive disease characterised by two phases: a pre-clinical phase (no clinical signs seen, but myocardial or electrical abnormalities present), and an overt clinical phase (clinical signs develop) (Dukes-McEwan et al, 2003; Oyama, 2008). It could be said that this patient presented in the overt clinical phase of DCM.
When the overt clinical phase of DCM is diagnosed clinical findings are often severe and sudden death is common (Oyama, 2008). The exact aetiology of DCM is unknown and the prognosis for dogs with CHF as a result of DCM is reportedly guarded (Monnet et al, 1995, Martin et al, 2009). A study by Martin et al (2009) showed that out of 369 dogs that were referred with clinical signs or a clinical abnormality, 65% of them presented in advanced heart failure (based on the recommendations of the International Small Animal Cardiac Health Council, 1999). Martin et al (2009) found that the mean survival time for these dogs was only 19 weeks following diagnosis and management of DCM.
Medical management
After diagnostic procedures had been completed, the veterinary surgeon instructed the administration of IV furosemide to stop and be replaced with 60 mg oral furosemide tablets twice daily. Pimobendan (Cardisure®, Dechra, UK), which has positive inotropic and vasodilatory effects (Pace, 2011), was prescribed orally, every 12 hours.
Spironalactone (Prilactone®, Ceva, Bucks), an aldosterone inhibitor and weak potassium sparing diuretic, was administered orally, once daily. This was prescribed because of its neuroinhibitory effects on aldosterone, helping to reduce sodium and water retention, and also countering potential potassium loss due to furosemide therapy (Pace, 2011). As the ECG (Figure 1) had recorded AF in this patient, digoxin (Digoxin, Actavis, UK), which slows the HR when supraventricular arrhythmias (such as AF) are present, (Ware, 2014b) was prescribed orally, twice daily.
Pace (2011) suggests that by knowing the action of drug therapy VNs can gain an understanding of the pathophysiology of heart disease/failure and be aware of the potential side effects that may occur. For example, digoxin can cause life-threatening arrhythmias and neurological symptoms to develop. It is therefore recommended that biochemistry, electrolyte and urinalysis tests are evaluated every month until the patient is stable, then reduced to testing every 3–6 months (Idexx, 2014). Monitoring of digoxin serum levels every 14 days is also necessary until patient stability is achieved, and then every 3–6 months thereafter (Idexx, 2014).
In conjunction with this it is important for VNs to consider routes of administration and to ensure that the medications are given correctly and on time (Pace, 2011).
As previously stated, stress reduction is an important objective of nursing care for patients with CHF (Pace, 2011). Oral administration of medications could have induced stress, compromising the patient, thus causing detrimental effects to the cardiorespiratory system. As there are other formulations of the above drugs, it may have been more beneficial to the patient to continue with these medications via IV or IM routes.
Nutritional considerations
Nutritional therapy for cardiac patients can be difficult as recommendations can vary (Jenkins and Pace, 2012). Nutrients considered important in the dietary management of cardiac patients include protein, sodium, fat, potassium and magnesium. Antioxidant supplements, such as of n-3 fatty acids or coenzyme Q10, are used due to their anti-inflammatory, antioxidant and cardioprotective effects (Jenkins and Pace, 2012). Other supplements including taurine and lcarnitine are also commonly added to cardiac diets. However, it should be noted that supplements can be expensive and their full effects are not yet known (Freeman et al, 2006).
Jenkins and Pace (2012) suggest that sufficient amounts of good quality protein are essential for the cardiac patient. This notion is supported by Ware (2014b) who also advocates maintaining good quality dietary protein and adequate calorie intake. During heart failure, hormonal messages tell the kidneys to retain sodium. Therefore, salt restriction in the diet can help control fluid accumulation and reduce the necessity for drug therapy (Ware, 2014b). However, very low dietary salt levels can increase activation of the renin-angiotensin-aldosterone system. Therefore, in clinical heart failure only moderate sodium restriction is advised (Ware, 2014b).
Due to his inappetance, the VN tried to encourage eating by offering a variety of food types simultaneously. On reflection this may not have been beneficial. Delaney (2006) warns that anorexic patients should not be offered a variety of food due to the risk of inducing food aversions. It is suggested that small quantities of the same diet should be offered several times a day (Lumbis, 2012).
Warmed food was offered to this patient, which is a technique supported by Case et al (2011) and Ware (2014b). However, when the food was not eaten it was removed without any other attempts to encourage eating. Lumbis (2012) suggests coax feeding or feeding in a different area of the practice as a way to tempt the patient.
Lumbis (2012) also suggests that good communication with the owner, regarding the patient's normal eating habits, could allow the VN to re-create normal routines thus improving the response to food. The VN did request that the owner bring in the patient's normal diet in an attempt to improve appetite. The patient ate a very small amount of this diet but then refused any further offerings. Two days after admission the patient's appetite developed. The patient took to eating Hills® Vet Essentials Puppy Large Breed diet, which was offered as part of the variety of foods readily available at the clinic.
Retrospectively the diet accepted by the patient was not cardiac specific. Its nutritional contents consisted of 30% protein and 0.45% sodium as well as potassium, magnesium, omega-3 fatty acids and l-carnitine. In comparison, Hills® H-D Canine Cardiac Health Prescription Diet contains 18.5% protein, taurine, potassium, B vitamins, magnesium and l-carnitine, and much lower sodium content (0.08%). However, this diet was not readily available. In keeping with the previously discussed nutritional needs of a cardiac patient, Hills® Vet Essentials Puppy Large Breed had high protein and moderate sodium content, while providing additional supplements. Therefore, it may have actually been an acceptable choice for this cardiac patient.
At the time of writing, no standardised protocol for planning the nutritional requirements of a patient existed in the author's previous clinic. It has been documented that, in general, poor feeding practice is a common occurrence in small animal practice (Remillard et al, 2001; Michel and Higgins, 2006). This is an area that the VN could be greatly involved in to help make improvements. Simple steps such as ensuring a range of prescription diets is kept in the practice could help improve the nutritional needs of their patients.
When the patient presented to the clinic an initial weight was recorded and his BCS was identified as being 2/9 (using a BCS system where 1 is severely underweight and 9 is severely obese (Figure 2)). He also had a distinct loss of fat and overall muscle mass which are characteristics of cachexia. It is important to be aware of this as cachexia has been related to the poor prognosis in CHF patients (Slupe et al, 2008; Freeman, 2012; Freeman and Rush, 2012).
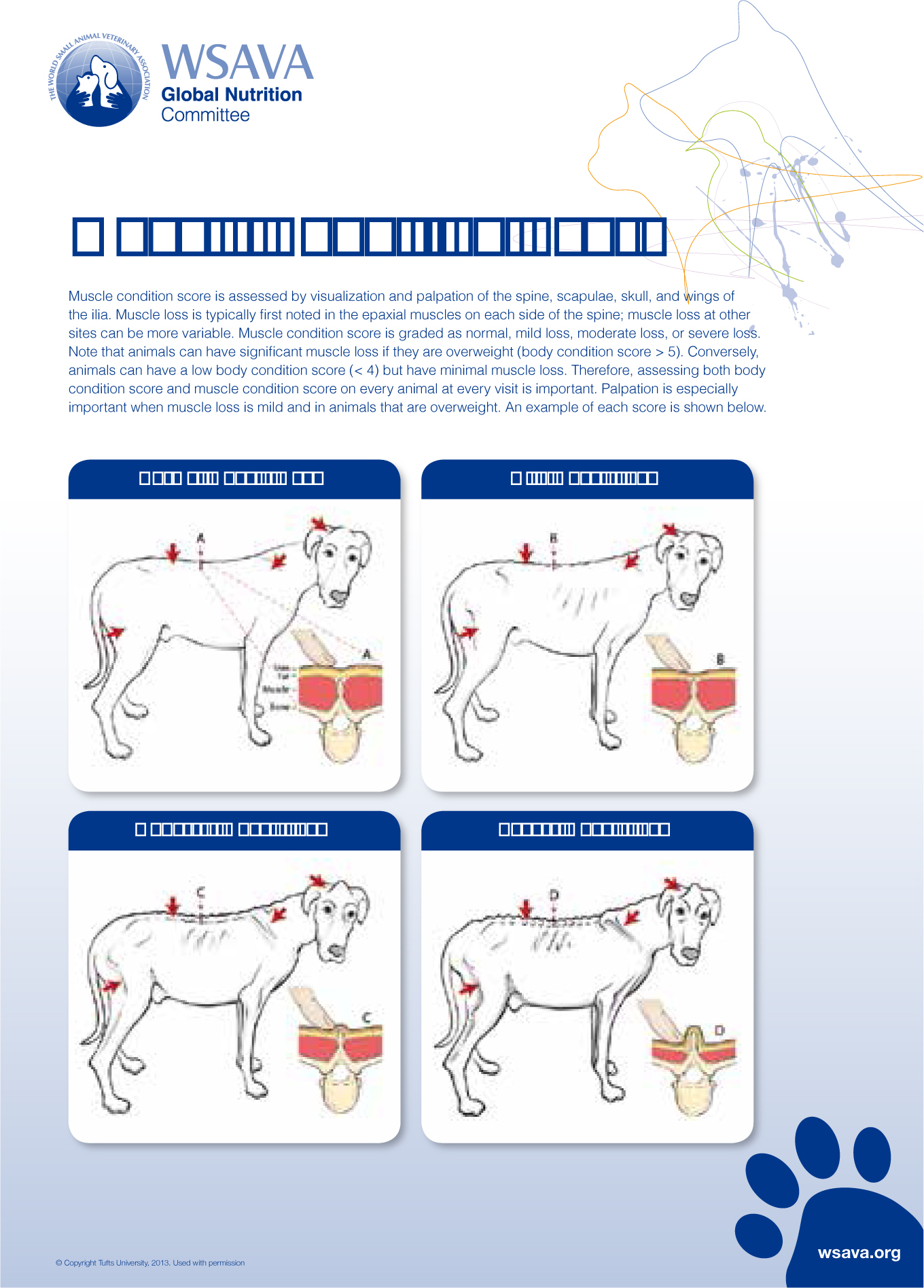
Reference to the patient's muscle loss was not recorded. This could be due to the fact there was no standard protocol for nutritional care in place to prompt members of the veterinary team. To perform this evaluation Freeman et al (1998) suggest the use of a 5-point cachexia scale (where 0 = no muscle loss and 4 = severe muscle loss). An example of this type of chart, produced by the World Small Animal Veterinary Association (2013), can be seen in Figure 3. This would have been a useful monitoring tool in regards to cachexia, allowing for a consistent approach to evaluation of muscle loss at each check-up. It could also facilitate the veterinary professional in identifying any improvement or deterioration in the patient's condition.
Weight and BCS were re-evaluated at a 7-day check and subsequent monthly revisits. To provide more accurate measurements it is suggested that the weight should be recorded the same way every time (i.e. on the same scales at the same time of day), and the BCS should be performed using the same scoring system, recorded by the same veterinary professional to avoid discrepancies (Slupe et al, 2008).
While this is ideal, in veterinary medicine it may not be practical or possible for the patient to see the same clinician/VN at the same time of day, at every revisit. Therefore, it is important to keep detailed clinical notes, which will aid standardisation of check-ups. For this patient, the scales used were the same, so changes in weight could be measured reasonably accurately. The inclusion of a muscle score system at these revisits could have further improved patient monitoring.
Out-patient monitoring and continued owner support
A home care plan for the owner was devised to include the drug therapy regimen, along with advice such as exercise and patient monitoring. At this stage the VN was able to engage in a discussion with the owners in regards to their expectations of the treatment regimen and was able to offer support and advice. Hills® Vet Essentials Puppy Large Breed diet was provided and advice was given on how to encourage eating. How to follow the feeding guidelines of the prescription diet was also demonstrated. To further ensure adequate nutritional needs would be met at home, the VN could have provided the owner with a nutrition plan.
The nutritional plan could have involved calculating the K/cal requirements of the patient in a 24- hour period, converting the result into the amount of food in grams that the owner should feed at each meal. Parker (2013) describes how once an animal is at home it should be fed in accordance with its maintenance energy requirements (MER). This can be found by calculating the resting energy requirement (RER), then multiplying this by an MER activity factor (Parker, 2013) (Figure 4).
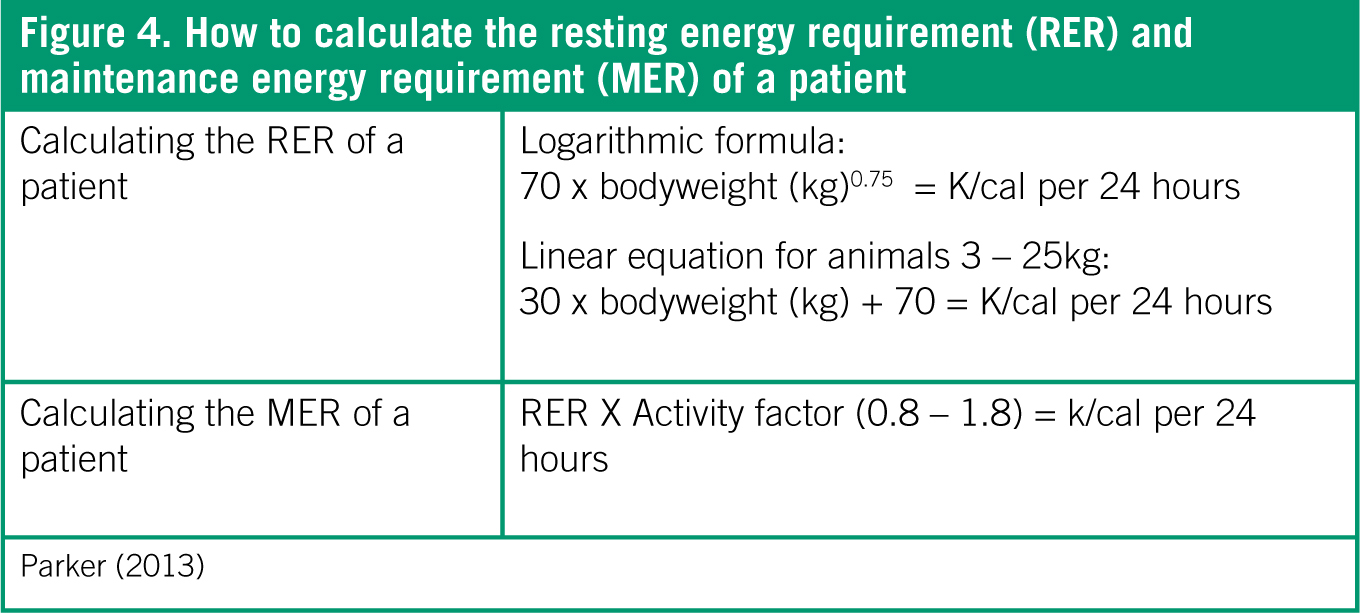
The MER activity factor is described by Parker (2013) as ranging from 0.8–1.8 for the adult dog, depending on its level of activity. It is important that the nutrition plan is regularly revisited and adjusted to maintain the animal's bodyweight and body condition (Parker, 2013). To ensure this happens the VN could keep in contact with the owner via telephone or email to offer advice and support.
Demonstration on how to record the patient's resting RR was provided and advice on possible side effects of drugs (e.g. polydipsia/polyuria from furosemide administration) was given. The owner was instructed to monitor demeanour, appetite, drinking and elimination. Exercise restriction is often suggested for patients with cardiovascular disease (Polton and Branscombe, 2008). However, Freeman (2012) reports that in people with cachexia exercise was effective at maintaining muscle mass and suggests that developing methods of resistance training for dogs with cachexia may be beneficial. Even though this may be suggested, exercise restriction was advised for this patient due to the presence of CHF.
Finally, it is important for the VN to advise owners that quality of life is the most important consideration in patients with heart disease, regardless of its severity (Pace, 2014). As suggested by Jenkins and Pace (2012) and Pace (2014) the owners were made aware that therapeutic management and patient monitoring were the key to adequate control of clinical signs.
Future recommendations
As heart disease and heart failure is such a common finding in small animal practice, the author suggests that assigning dedicated nurses to these patients could standardise the care given. In human nursing, cardiac nurse practitioners exist to provide specialist nursing care to patients with heart disease and heart failure (University Hospital Southampton NHS, 2014). This type of nursing role exists in small animal practice but mainly in referral clinics.
One study found that dogs with DCM were treated in first-opinion veterinary practice up to 6 weeks prior to referral to a veterinary specialist, of which 65% had concurrent heart failure (Martin et al, 2009). This indicates that many patients with advanced heart disease will be initially seen by firstopinion veterinary professionals.
As with the National Health Service, if dedicated cardiac VNs were readily available in first-opinion practice, it may help with the continued patient and owner care associated with heart failure in routine nurse clinics. However, having VNs dedicated to one discipline may be considered impractical in general practice due to time and staff constraints.
One suggestion could be that each individual practice reviews, if necessary, their current practice for these patients. This could help identify any areas where further training may be needed or aid in highlighting any areas of improvement. This may also help practices to recognise particular areas of interest for their VNs, such as nursing the cardiac patient, which could not only enhance job satisfaction but also improve both client and patient care.
Conclusion
DCM is the most commonly seen form of acquired heart disease in large breed dogs. Progression of this disease can lead to CHF and complications such as cachexia. VNs should be familiar with the drugs used for cardiac conditions and should be able to identify preferred methods of administration. Understanding the nutritional requirements and potential issues associated with weight and muscle loss is a vital aspect of the VN's role. The ability of the VN to communicate effectively with the owners can optimise patient care and enhance quality of life for the patient.
Key Points
- Dilated cardiomyopathy is the most common form of acquired myocardial disease in dogs.
- Poor body condition score and distinct loss of fat and overall muscle mass are characteristics of cachexia, which is related to the poor prognosis in congestive heart failure patients.
- Nutritional therapy for cardiac patients can be difficult as recommendations can vary.
- It is important for the VN to advise owners that quality of life is the most important consideration in patients with heart disease, regardless of its severity.


